How To Calculate Your Carb Ratio
If you suspect that your carb ratio is off , its time to collect data in the form of blood sugar readings and do some analysis.
If you want good results you need good data, and youre the only one who can collect it. As with most other things related to diabetes, it requires work but its worth it.
I suggest following the 4 steps below for 3-5 days minimum to collect data for you or your doctor to assess whether your carb ratio is correct. If you and/or your doctor dont see any trends after 3-5 days, youll have to collect more blood sugar data.
After 3-5 days, you should have enough data to start assessing whether your carb ratio for this time of day is accurate.
When you or your doctor does the analysis, youll focus on whether your blood sugar was in your desired range before the meal and whether your blood sugar came back into your desired range within 90-120 minutes of your insulin injection.
Blood sugar in-range before the meal, but high 90-120 minutes after
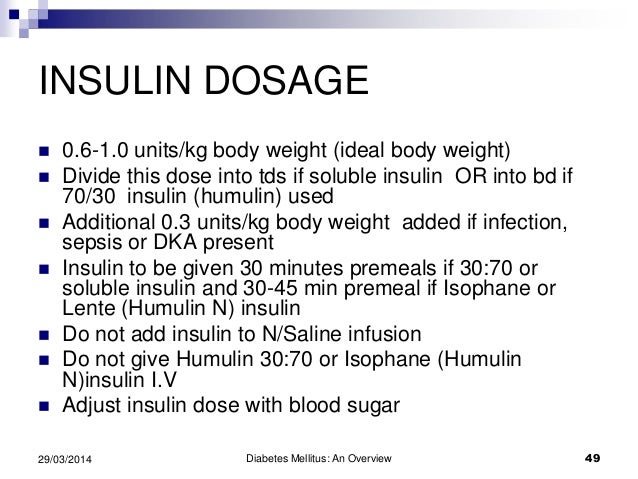
Treating Diabetes With Insulin
There are three main types of diabetes:
- Type 1 – damage to the pancreatic cells means that little to no insulin is produced.
- Type 2– insulin production is inadequate, or body cells are resistant , or both.
- Gestational diabetes – diabetes that occurs in pregnant women without a prior history of diabetes. Usually disappears after giving birth.
Insulin can be used as a treatment for all three types of diabetes. Insulin is typically given by the injection under the skin. Patients with insulin-dependent diabetes usually require some base level of insulin throughout the day , as well as some short-acting insulin to cover meals . There are many different types of insulin, and just as many different treatment strategies. Which one an individual needs should be established by a doctor. Among the strategies are conventional insulin therapy, for patients with a regular lifestyle where insulin can be given in regular, fixed doses, and intensive insulin therapy, where the patient decides on their own mealtime insulin dose, which depends on the carbohydrate content of the meal, their current blood sugar concentration, and the amount of physical activity performed.
Things To Remember In Order To Change Insulin Doses:
- If the pattern happens at the blood sugar check before breakfast, change the long-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check before lunch, change the breakfast rapid-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check 2 to 3 hours after lunch, change the lunch rapid-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check 2 to 3 hours after supper , change the supper rapid-acting insulin dose by 10 percent.
- If your blood sugar is above 180 two to three hours after a meal, ask yourself what caused this.
- Common reasons for high blood sugar 2 to 3 hours after eating are:
- Not taking insulin at least 15 minutes before eating
- Eating too much carbohydrate or too much quick-acting carbohydrate
- Not taking enough insulin to cover the carbohydrate
- Not eating protein or fat in your meal
- Eating a very high fat meal
If you rule out numbers 1 and 2, you may need to take more insulin next time.
- If the pattern is high blood sugar, you will increase the insulin dose that affects that column of blood sugars.
- If the pattern is low blood sugar, you will decrease the insulin dose that affects that column of blood sugars.
Also Check: Weekly Diet Plan For Type 2 Diabetes
How Protein And Fats Affect Carb Counting And Insulin Dosing
It is also important to know that although proteins and fats do not have a direct effect on carbohydrates, they do affect the way carbohydrates are absorbed. A food that contains carbohydrates in addition to a high protein or fat content will be absorbed more slowly but the effect will be longer, that is, it will not generate such a high glucose peak but it will last longer. You may need to adjust your ratios as you learn how various meals impact you.
If Youre Prescribed Bolus Insulin The Amount You Take Will Vary
If your doctor adds bolus insulin to your treatment plan, theyll prescribe a certain ratio of rapid-acting or regular-acting insulin to carbohydrates. This way your carb intake can be more flexible and youll adjust your mealtime insulin accordingly. Another option is to stick to a certain amount of carbs with each meal and take a fixed amount of insulin, though this approach offers less flexibility.
In other words, youll have to match the amount of bolus insulin that you take to the amount of carbohydrates that you eat. If you plan to eat a meal thats high in carbohydrates, youll need to take more bolus insulin beforehand. If you plan to eat a low-carb meal, youll take less bolus insulin beforehand.
You can also take bolus insulin to correct a high blood sugar. Your doctor will likely give you a correction factor to help you figure out how much insulin you need. This is also commonly known as a sliding scale.
Many factors affect the type and amount of basal or bolus insulin that you might need to take, including:
- how much insulin your body produces on its own
- how sensitive or resistant you are to insulin
- how many carbohydrates you eat
- how much exercise you get
- how much sleep you get
- how much you weigh
- alcohol intake
- other medications, such as steroids
Any other medications you take for type 2 diabetes can affect how your body responds to insulin therapy, too. Weight loss surgery can also affect your insulin needs.
Recommended Reading: How To Treat A Corn When Diabetic
What Is The Insulin Sensitivity Factor
The insulin sensitivity factor tells you how many points, in mg/dL, your blood sugar will drop for each unit of insulin that you take. The insulin sensitivity factor is also sometimes called a correction factor. You need to know this number to correct a blood sugar level thats too high. This is most useful for people with type 1 diabetes.
Blood Sugar Tests Help You Understand Your Insulin Needs
To learn how well your current treatment plan is working, its important to test your blood sugar according to your doctors recommendations. For example, theyll likely advise you to use home testing equipment to monitor and log your blood sugar each day. Theyll also order A1C tests, which provide information about your average blood sugar levels over the past three months.
If you find it hard to manage your blood sugar levels using your current treatment plan, talk to your doctor. They might recommend changes to your insulin regimen or other prescribed treatments.
You May Like: Can Blurry Vision From Diabetes Be Reversed
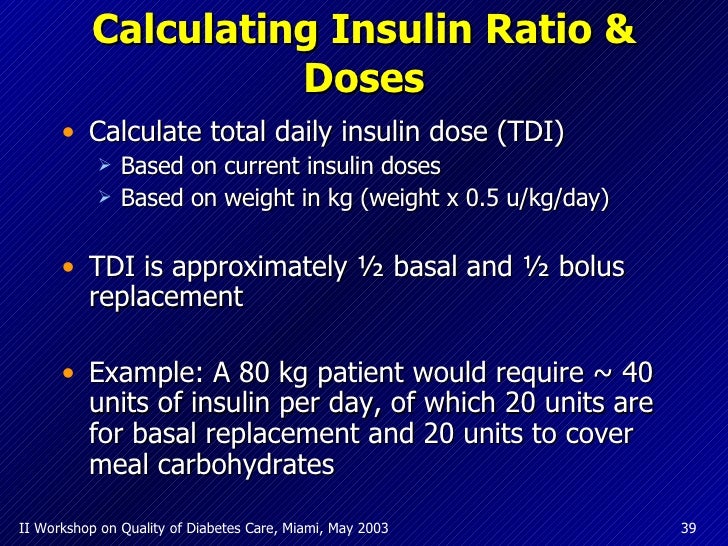
You’ll Need To Calculate Some Of Your Insulin Doses
You’ll also need to know some basic things about insulin. For example, 40-50% of the total daily insulin dose is to replace insulin overnight.
Your provider will prescribe an insulin dose regimen for you however, you still need to calculate some of your insulin doses. Your insulin dose regimen provides formulas that allow you to calculate how much bolus insulin to take at meals and snacks, or to correct high blood sugars.
Calculating Insulin Dose In Type 1 Diabetes From Diabetes Education Online
Your doctor will prescribe an insulin dosing regimen for you to get you started on your type 1 diabetes that will include the three components of intensive insulin therapy: Basal Insulin Dosage a once or twice daily dose of long acting insulin Bolus Dosage a short acting insulin dosage based on the amount of the carbohydrates in each meal . Bolus Correction Dose For A High Blood Sugar a correction factor dosage to bring your blood sugar level back to the target range when it gets too high . However, each of these three dosages can change over time or even throughout the day and you will learn how to adjust up or down each of these three components. Of course, your diabetes team should always be available by phone or internet to counsel you on an appropriate insulin dosage for any of the three components of intensive insulin therapy if youre unsure. What follows are the first three examples* from Calculating Insulin Dosage from Diabetes Education Online which will show you how you will do it: *Example #4, Formulas commonly used to create insulin dose recommendations is in the next post of my blog study notes . First, some basic things to know about insulin: Approximately 40-50% of the total daily insulin dose is to replace insulin overnight, when you are fasting and between meals. This is called background or basal insulin replacement. The basal or background insulin dose usually is constant from day to day. The other 50-6Continue reading > >
You May Like: Is Propel Water Good For Diabetics
Why Do Some People With Type 2 Diabetes Need To Take Insulin
Type 2 diabetes can progress with time, which means that it gets more difficult for a persons body to regulate glucose levels. The bodys many cells become less responsive to insulin , and the specific cells in the pancreas that produce insulin make less of it . This is not necessarily related to a persons diabetes management, and it is likely not possible to prevent.
For many people, adjusting lifestyle factors such as a reduced calorie diet and increased physical activity are key to keeping blood glucose levels stable and in a target range. Healthcare professionals may also recommend that people with type 2 diabetes take additional medications like metformin, DPP-4 inhibitors, SGLT-2 inhibitors, or GLP-1 agonists to their treatment plan to improve glucose management, reduce A1C, lose weight, or support heart and kidney health.
Where Have Current Dosing Formulas Come From
The chronological development of published insulin-dosing formulas is presented in Table Table2,2, with a detailed description of their derivation available in a recent review . Briefly, the first formula proposed in 1922, using a very crude insulin preparation, was weight based and was calculated conservatively in order to avoid hypoglycemia and to preserve the limited amount of insulin available . In 1982, Skyler et al., based upon clinical experience using buffered human regular insulin, suggested that the TBD should be about 40 % of the total daily dose .
Recommended Reading: Non Insulin Injections For Type 2 Diabetes
Example #: Carbohydrate Coverage At A Meal
First, you have to calculate the carbohydrate coverage insulin dose using this formula:
CHO insulin dose = Total grams of CHO in the meal ÷ grams of CHO disposed by 1 unit of insulin .
For Example #1, assume:
- You are going to eat 60 grams of carbohydrate for lunch
- Your Insulin: CHO ratio is 1:10
To get the CHO insulin dose, plug the numbers into the formula:
CHO insulin dose =
- The carbohydrate coverage dose is 6 units of rapid acting insulin.
- The high blood sugar correction dose is 2 units of rapid acting insulin.
Now, add the two doses together to calculate your total meal dose.
Carbohydrate coverage dose + high sugar correction dose = 8 units total meal dose!
The total lunch insulin dose is 8 units of rapid acting insulin.
Analogue Versus Human Insulin
Glucose control, adverse effects, cost, adherence, and quality of life need to be considered when choosing a type of insulin. In general, analogue insulin is similar to human insulin in controlling diabetes, although some trials have found higher mean A1C levels in patients taking analogue insulin compared with human insulin. 17 Analogue insulin usually causes less postprandial hyperglycemia and delayed hypoglycemia. 18,19 In a recent meta-analysis, glycemic control was not improved with analogue insulin compared with human insulin, but nocturnal hypoglycemia was reduced.17
An industry-funded cost-effectiveness analysis found that the increased cost of medication is more than off set by the reduction in hypoglycemic events. 20 However, the analysis assumed a cost differential of 14 percent, which is inconsistent with current pricing . 20,21 Cost-effectiveness analyses have differed regarding the long-term cost savings of using analogue insulin in patients with type 2 diabetes, with industry-sponsored studies finding reduced cost22 and government-sponsored studies finding no cost reduction. 23 Measures of adherence and quality of life have been improved with analogue insulin compared with human insulin. 24,25
You May Like: Can You Get Insulin For Free
How Have Existing Guidelines Embraced This New Information
Very little new empirical research focusing on insulin dosing in CSII in T1D has been published since the King and Kuroda studies described earlier . Nevertheless, one retrospective study of 170 pump-treated patients with T1D from Spain that focused on establishing the CIR found that the mean CIR in the morning was 350/TDD for breakfast and 400/TDD for other meals . The TBD/TDD reported in that study was quite high, 58 %, and it was not stated whether the TBD had been set by standardized diet, intense glucose monitoring, and meal omissions.
Disadvantages Of The Sliding Scale Regimen:
- The sliding scale method does not accommodate changes in insulin needs related to snacks or to stress and activity.
- You still need to count carbohydrates.
- Sliding scales are less effective in covering a pre-meal high blood sugar, because the high blood glucose correction and food bolus cannot be split.
Recommended Reading: Normal Blood Sugar For Type 2 Diabetes
What Should Be Done In High
Accurate formulas are essential to estimate the initial insulin dose and to adjust insulin pump settings. For formulas to be accepted, we believe that they should be based on studies with the following attributes:
Example To Calculate Insulin Dosage Level:
A person weighs 65 kg, his height is 150m and his fasting blood glucose level is 50mmol/L. Calculate the total number of insulin units needed each day for that person.
- Weight = 65 kg
- Fasting Blood Glucose level = 50mmol/L
Solution:
Let us find out the diabetes mellitus type 2 level of a person from the given values. Substitute the values in the formula,
Initial dose =
= *fbg / -height= *50 / ]-150= -150
Read Also: Free Diabetic Meter And Test Strips
The General Principles Of Sliding Scale Therapy Are:
- The amount of carbohydrate to be eaten at each meal is pre-set.
- The basal insulin dose doesnt change. You take the same long-acting insulin dose no matter what the blood glucose level.
- The bolus insulin is based on the blood sugar level before the meal or at bedtime
- Pre-mixed insulin doses are based on the blood sugar level before the meal
How Do You Determine Insulin Dosage
Once you know how sensitive you are to insulin, you can figure out how much insulin you need to give yourself to lower your blood sugar by a certain amount.
For example, if your blood sugar is 200 mg/dL and youd like to use your short-acting insulin to lower it to 125 mg/dL, youd need your blood sugar to drop by 75 mg/dL.
From the insulin sensitivity factor calculation, you know that your short-acting insulin sensitivity factor is 1:60. In other words, one unit of short-acting insulin lowers your blood sugar by about 60 mg/dL.
How much insulin do you then need to lower your blood sugar by 75 mg/dL?
Youll need to divide the number of mg/dL you want to lower, which is 75, by the number from your insulin sensitivity factor calculation, which is 60. The answer of 1.25 tells you that you need to take 1.25 units of short-acting insulin to lower your blood sugar by 75 mg/dL.
These are rough calculations that are used by people with type 1 diabetes. If you have type 2 diabetes, youll need to check with your doctor for guidance.
Read Also: Type One Diabetes Side Effects
Using Insulin With Oral Medications
Many oral medications are safe and effective when combined with insulin therapy. To maximize benefit without causing significant adverse effects, it is important to consider the mechanism of action for different therapies.
Insulin sensitizers have been proven safe and effective when combined with insulin therapy. 36,37 Metformin is usually continued indefinitely after the patient starts insulin therapy because it reduces cardiovascular risk in overweight patients with type 2 diabetes.12 Metformin combined with insulin is also associated with decreased weight gain, a lower insulin dosage, and less hypoglycemia compared with insulin alone. 38 Thiazolidinediones improve insulin sensitivity but may increase weight gain, fluid retention, and risk of congestive heart failure when combined with insulin.36 Thiazolidinediones also have not been shown to reduce macrovascular complications or all-cause mortality.
Alpha-glucosidase inhibitors delay absorption of carbohydrates in the gastrointestinal tract to decrease postprandial hyperglycemia. These medications are safe and effective when combined with insulin.39
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.