Treating Type 1 Diabetes
It’s important that diabetes is diagnosed as early as possible. If left untreated, type-1 diabetes is a life-threatening condition. It’s essential that treatment is started early.
Diabetes can’t be cured, but treatment aims to keep your blood glucose levels as normal as possible and control your symptoms, to prevent health problems developing later in life.
If you’re diagnosed with diabetes, you’ll be referred to a diabetes care team for specialist treatment and monitoring.
As your body can’t produce insulin, you’ll need regular insulin injections to keep your glucose levels normal. You’ll be taught how to do this and how to match the insulin you inject to the food you eat, taking into account your blood glucose level and how much exercise you do.
Insulin injections come in several different forms, with each working slightly differently. You’ll most likely need a combination of different insulin preparations.
Insulin is given to some patients by a continuous infusion of fast acting insulin . This is where a small device constantly pumps insulin into your bloodstream through a plastic tube that’s inserted under the skin with a needle.
There are alternatives to insulin injections and pumps, but they’re only suitable for a small number of patients. They are:
Read more about diagnosing diabetes and treating type 1 diabetes
What We’re Doing To Get Us There Sooner
We set up the Type 1 diabetes Immunotherapy Consortium in 2015, with an investment of £2.8 million and co-funding from JDRF. Its goal is to bring scientists together to speed up the clinical trial process and make the first immunotherapy available to people with type 1 diabetes as soon as possible.
Were also funding research to further unravel what happens to the immune system in people with type 1 diabetes, so scientists can find new and better therapies.
Professor Marelli-Berg is testing if an existing drug could help Tregs work better and protect beta cells.
Professor Susan Wong is looking at a protein found on B cells to figure out whether changes in its levels could play a role in the type 1 immune attack.
Dr Parth Nardendran is trying to identify the exact regions on beta cells that killer T cells recognise.
Box 3 Evidence Supporting A Role For
-
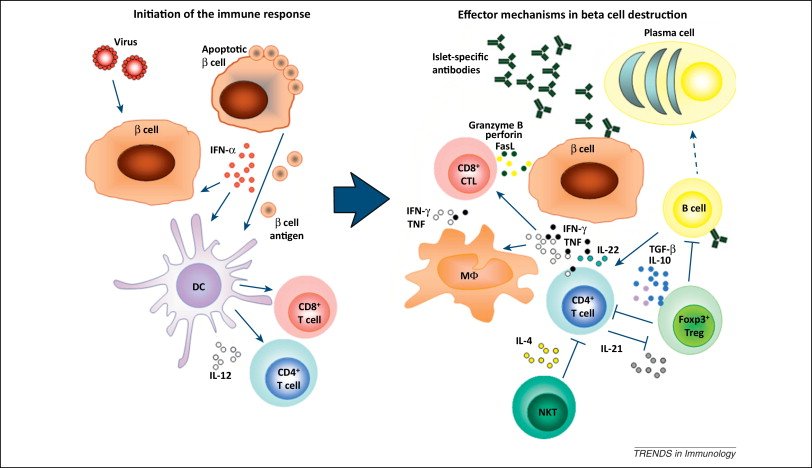
Smaller size of pancreas and islet mass in patients with type 1 diabetes mellitus and individuals at risk
Studies of human insulitis have revealed that danger signals from stressed -cells might precede insulitis. Among these signals, hyper-expression of HLA class I was noted across pancreata from patients with newly diagnosed T1DM. In addition, islets secrete the chemokine CXCL10, attracting leukocytes expressing its receptor CXCR3 to the lesion. This chemokine production by stressed -cells might present a master switch of islet inflammation and has attracted interest from the pharmaceutical industry as an opportunity for intervention therapy. Other strategies include efforts to reduce -cell stress with verapamil, where early studies have shown promise for delaying T1DM disease progression. Intriguingly, high levels of insulin-specific autoreactive human T cells only precipitated insulitis and selective -cell destruction in humanized mice in vivo after the mice had been vaccinated with insulin peptide to prime an autoimmune response and subjected to low-dose streptozotocin to stress the -cells. This finding underscores the need for -cell perturbation and loss of autoimmune tolerance to -cells to create a perfect storm that causes their destruction.
You May Like: How Many People In The Us Have Type 1 Diabetes
Does Diabetes Affect The Immune System
Both Type 1 and Type 2 diabetes affect millions of people around the world, although many who suffer from it have not been officially diagnosed with the disease. The most common warning signs of diabetes have become widely publicized in recent years. They include excessive thirst, general fatigue, blurred vision, numbness in the extremities and changes in personality.
However, there is another side effect of diabetes that can lead to serious health problems left unchecked. A number of undiagnosed or under-treated diabetics can also have compromised immune systems as a result of the changes in blood chemistry and the nervous system. This isnt the same process as a cancer patient losing all immunity due to strong chemotherapy, but more of a reduction of the bodys natural immune reaction.
But it is important to understand that not all diabetics, regardless of type, have compromised immune systems, and they are not noticeably more vulnerable to opportunistic infections, such as influenza or a common cold. The effects of uncontrolled hyperglycemia tend to target a fragile diabetics skin, urinary tract, kidneys and eyes.
Impairment Of Cytokine Production
Unlike the effect of hyperglycemia on immune cell activity in T2D, the impact of insulin deficiency in T2D on macrophage activity against pathogens has not been widely studied. A study regarding the impact of insulin deficiency on immune response by Tessaro et al. demonstrated that the administration of insulin into bone marrow-derived macrophages isolated from diabetic mice significantly increased the production of TNF- and IL-6 after LPS stimulation . Another study using rats revealed that a lack of insulin resulted in a disruption in phagocytosis of alveolar macrophages as well as cytokine release, both of which were restored after insulin intervention . Since TNF- and IL-6 play a role in leukocyte function against pathogens, this result indicated that the administration of exogenous insulin in diabetes may enhance immune cell activity to protect against pathogens.
Recommended Reading: Nursing Care Plan For Diabetes
Do I Have Other Treatment Options For My Type 1 Diabetes
The National Institute of Diabetes and Digestive and Kidney Diseases has played an important role in developing artificial pancreas technology. An artificial pancreas replaces manual blood glucose testing and the use of insulin shots. A single system monitors blood glucose levels around the clock and provides insulin or a combination of insulin and glucagon automatically. The system can also be monitored remotely, for example by parents or medical staff.
In 2016, the U.S. Food and Drug Administration approved a type of artificial pancreas system called a hybrid closed-loop system. This system tests your glucose level every 5 minutes throughout the day and night through a continuous glucose monitor, and automatically gives you the right amount of basal insulin, a long-acting insulin, through a separate insulin pump. You still need to manually adjust the amount of insulin the pump delivers at mealtimes and when you need a correction dose. You also will need to test your blood with a glucose meter several times a day. Talk with your health care provider about whether this system might be right for you.
The illustration below shows the parts of a type of artificial pancreas system.
Starting in late 2016 and early 2017, the NIDDK has funded several important studies on different types of artificial pancreas devices to better help people with type 1 diabetes manage their disease. The devices may also help people with type 2 diabetes and gestational diabetes.
Box 2 Observations Inconsistent With T Cells As A Driving Force In T1dm
-
Islet-specific autoreactive T cells in the healthy population,,,
-
No development of insulitis or selective loss of -cells in humanized mice transduced with islet antigens specific T cell receptor and immunized with islet antigen
-
No development of autoimmune diabetes mellitus in HLA class II transgenic mice immunized with islet autoantigens,
-
No development of type 1 diabetes mellitus in pancreatitis, even with high risk HLA
-
No lasting effect of immunotherapy on preservation of -cell function,,,
-
Most patients with cancer who are treated with co-stimulation blockade never develop T1DM,
-
Most patients with T1DM do not display abnormalities in immune regulation
-
HLA class I upregulation without islet inflammation,
-
Paucity of insulitis in individuals with islet autoantibodies
-
Limited rate of insulitis at diagnosis of T1DM, even with more widespread -cell stress,
-
Immunization with islet autoantigens does not cause T1DM,,,
You May Like: Normal Glucose Range For Diabetics
Allergies Are Also An Immune System Mistake
If youve ever been to see a doctor who specializes in allergies, you may have noticed a sign on the door: Allergy and Immunology. Yup, they go hand-in-hand.
For some reason, in people with allergies, the immune system strongly reacts to an allergen that should be ignored. The allergen might be a certain food, or a certain type of pollen, or a certain type of animal fur. For example, a person allergic to a certain pollen will get a runny nose, watery eyes, sneezing, etc., Joslins Dr. Jackson tells DiabetesMine.
People with one autoimmune condition can be prone to getting a second one too. In the case of T1D, that second is often thyroid disease, or, you guessed it an
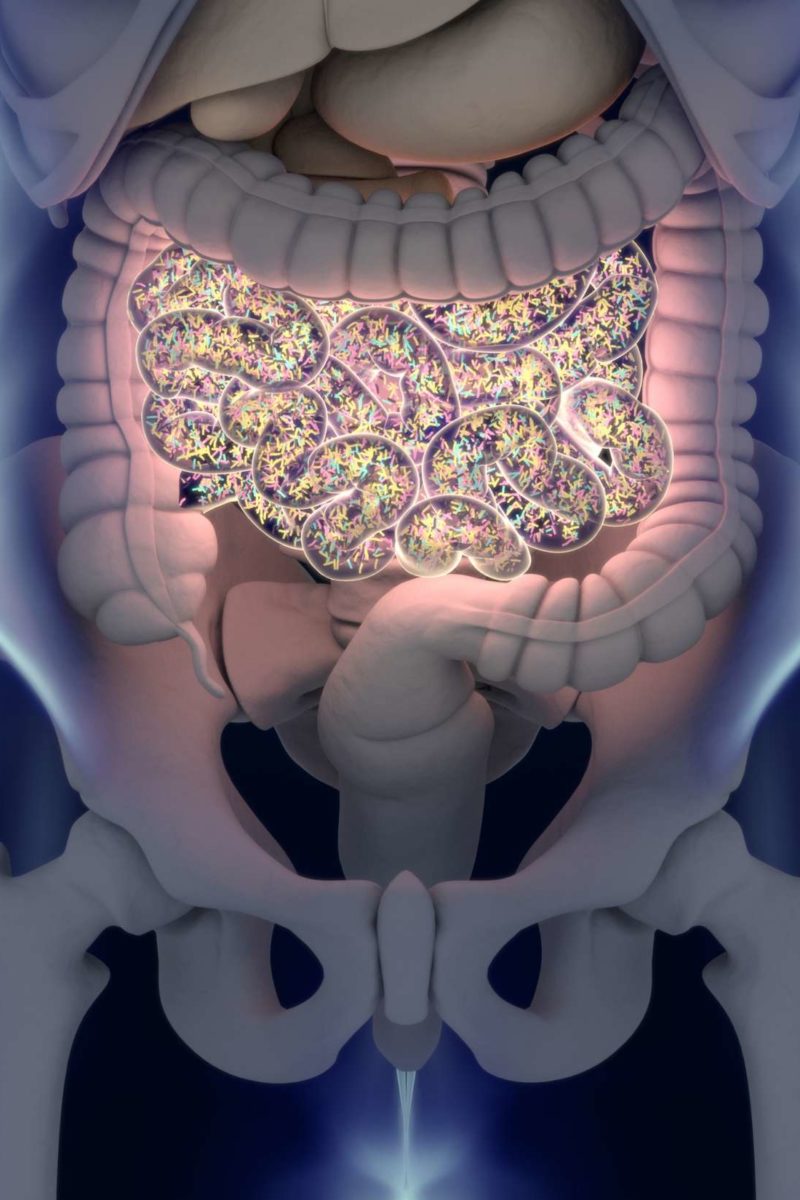
Teaming Up With Bacteria
The bacteria in our gut have a strong connection with our immune system. ActoBio, a company based in Belgium, wants to exploit this connection to treat type 1 diabetes. Our product candidates are based on the use of Lactococcus lactis bacteria that are genetically modified to express proteins, peptides, antibodies or human cytokines, Lothar Steidler, CTO of ActoBio, told me.
Our guts are familiar to this bacterium, as its used to produce cheese and buttermilk. In the case of type 1 diabetes, the bacteria are engineered to produce the insulin precursor human proinsulin and a signaling molecule called interleukin 10. Together they signal the gut-associated lymphoid tissue, where immune cells are stored, to restore the tolerance of insulin-producing cells with the goal of slowing down or stopping their destruction.
It is potentially a safe oral treatment that will be given for a limited period of time and could lead to patients who develop type 1 diabetes not needing to use insulin, or delay the need for insulin after diagnosis added Pieter Rottiers, CEO of ActoBio.
The company is now running a phase I/II clinical trial in the US and Europe in people with type 1 diabetes as young as 12 years old. Patients will have to have some remaining capacity for production of insulin, said Rottiers. Results are expected this year.
Also Check: What Should My Sugar Level Be With Type 2 Diabetes
Type 1 Diabetes With Other Autoimmune Diseases
Editors Note: This content has been verified by Marina Basina, MD, a Clinical Associate Professor at Stanford University. Shes a clinical endocrinologist and researcher with a focus on diabetes management and diabetes technology. Dr. Basina is an active member of multiple medical advisory boards and community diabetes organizations, and she is on the Beyond Type 1 Science Advisory Council.
People with Type 1 diabetes, an autoimmune disease, are more likely to have a co-occurring autoimmune disorder. An autoimmune disease means that your immune system sees your bodys own tissue as foreign invaders and attacks itself. For example, if you have Type 1, your body mistakenly attacks the insulin-producing cells in your body. The reason that co-occurring autoimmune disorders are so common isnt exactly known, although we do know that genetics play a significant role.
Because we know that having Type 1 puts you at a higher risk of developing other autoimmune diseases, its important to be aware of what the signs and symptoms are. The following are warning signs that are common for all autoimmune diseases, including Type 1:
- Fever
Quick Tips For Helping Increase Your Immunity
The following are quick tips to help you increase your immune system response if you have diabetes. Follow these tips for a healthier you with less colds, viruses and nasty microbes to fight off in your system.
As you age, your immune system response can become slow. When you have diabetes, this is doubly true.
- Get enough exercise
- Get the right amount of sleep
- Eat the right portions of carbohydrates, proteins, fats
- Stop any bad habits such as smoking and drinking alcohol
- Managing your stress levels can also play a big role
Don’t Miss: Does One High A1c Mean Diabetes
When To See A Doctor
Visit your GP as soon as possible if you experience the main symptoms of diabetes, which include:
- weight loss and loss of muscle bulk
- itching around the penis or vagina, or frequent episodes of thrush
- cuts or wounds that heal slowly
- blurred vision
Type 1 diabetes can develop quickly over weeks or even days.
Many people have type 2 diabetes for years without realising because the early symptoms tend to be general.
Inhibition Of Antibodies And Complement Effector
The dysfunction of complement activation was observed in an animal study in rats conducted by Clifford et al. . They demonstrated that hyperglycemia was associated with decreased C4-fragment opsonization, which inhibits classical or lectin pathways of complement activation. The summary of possible mechanisms that cause infection susceptibility in people with diabetes is presented in Table and Fig. .
Also Check: How Many Carbs Should A Pre Diabetic Eat Per Day
Risk Factors For Type 1 Diabetes:
Any combination of the following factors may put people at a higher risk for type 1 diabetes:
- Self-allergy : The immune system usually protects us from disease, but in the case of type 1 diabetes, the immune system turns against the cells in the pancreas that produce insulin . If you have any type of autoimmune disease, your risk of developing diabetes increases. Doctors can test for diabetes antibodies, specifically one called GAD65. Measuring this antibody early in the disease can help your medical team determine if you have type 1 or type 2 diabetes.
- Genes: People with type 1 diabetes are more likely to have inherited genes putting them at risk. Over 50% of those diagnosed with type 1 diabetes also have a close relative with the disease.
What Stage Is The Research At
Before any new treatments can be given outside of a research setting they have to be rigorously tested in clinical trials. Scientists are doing this with different immunotherapies right now. The majority of trials are involving people who are within 100 days of their diagnosis.
But trials are also happening in people who dont yet have type 1 diabetes, but are at a high risk. We’ve recently had an exciting breakthrough in this area. A landmark trial showed that an immunotherapy could delay the diagnosis of type 1 diabetes by an average of three years. Find out more about these results.
The results of large clinical trials then need to be put to regulatory bodies who decide whether a new treatment is safe and effective, and grant it a licence. Only once an immunotherapy has been licensed can doctors can prescribe it to people with or at risk of type 1 diabetes.
Recommended Reading: How Can Diabetes Be Managed
How Else Can I Manage Type 1 Diabetes
Along with insulin and any other medicines you use, you can manage your diabetes by taking care of yourself each day. Following your diabetes meal plan, being physically active, and checking your blood glucose often are some of the ways you can take care of yourself. Work with your health care team to come up with a diabetes care plan that works for you. If you are planning a pregnancy with diabetes, try to get your blood glucose levels in your target range before you get pregnant.
What Are The Signs & Symptoms Of Type 1 Diabetes
Type 1 diabetes can come on over time or suddenly. Sometimes, kids dont have diabetes symptoms yet and the condition is discovered when blood or urine tests are done for another reason. Kids who show symptoms may:
- need to pee a lot
- start to wet the bed after having been dry at night
- be thirstier and drink more than usual
- feel tired often
- lose weight
Also Check: Does Insulin Cause Erectile Dysfunction
Researchers Find New Subpopulation Of Beta Cells
The scientists investigated the adaptive changes in beta cells that take place during the immune attack in both mouse models and in human cell culture. They used cyclophosphamide to accelerate the diabetes onset.
Herold and colleagues identified a resistant subpopulation of beta cells in 9-week-old, non-obese diabetic mice. The new subpopulation seems to develop from normal beta cells when they detect infiltration into the islet.
These new cells have a lower granularity, and they develop during the progression of type 1 diabetes.
During the development of diabetes, there are changes in beta cells so you end up with two populations of beta cells. One population is killed by the immune response. The other population seems to acquire features that render it less susceptible to killing.
Dr. Kevan Herold
The new subpopulation is also less differentiated and displays stem-like properties. Much like stem cells, they have the ability to revert to a previous stage of development that enables them to survive and continue to replicate despite the immune attack.
As the studys senior author explains, these cells duck and cover as they develop molecules that inhibit the immune response. Human beta cells were revealed to go through similar changes when the researchers cultured them together with immune cells.
Although the cells do eventually die, the authors explain, the mechanism they uncovered might account for the long-term development of type 1 diabetes.
Failing Immune System Brakes Help Explain Type 1 Diabetes In Mice
Research about the underlying autoimmune mechanisms in type 1 diabetes and potentially open up new immune system treatments for the disorder
Results of the study, published July 16 in Frontiers in Immunology, add to a growing body of research about the underlying autoimmune mechanisms in type 1 diabetes and potentially open up new immune system treatments for the disorder.
What weve shown in mice is one novel way that a strong inflammatory response can hijack the immune system and lead to chronic disease, says lead author Giorgio Raimondi, M.Sc., Ph.D., assistant professor of plastic and reconstructive surgery at the Johns Hopkins University School of Medicine.
An estimated 1.25 million people in the U.S. have type 1 diabetes, which is most often diagnosed in children and young adults and incurs more than $14 billion per year in medical costs and lost income. In those with the autoimmune disorder, the pancreas loses the ability to produce insulin, needed by the body to control blood sugar levels. The disease is treated with lifelong insulin therapy that must be precisely calibrated and delivered many times each day. Researchers believe that type 1 diabetes is caused by an interplay of genetics and environmental triggers recent evidence suggests that viral infections may set off some cases of the disease.
Raimondi says he wondered whether the role of these molecules in diabetes could teach him anything about transplant rejection.
You May Like: What Is An Insulin Pump