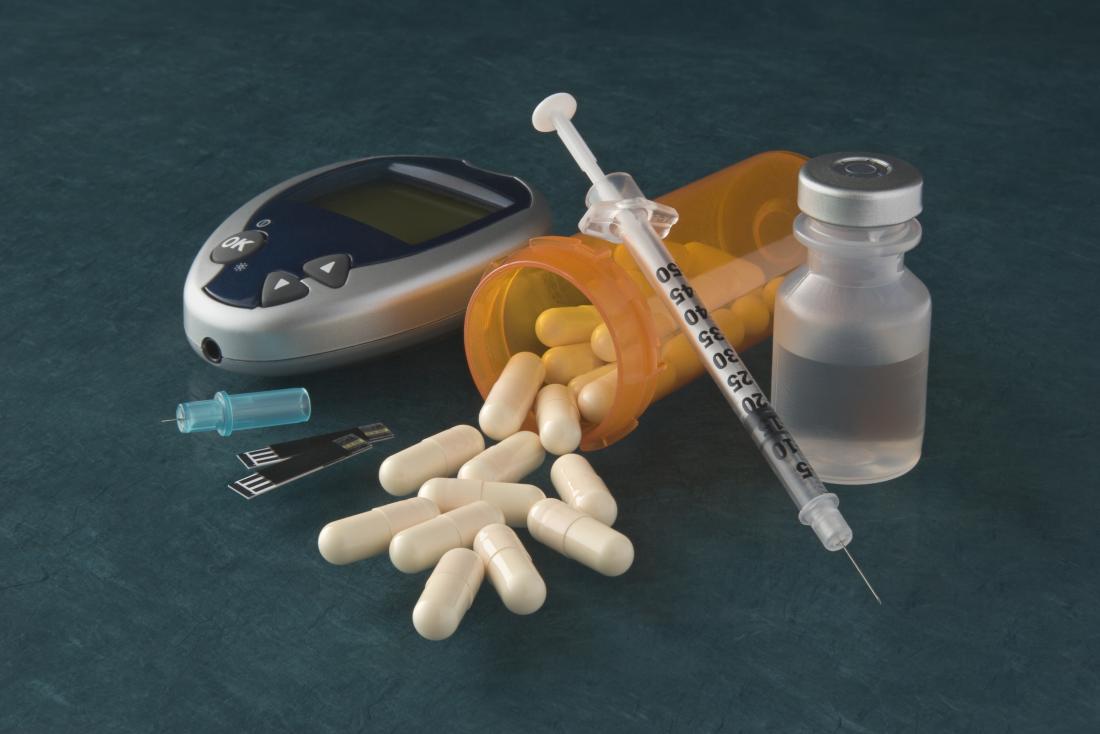
Management Of Blood Glucose With Noninsulin Therapies In Type 2 Diabetes
CHRISTA M. GEORGE, PharmD, and LUCY L. BRUIJN, MD, MPH, University of Tennessee Health Science Center, Memphis, Tennessee
KAYLEY WILL, PharmD, Texas Tech University Health Sciences Center, Abilene, Texas
AMANDA HOWARD-THOMPSON, PharmD, University of Tennessee Health Science Center, Memphis, Tennessee
Am Fam Physician. 2015 Jul 1 92:27-34.
Treatment of type 2 diabetes mellitus begins with a comprehensive and collaborative approach. The American Diabetes Association treatment guidelines focus on medical nutrition therapy, exercise, pharmacologic therapy, and the prevention and management of diabetes-related complications.1 Selected major trials that form the basis for treatment recommendations are listed in eTable A. There is no evidence demonstrating the impact on complications or mortality for the newer agents described in this article.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Metformin should be used as first-line therapy to reduce microvascular complications, assist in weight management, reduce the risk of cardiovascular events, and reduce the risk of mortality in patients with type 2 diabetes mellitus.
A = consistent, good-quality patient-oriented evidence B = inconsistent or limited-quality patient-oriented evidence C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to .
SORT: KEY RECOMMENDATIONS FOR PRACTICE
UKPDS 33A1
UKPDS 33A1
How Do I Get The Medicine Ready To Use
- Check the label. Check that you have the correct medicine. Also check the expiration date. Use a new pen if the expiration date has passed.
- Check the color of the medicine. The medicine in the cartridge should be clear, colorless, and free of particles or clumps. Use a new pen if the medicine is cloudy or has particles in it.
Assessment Of The Study Quality And Risk Of Bias
Two independent reviewers assessed the study quality and risk of bias according to the Cochrane Collaboration tool, and any controversies were resolved by mutual discussion. We considered the 6 aspects of risk of bias, including the adequacy of random sequence generation, allocation concealment, blinding of participants and personnel, completeness of outcome data, selective reporting, and other sources of bias. For the completeness of outcome data, analyses based on the intention-to-treat principle or the full analysis set were considered to be low-risk. Selective reporting was assessed as high-risk when any results were regarded as missing while some outcome variables or conditions of analysis were mentioned in the articles or when the publication was not considered as in full. Other sources of bias were assessed according to the comparability of the baseline characteristics of the participants in the trial groups.
Don’t Miss: Does Insulin Cause Erectile Dysfunction
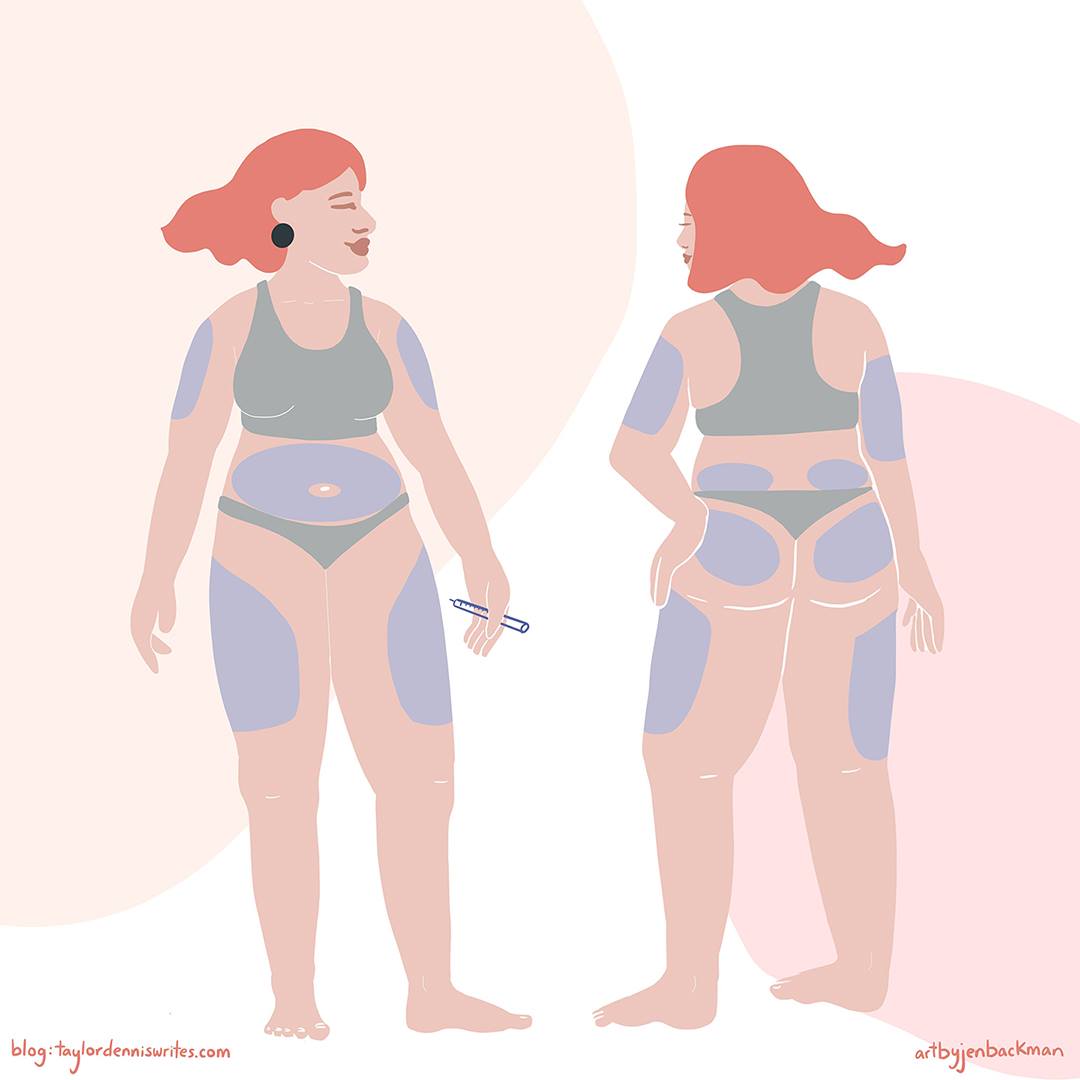
Avoiding Injection Bruises And Lumps
Bruising can happen when you catch a tiny blood vessel under the skin where you have injected. It is quite normal for this to happen occasionally when you are injecting regularly and youre not doing anything wrong.
If you are concerned, you could make an appointment with your diabetes specialist nurse who will be able to do a review of your injection technique. In some cases, bleeding and bruising can be reduced by something as simple as using a different sized needle or changing your needle after each injection.
Some people notice hard lumps that can form if you inject in the same place too often. This might be lipohypertrophy , or could be something called cutaneous amyloidosis. These lumps can stop the insulin from working properly, so make sure you rotate where you inject and choose a different spot each time. If you notice any lumps, especially if they’re not going away, speak to your healthcare professional for more advice.
Other side effects from injecting a lot can be itching, rashes and other skin irritations. Changing where you inject helps with this too. You can also get treatments from your local pharmacy that can will help with the irritation.
Choice Of Oral Agent And Weight Gain In Previously Insulin
Switching patients from treatment with insulin alone to insulin combination therapy with metformin has been associated with less weight gain in two of three studies, whereas no difference was found in any of the 16 comparisons in which insulin plus sulfonylurea was compared with insulin alone, despite better control in 10 of 16 comparisons . It is unclear whether this is because weight was not accurately recorded or because the larger dose of exogenous insulin or the greater number of insulin injections used in insulin alone as compared with the insulin combination regimen had independent weight-promoting effects. In studies comparing insulin-glitazone treatment with insulin alone, glycemic control was better in each study with the insulin-glitazone combination than with insulin alone. Better glycemic control was also associated with greater weight gain in each of the three studies. Although the amount of weight gain relative to the improvement in glycemic control seemed slightly greater than with sulfonylureas , data on insulin-glitazone combination therapy are still sparse. The significance of weight gain with glitazones is also difficult to judge, because glitazones may be beneficial in redistributing fat from visceral to subcutaneous sites . A small fraction of weight gain with glitazones could be due to peripheral edema .
Don’t Miss: How Much Does It Cost To Make Insulin
How To Manage Type 2 Diabetes
The same dietary and lifestyle strategies that can help you prevent type 2 diabetes can also help you manage and reverse insulin resistance, return to normal blood glucose levels, and reverse type 2 diabetes.
These strategies are:
- Eating a low-fat, plant-based, whole-food diet specifically designed to reverse insulin resistance permanently
- Integrating intermittent fasting into your dietary schedule
- Adding daily movement to your routine
Well go into each of these areas in detail below.
Avoiding Problems With Your Pen
Read Also: Long Acting Insulin Side Effects
Tips For Using Your Pen
Future Medications For Type 2 Diabetes
Thursday, 8 April 2021
Research is currently demonstrating great potential in the search for new medications to treat type 2 diabetes. There are several new medications for type 2 diabetes currently in development. One is a once a week insulin injection, the other is a combined insulin and GLP-1 agonist daily injection.
You May Like: How To Care For Someone With Diabetes
Type 1 Diabetes Complications
- Heart disease or heart attack
- Chronic kidney disease and kidney failure
- Damage to macrovascular and microvascular blood vessels
- Type 3 diabetes
- Coronary artery disease
- Heart disease or heart attack
- Chronic kidney disease and kidney failure
- Damage to macrovascular and microvascular blood vessels
- Type 3 diabetes
- Coronary artery disease
What Happens If You Avoid Taking Your Insulin
If you have type 1 diabetes, taking insulin is essential and you cannot live without it. If you avoid taking it, your blood sugar levels can become too high and you risk developing diabetic ketoacidosis . If left untreated, DKA could be life-threatening. Thats why its important to make sure you take your insulin.
If you have type 2 diabetes and use insulin to treat your condition, you should continue to take it as prescribed. If you avoid taking it, your blood sugar levels could become too high and you may become ill. Please speak to your healthcare professional if you have any questions or concerns about taking your insulin.
Insulin is a treatment that helps manage blood sugars, so this also reduces the risk of serious long-term complications as well a shorter-term consequences. Its still important to keep going to your appointments and manage your condition with healthy lifestyle choices. Staying active and eating a healthy diet will reduce the risk of complications from your diabetes, but insulin is also an important part of your treatment.
Recommended Reading: Is Insulin Used To Treat Type 2 Diabetes
Managing Type 2 Diabetes Through Exercise
Exercise is the third incredibly powerful strategy for reversing insulin resistance in type 2 diabetes.
When you exercise, cells in your muscle increase their energy requirements, which in turn increases their glucose requirements.
When your cells increase their energy demands, excess triglyceride is burned inside muscle cells, which in turn increases their responsiveness to insulin.
Timing Of The Intermediate

The pros and cons of timing of the intermediate-acting insulin injection has been examined in three studies . In two studies, a bedtime injection was recommended because it resulted in less weight gain or less hypoglycemias than a morning injection. In the third study, no differences in glycemia or weight gain were found .
Recommended Reading: Sure Comfort Insulin Syringes 30 Gauge
How Should This Medicine Be Used
Human insulin comes as a solution and a suspension . to be injected subcutaneously . Human insulin is usually injected subcutaneously several times a day, and more than one type of insulin may be needed. Your doctor will tell you which type of insulin to use, how much insulin to use, and how often to inject insulin. Follow these directions carefully. Do not use more or less insulin or use it more often than prescribed by your doctor.
Human insulin solution may also be injected intravenously by a doctor or nurse in a healthcare setting. A doctor or nurse will carefully monitor you for side effects.
Human insulin controls high blood sugar but does not cure diabetes. Continue to use human insulin even if you feel well. Do not stop using insulin without talking to your doctor. Do not switch to another brand or type of insulin or change the dose of any type of insulin you use without talking to your doctor.
Human insulin comes in vials, prefilled disposable dosing devices, and cartridges. The cartridges are designed to be placed in dosing pens. Be sure you know what type of container your insulin comes in and what other supplies, such as needles, syringes, or pens, you will need to inject your medication. Make sure that the name and letter on your insulin are exactly what your doctor prescribed.
If your human insulin comes in a disposable dosing device, read the instructions that come with the device carefully. Ask your doctor or pharmacist to show you how to use the device.
Type 1 Diabetes Causes
- Family history of type 1 diabetes
- Childhood consumption of cows milk, often before 1 year of age
- Mycobacterium avium paratuberculosis in dairy and meat products
- Enterovirus infections
- A sedentary lifestyle
- Excess body weight
In essence, type 1 diabetes is a disease that manifests beyond your control, while type 2 diabetes is loosely determined by your genetics and largely determined by your lifestyle.
Read Also: What’s The Treatment For Type 2 Diabetes
Diagnosing Type 2 Diabetes
According to the American Diabetes Association, in order to be diagnosed with type 2 diabetes, one of the following must be true:
- An A1c value 6.5%
- A fasting plasma glucose value 126 mg/dl . Fasting is defined as no caloric intake for at least 8 hours.
- A 2-hour plasma glucose value 200 mg/dl during an oral glucose tolerance test
- A random plasma glucose value 200 mg/dl
The majority of people live with some form of insulin resistance without recognizing the symptoms for years before being officially diagnosed with type 2 diabetes.
The A1c test is a blood test that provides information about your average blood glucose levels over the past 3 months.
An OGTT is a test of your ability to metabolize glucose in response to a glucose challenge, and works like this:
- Step 1: After an extended fasting period , youll arrive at a medical clinic. A doctor will test your fasting blood glucose
- Step 2: Youll be asked to drink a glucose solution containing 75g of glucose
- Step 3: Depending on the clinic and the specific testing protocol, a medical professional will test your blood glucose , either following 1 hour, 2 hours, and/or 3 hours
- Step 4: If your blood glucose is greater than 200 mg/dL 2 hours after you drink the glucose solution, you are diagnosed with type 2 diabetes
Type 1 Diabetes Diagnosis
- A c-peptide value lower than 0.2ng/mL
- The presence of one or more diabetes autoantibodies
- A fasting blood glucose greater than 125 mg/dL
- A random finger stick blood glucose greater than 200 mg/dL
- An A1c greater than or equal to 6.5%
- An Oral Glucose Tolerance Test with a blood glucose value exceeding 200 mg/dL at any time
Recommended Reading: Why Do Diabetics Legs Swell
Approach To The Patient
Guidelines from the ADA and the American Association of Clinical Endocrinologists recommend a comprehensive, patient-centered approach for achieving and maintaining glycemic control. Figure 1 provides multiple pharmacotherapy options based on A1C levels, fasting or postprandial glucose control, weight loss, and adverse effects.1,12,32 Although glycemic control is important, addressing other cardiovascular risk factors, such as hyperlipidemia and hypertension, is at least as important but is beyond the scope of this article.
Management of Type 2 Diabetes Mellitus
Figure 1.
Algorithm for the management of type 2 diabetes mellitus.
Information from references 1,12, and 32.
Management of Type 2 Diabetes Mellitus
Figure 1.
Algorithm for the management of type 2 diabetes mellitus.
Information from references 1,12, and 32.
Quality Assessment Of The Included Studies
Twenty-seven,,,,,,,,,,,,,,,,,,,,,,,,,, and twenty-three,,,,,,,,,,,,,,,,,,,,,, of the 50 studies did not describe their methods of generating a random number and of allocation concealment, respectively. In the assessment for the blinding of patients and personnel, 8 trials,,,,,,, were evaluated as high-risk, as they were open-label trials. For the risk of incomplete outcome data, most studies,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,, were rated as low-risk. Three studies,, were considered open to a high risk of selective reporting bias since we used their data from the Clinicaltrials.gov website only, and those data were not regarded as complete reports. Most of the trials,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,, had balanced baseline characteristics between the treatment groups. The detailed results of the assessment are found in Supplementary Figure .
Recommended Reading: Nursing Care Plan For Diabetes
Whats The Difference Between Type 1 And Type 2 Diabetes
Type 1 and Type 2 diabetes are two of the fastest-growing chronic conditions on the planet, and combine to affect more than 34 million people in the US .
The main difference between the two forms of diabetes is actually quite simple.
Type 1 diabetes is an autoimmune condition in which your bodys immune system mistakenly targets insulin-producing beta cells for destruction.
Type 2 diabetes, on the other hand, is not an autoimmune condition. With type 2 diabetes, your body can produce insulin, but it is not sufficient to control your blood glucose thanks to a condition called insulin resistance.
According to the American Diabetes Association, type 1 diabetes is less common, occurring in 1.5-2 million people in the United States .
Type 2 diabetes is more common, occurring in 31-32 million people .
Prediabetes is the precursor condition to type 2 diabetes, and is estimated to affect another 88 million more people in the US. According to the CDC, of those with prediabetes, more than 84% of them dont even know it.
Type 1 diabetes is more common in young people, though not always. Meanwhile, type 2 more commonly manifests later in life.
However, while they both manifest in the same initial symptoms, their causes and overall treatment plan can be very different.
In this article, well explore the differences between type 1 and type 2 diabetes in detail.
Well touch on their causes, risk factors, symptoms, and diagnoses.
Type 1 Vs Type 2 Diabetes: Whats The Difference
In type 1 diabetes, insulin deficiency initially occurs as a result of an autoimmune condition in which your immune system mistakenly attacks the beta cells in your pancreas.
As a result, the population of beta cells in your pancreas is significantly compromised, resulting in insulin insufficiency and high blood glucose.
In non-insulin-dependent type 2 diabetes, the beta cells in your pancreas can produce enough insulin, but the insulin they produce is not powerful enough to overcome the amount of insulin resistance in your muscle and liver.
In the case of insulin-dependent type 2 diabetes, beta cells that have been overproducing insulin for months to years begin dying, resulting in a reduced population and insufficient insulin production.
Don’t Miss: Diabetes And Heat Exhaustion Symptoms
When Should I Contact My Healthcare Provider
- You feel or see hard lumps in your skin where you inject your medicine.
- You think you gave yourself too much or not enough medicine.
- Your injections are very painful.
- You see blood or clear fluid on your injection site more than once after you inject medicine.
- You have questions about how to give the injection.
- You cannot afford to buy your diabetes supplies.
- You have questions or concerns about your condition or care.