Is One Medication Better Than Another
In recent years, many new medicines for treating type 2 diabetes have been developed.
According to international guidelines, patients should take metformin as their first-line type 2 diabetes treatment unless there is a medical reason that it should not be prescribed.
However, various factors should be taken into account when choosing a ‘second-line’ medication to add to metformin. You can find out more about the individual medicines later in this leaflet.
- If it is important to avoid low blood glucose – DPP-4 inhibitor, SGLT-2 inhibitor, pioglitazone or GLP-1 mimetic.
- For people with a history of heart attack, stroke, etc – SGLT-2 inhibitor or GLP-1 mimetic with proven heart benefit.
- For people with a history of heart failure or chronic kidney disease – SGLT-2 inhibitor or, if not suitable, GLP-1 mimetic.
- For people where weight loss or avoiding weight gain is important – SGLT-2 inhibitor or GLP-1 mimetic .
- In the UK, the National Institute for Health and Care Excellence recommends that with some exceptions, GLP-1 mimetics should only be prescribed for people with a body mass index over 35.
When To Start Insulin
Insulin is usually started when oral medicines and lifestyle changes have failed to lower a persons HbA1c level to less than 7%. However, a recent consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes suggested that insulin is a reasonable choice if a persons HbA1c level remains above 7% while he is taking metformin alone.
Type 2 Diabetes And Insulin
Getting Started
When most people find out they have Type 2 diabetes, they are first instructed to make changes in their diet and lifestyle. These changes, which are likely to include routine exercise, more nutritious food choices, and often a lower calorie intake, are crucial to managing diabetes and may successfully lower blood glucose levels to an acceptable level. If they do not, a drug such as glyburide, glipizide, or metformin is often prescribed. But lifestyle changes and oral drugs for Type 2 diabetes are unlikely to be permanent solutions. This is because over time, the pancreas tends to produce less and less insulin until eventually it cannot meet the bodys needs. Ultimately, insulin is the most effective treatment for Type 2 diabetes.
There are many barriers to starting insulin therapy: Often they are psychological sometimes they are physical or financial. But if insulin is begun early enough and is used appropriately, people who use it have a marked decrease in complications related to diabetes such as retinopathy , nephropathy , and neuropathy . The need for insulin should not be viewed as a personal failure, but rather as a largely inevitable part of the treatment of Type 2 diabetes. This article offers some practical guidance on starting insulin for people with Type 2 diabetes.
You May Like: Is Type 2 Diabetes Serious
How To Titrate Insulin Dosage And Monitor Progress
A major feature of this regimen is that insulin is added to existing treatment. Glycaemic control should therefore improve immediately and for practical purposes, should not deteriorate. This means that the dose of insulin can be increased relatively slowly, minimising the risk of hypoglycaemia. As described originally, the regimen2 increased the insulin dosage by 4 units a day if the fasting blood glucose exceeded 8 mmol/L on three consecutive days and by 2 units a day if it exceeded 6 mmol/L. We tend to do it slightly slower and adjust insulin dosage according to these glucose thresholds every 1-2 weeks. The slower pace helps to gain the patient’s confidence and reduces the risk of hypoglycaemia. This titration regimen is of course not ‘cast in stone’ and there are ongoing trials that are exploring the best options.
After 2-3 months, the patient is likely to be on about 30 units of insulin each day and maximum oral drug therapy. Measuring the HbA1c concentration after this interval helps to quantify the new level of glycaemic control and further increases in insulin dosage can be made accordingly. There is generally a reduction in HbA1c of about 2% and an increase in body weight of several kilograms. If these changes are not evident, one should consider the possibility that the patient has not been taking the insulin regularly or someone unfamiliar with the regimen has reduced or stopped one or more of the oral hypoglycaemic drugs.
Your Doctor Might Prescribe Other Injectable Medication
Insulin isnt the only type of injectable medication used to treat type 2 diabetes. In some cases, your doctor might prescribe other injectable medications.
For example, medications such as GLP-1 receptor agonists and amylin analogues need to be injected. These types of medications both work to keep your blood glucose levels within a normal range, particularly after meals.
Depending on the specific medication, you might need to inject it daily or weekly. If your doctor prescribes an injectable medication, ask them when and how to take it. They can help you learn how to safely inject the medication and dispose of used needles.
You May Like: Best Cookbook For Type 1 Diabetes
Choice Of Insulin Regimen: The Combined Oral Drug And Insulin Approach
Many patients and practitioners procrastinate as insulin treatment is erroneously considered to be risky and difficult. However, the regimen used routinely in our clinic is safe and easy to start.2 In our opinion this regimen can be started in general practice. The regimen consists of a combination of intermediate-acting insulin before bed, while continuing maximum oral drug therapy during the day.
How Should Insulin Therapy Be Intensified
The available options for additional insulin injections include a second injection of basal insulin, prandial insulin before one or more meals, or a switch to biphasic insulin. The choice between intensification of basal insulin versus the introduction of prandial or biphasic insulin should be individualized based on patients’ diurnal blood glucose profiles. When considering the profiles obtained with NPH insulin or long-acting insulin analog once daily, the effect appears to wane during the day, even in patients starting insulin therapy, i.e., with remaining endogenous insulin secretion . These patients could benefit from adding a second injection of basal insulin . However, in the context of declining endogenous insulin secretion, daytime hyperglycemia is usually related to elevated postprandial glucose levels, favoring the initiation of prandial or biphasic insulin.
Don’t Miss: Cinnamon For Diabetes Type 2
Foods And Beverages To Limit
If youve been diagnosed with type 2 diabetes, or even if youre trying to avoid diabetes and manage your weight, there are certain foods and beverages that you should limit if possible. These include:
- foods heavy in saturated or trans fats
- refined baked goods
- high-sugar, highly processed snacks
- sugary drinks
While no one food, enjoyed every so often, should knock you off your healthy path, its a good idea to talk with your doctor about dietary restrictions based on your blood sugar levels. Some people may need to monitor their glucose more carefully than others after eating these foods.
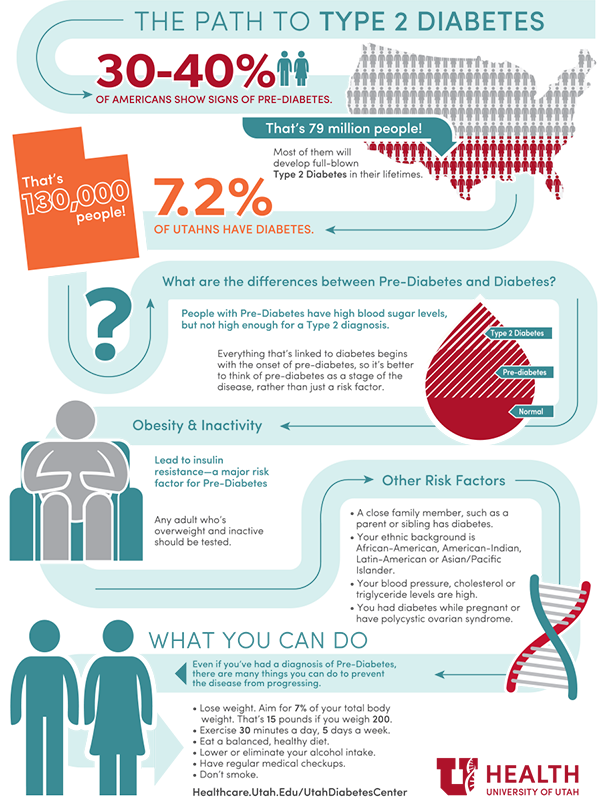
Type 2 Diabetes Risk Factors
Certain things make it more likely that youâll get type 2 diabetes. The more of these that apply to you, the higher your chances of getting it are. Some things are related to who you are:
- Age. 45 or older
- Family. A parent, sister, or brother with diabetes
- Ethnicity. African American, Alaska Native, Native American, Asian American, Hispanic or Latino, or Pacific Islander American
Risk factors related to your health and medical history include:
- Prediabetes
- Sleeping too little or too much
You May Like: 504 Accommodation Plan For Type 1 Diabetes
Glycemic Control And Daily Insulin Requirement
In the short-term active treatment phase, plasma glucose values obtained with home monitoring decreased significantly more in the metformin group than in the placebo group . The mean daily glucose level decreased from 8.8 ± 2.1 to 8.5 ± 1.7 mmol/l in the placebo group and from 8.8 ± 2.2 to 7.8 ± 1.7 mmol/l in the metformin group . The mean daily glucose level decreased 0.7 mmol/l more in the metformin group than in the placebo group.
Changes in GHb and daily dose of insulin are shown in . Mean GHb level decreased from 7.9 ± 1.2 to 7.6 ± 1.2% in the placebo group and from 7.9 ± 1.2 to 6.9 ± 1.0% in the metformin group . Mean GHb levels decreased 0.6% point more in the metformin than in the placebo group . The difference in GHb levels between the metformin and placebo groups was similar in each of the three centers . The daily dose of insulin increased 1.4 IU in the placebo group and decreased 7.2 IU in the metformin group .
Type 2 Diabetes Complications
Over time, high blood sugar can damage and cause problems with your:
- Heart and blood vessels. Youâre up to five times more likely to get heart disease or have a stroke. Youâre also at high risk of blocked blood vessels and chest pain .
- Kidneys. If your kidneys are damaged or you have kidney failure, you could need dialysis or a kidney replacement.
- Eyes. High blood sugar can damage the tiny blood vessels in the backs of your eyes . If this isnât treated, it can cause blindness.
- Nerves. This can lead to trouble with digestion, the feeling in your feet, and your sexual response.
- Skin. Your blood doesnât circulate as well, so wounds heal slower and can become infected.
- Pregnancy. Women with diabetes are more likely to have a miscarriage, a stillbirth, or a baby with a birth defect.
- Sleep. You might develop sleep apnea, a condition in which your breathing stops and starts while you sleep.
- Hearing. Youâre more likely to have hearing problems, but itâs not clear why.
- Brain. High blood sugar can damage your brain and might put you at higher risk of Alzheimerâs disease.
- Depression. People with the disease are twice as likely to get depressed as people who donât have it.
The best way to avoid these complications is to manage your type 2 diabetes well.
- Take your diabetes medications or insulin on time.
- Eat right, and don’t skip meals.
- See your doctor regularly to check for early signs of trouble.
Don’t Miss: What Is Type Ii Diabetes
The Advantages Of The Combined Oral Drug And Insulin Regimen
The literature often addresses the question of whether combined oral drug and insulin treatment provides better glycaemic control than insulin alone. This is in a sense a meaningless question because the answer would depend on how much insulin was used. We favour the combined regimen because glycaemic control begins to improve from the day insulin is started. The titration of insulin dosage can be gradual and therefore relatively safe, in an outpatient setting.
The alternative is to stop the oral drugs abruptly. In this scenario, insulin needs to be given at least twice daily and the dose needs to be quickly titrated upward to 70-80 units per day, or glycaemic control may actually deteriorate. This ‘insulin alone’ regimen is obviously possible, but requires more patient contact, making it less user-friendly for both doctors and patients. All too commonly, we have witnessed deterioration in glycaemic control when both oral drugs were stopped and not replaced with sufficient insulin.
In our experience, it is easier to persuade patients to undertake combined oral drugs and insulin treatment. They are often comforted by the knowledge that they only need to take insulin once, in the privacy of their own home and without a great deal of disturbance to their daytime routine. When they are familiar with insulin injections they become accepting of a more intensive insulin regimen, should this be required.
Advanced Glycation End Products
Food-derived, pro-oxidant, advanced glycation end products may contribute to insulin resistance in clinical type 2 diabetes mellitus and may suppress protective mechanisms. Advanced glycation end-product restriction may preserve native defenses and insulin sensitivity by maintaining a lower basal oxidative state.
Don’t Miss: When Are You Diagnosed With Type 2 Diabetes
Healthy Eating For Type 2 Diabetes
A dietitian or your doctor will be able to advise you on what to eat to meet your nutritional needs and control your blood sugar. Your doctor should be able to refer you to a registered dietitian for personalised advice.
Eating healthy foods with a low glycaemic index can help to optimise your blood sugar levels. This includes wholegrain breads, minimally processed breakfast cereals like rolled or steel cut oats, legumes, fruit, pasta and dairy products.
Avoid high-carbohydrate, low-nutrient foods such as cakes, lollies and soft drinks, and eat a diet low in saturated fat.
You should eat at regular times of the day and may also need snacks. Try to match the amount of food you eat with the amount of activity you do, so that you dont put on weight.
If you are overweight or obese, losing even 5-10 per cent of your body weight can significantly improve blood sugar control.
Do I Have Other Treatment Options For My Diabetes
When medicines and lifestyle changes are not enough to manage your diabetes, a less common treatment may be an option. Other treatments include bariatric surgery for certain people with type 1 or type 2 diabetes, and an “artificial pancreas” and pancreatic islet transplantation for some people with type 1 diabetes.
Recommended Reading: What Is The Earliest Sign Of Diabetes Nephropathy
What Happens If You Avoid Taking Your Insulin
If you have type 1 diabetes, taking insulin is essential and you cannot live without it. If you avoid taking it, your blood sugar levels can become too high and you risk developing diabetic ketoacidosis . If left untreated, DKA could be life-threatening. Thats why its important to make sure you take your insulin.
If you have type 2 diabetes and use insulin to treat your condition, you should continue to take it as prescribed. If you avoid taking it, your blood sugar levels could become too high and you may become ill. Please speak to your healthcare professional if you have any questions or concerns about taking your insulin.
Insulin is a treatment that helps manage blood sugars, so this also reduces the risk of serious long-term complications as well a shorter-term consequences. Its still important to keep going to your appointments and manage your condition with healthy lifestyle choices. Staying active and eating a healthy diet will reduce the risk of complications from your diabetes, but insulin is also an important part of your treatment.
Situations When Type 2 Diabetics Must Go On Insulin
Few things are more worrisome for diabetics than when type 2diabetes needs insulin. Some doctors even use insulin as a scare tactic.
But the truth is, sometimes insulin therapy is really theonly way to go. Most of the time insulin is associated with worsened diabetesor the end of the road. But hopefully after you finish reading, youll feelmore confident that insulin is not the end and you can still regain yourhealth.
Insulin is indicated when blood sugar control cant beachieved with diet, exercise, and oral drugs for people with type 2 diabetes.
There are 3 main situations when insulin is usually used forpeople with type 2 diabetes. They are as follows:
Early Initiation ofInsulin in Type 2 Diabetes
For most newly diagnosed or people who havent had diabetesfor very long, their doctor will put them on oral medications and a diet andexercise regimen. The goal is to get these three to work in getting blood sugarlevels under control.
But when a type 2 diabetic presents with weight loss, moresevere symptoms and blood sugar levels greater than 250 mg/dL patients arestarted early on insulin therapy.
Late-Stage InsulinTherapy in Type 2 Diabetes
When MedicalSituations in Type 2 Diabetes Require Insulin
Recommended Reading: High Blood Sugar And Insulin
Why You May Need To Take Insulin
What impacts your need for insulin differs from person-to-person, Dr. Levy says. So, its important to understand what places you at-risk for diabetes complications. The higher your risk, the more you may potentially need to include insulin in your treatment plan. These risk factors include:
But if you dont fall into one of these risk groups, there may be ways that you can avoid taking insulin with certain lifestyle modifications.
What Should A Type 2 Diabetes Meal Plan Include
Ask your healthcare provider or a nutritionist to recommend a meal plan thats right for you. In general, a Type 2 diabetes meal plans should include:
- Lean proteins: Proteins low in saturated fats include chicken, eggs and seafood. Plant-based proteins include tofu, nuts and beans.
- Minimally processed carbohydrates: Refined carbs like white bread, pasta and potatoes can cause your blood sugar to increase quickly. Choose carbs that cause a more gradual blood sugar increase such as whole grains like oatmeal, brown rice and whole-grain pasta.
- No added salt: Too much sodium, or salt, can increase your blood pressure. Lower your sodium by avoiding processed foods like those that come in cans or packages. Choose salt-free spices and use healthy oils instead of salad dressing.
- No added sugars: Avoid sugary foods and drinks, such as pies, cakes and soda. Choose water or unsweetened tea to drink.
- Non-starchy vegetables: These vegetables are lower in carbohydrates, so they dont cause blood sugar spikes. Examples include broccoli, carrots and cauliflower.
Read Also: How To Gain Weight With Diabetes
Receiving A Type 2 Diabetes Diagnosis
Whether or not you have prediabetes, you should see your doctor right away if you think you may be experiencing symptoms of diabetes. Your doctor can get a lot of information from blood work. Diagnostic testing may include the following:
- Hemoglobin A1C test.This test measures average blood glucose levels for the previous 2 or 3 months. You dont need to fast for this test, and your doctor can diagnose you based on the results. Its also called a glycosylated hemoglobin test.
- Fasting plasma glucose test. This test measures how much glucose is in your plasma. You may need to fast for 8 hours before taking it.
- Oral glucose tolerance test. During this test, your blood is drawn three times: before, 1 hour after, and 2 hours after you drink a dose of glucose. The test results show how well your body deals with glucose before and after the drink.
If you have diabetes, your doctor will provide you with information about how to manage the disease, including:
- how to monitor blood glucose levels on your own
- dietary recommendations
- physical activity recommendations
- information about any medications that you need
You may need to see an endocrinologist who specializes in the treatment of diabetes. Youll probably need to visit your doctor more often at first to make sure your treatment plan is working.