Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
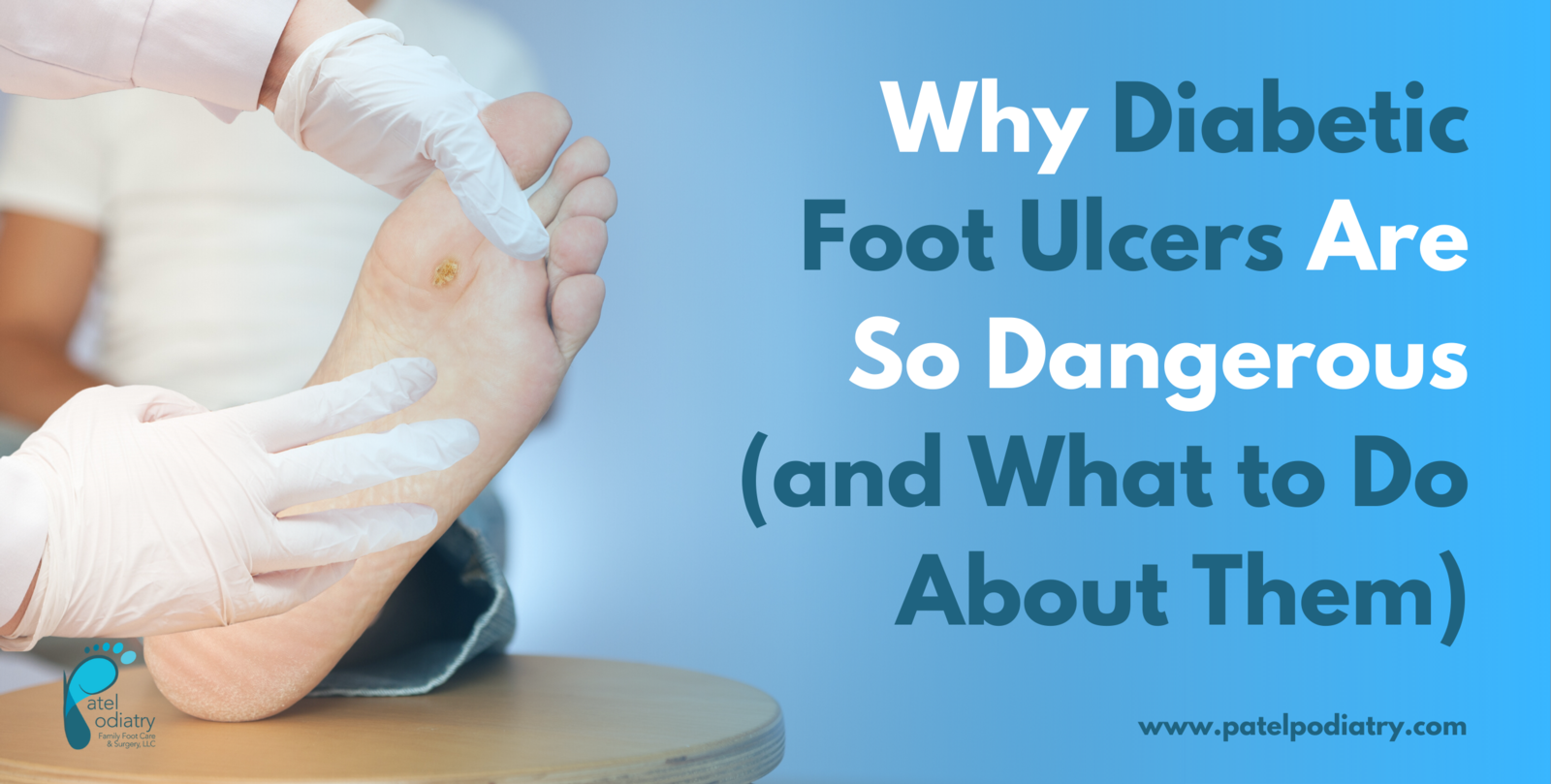
Promising Treatments For The Healing Of Diabetic Foot Ulcers
The number of Canadians with #diabetes is rapidly increasing. According to the Canadian Diabetes Association, more than 20 Canadians are diagnosed with the disease every hour of every day.
#Diabetic foot ulcers are the most common chronic complication from diabetes, affecting four to 10 per cent of patients. DFUs can last a year or longer and can happen again in up to 70 per cent of people who have previously been affected. Patients are more likely to develop DFUs if they have had diabetes for a long time, have poorly controlled blood sugar, have foot injuries or infection, are older, or smoke. However, neuropathy, damage to the nerves, which may result in a lack of feeling in the feet, and peripheral artery disease, which reduces the blood flow to the limbs, may be the most significant causes. Because of nerve damage and numbness, an individual with diabetes may not be aware that they have a sore or wound, leading to even minor injuries getting worse or becoming infected. Decreased blood flow caused by peripheral vascular disease may prevent healing once an injury occurs.
When DFUs become infected, the bone or skin can also become infected. This can lead to significant pain and suffering poor quality of life for patients amputation of a leg, foot, or toe increased treatment and hospitalization costs and can even lead to death.
Off-Loading Devices
Compression Therapy
Diabetic Shoes And Boots
Your doctor may recommend Unna Boots or other diabetic shoes or boots to treat your diabetic wound. Unna Boots are compression bandages designed to provide a semi-solid mold around the foot and lower leg. The boots apply gentle pressure, but still allow movement, and the medicated paste on the inside of the boots keeps your diabetic wound moist to promote healing and provide protection against infection.
Also Check: Insulin Brands For Type 2 Diabetes
Can Emuaid Help Relieve Diabetic Ulcers Naturally
Yes! Before we show you how EMUAID® works, there’s something you must know.
Your skin is a barrier designed to keep bacteria and infections out. Most medications cannot penetrate deep into the skin to efficiently deliver the active ingredients to where they are needed the most.
No matter how effective the medication is, there’s no use if it can’t penetrate the skins barrier to treat your your diabetic ulcers.
EMUAID® is different.
EMUAID® is specially designed to penetrate skin. It has a unique delivery system that helps carry powerful healing ingredients deep into your skin.
How To Prevent And Treat Blisters
How to prevent and treat blisters
While we often think of blisters on our feet, these painful skin irritations can occur anywhere on the body where body parts rub together or rub against clothing. To prevent chafing that can lead to blisters, dermatologists recommend following these tips.
While we often think of blisters on our feet, these painful skin irritations can occur anywhere on the body where body parts rub together or rub against clothing. Fortunately, blisters can be prevented by preventing chafing. To stop them before they appear, pay attention to your skin and take precautions if you know youre going to do a lot of walking, running, or other physical activity.
To prevent chafing that can lead to blisters, dermatologists recommend the following tips:
Protect your feet. To prevent blisters on your feet, wear nylon or moisture-wicking socks. If wearing one pair of socks doesnt help, try wearing two pairs to protect your skin. You should also make sure your shoes fit properly. Shoes shouldnt be too tight or too loose.
Wear the right clothing. During physical activity, wear moisture-wicking, loose-fitting clothes. Avoid clothes made of cotton, as cotton soaks up sweat and moisture, which can lead to friction and chafing.
Consider soft bandages. For problem areas, such as the feet or thighs, consider using adhesive moleskin or other soft bandages. Make sure the bandages are applied securely.
To treat a blister, dermatologists recommend the following:
Read Also: How Much Does It Cost To Make Insulin
Control Your Blood Sugar
Of course, keeping your diabetes under control is the best overall strategy to prevent diabetic wounds. Working with your doctor to treat your diabetes with diet, exercise, and medication adjustments can have a huge influence on the efficiency of your bodys natural wound-healing process and immune system.
If you can optimize the activity of red blood cells, white blood cells, and your overall circulatory system, youll begin to improve your bodys wound healing response and protect yourself from non-healing diabetic wounds.
A Word From Mantracare
If you are looking for more information on this topic or Diabetes treatment, Online Therapy, Hypertension, PCOS treatment, Weight Loss, and Physiotherapy, please visit mantracare.org or feel free to reach out to us at +91-9711118331 or email at . You can also download our free Android App or IOS app.
Here at Mantra Care, we have an incredibly skilled team of health care professionals and coaches who will be happy to answer any questions and provide further information so you know whats best for your unique needs.
You May Like: Financial Help With Diabetic Supplies
Preventing A Diabetic Foot Ulcer
Holistic treatment of the individual with diabetes can help treat the underlying health issues and not only promote faster wound healing but also minimize risk factors that may have contributed to the development of a diabetic foot ulcer. Good diabetic control and lifestyle modification include:
- Keeping blood glucose levels optimal.
- Good nutrition and eating habits.
- Reducing high blood pressure.
- No smoking.
Individuals with diabetes should be instructed to:
- Examine their feet daily with a mirror and to look carefully for fungal infections or any abnormality.
- Wash and dry feet at least once a day in lukewarm water , paying special attention to dry between the toes.
- Not use heating pads or put feet close to heaters.
- Always use footwear inside and outdoors.
- Use close-toed shoes if they can’t feel their feet.
- Always use socks and change them daily.
- Have their nails cut carefully straight across by a trained professional .
- Treat dry feet with lubricants containing urea or salicylates, but don’t apply between toes.
In addition, every patient with diabetes should have a comprehensive foot exam yearly. Along with a careful physical exam, health care professionals should reinforce best practices of diabetic foot self-care at each visit to make sure the individual understands the recommendations and importance of caring for their feet.
Keep It Dressed And Safe
One way to treat the wound is to protect it. A simple band-aid wont do. A medical gauze is recommended to cover the wound and keep it safe from bacteria that may infect it. Avoid using a simple clean white cloth unless there is no other choice, as these get dirty too easily. If you must use a cloth to dress your wound, make sure it is changed and maintained regularly.
You May Like: What Is The Most Common Form Of Diabetes
Bacterial Skin Infections Need Immediate Treatment
Although anyone can get bacterial skin infections, people with diabetes are more prone to them. Typical bacterial skin problems that tend to trouble patients include eyelid sties, boils, nail infections, and carbuncles deep infections of the skin and the tissue underneath. Usually, the area around the infection will be hot, red, painful, and swollen. Treatment with antibiotic creams or pills will usually clear up these skin problems.
How Diabetic Foot Ulcers Are Treated
If you do develop a diabetic foot ulcer, your podiatrist will perform debridement of the wound. This means that the doctor will remove the dead skin and tissue from the ulcer to encourage the healing of the tissue. The podiatrist will then apply a dressing to it to prevent an infection. The physician can also perform off-loading to relieve pressure from your foot ulcers, whereby your foot may be placed in a special boot, brace, or cast as your ulcers heal.
You May Like: What Do You Do If You Think You Have Diabetes
Etiology Of Foot Ulceration
The etiology of diabetic foot ulcers usually has many components.4,7 A recent multicenter study8 attributed 63 percent of diabetic foot ulcers to the critical triad of peripheral sensory neuropathy, trauma, and deformity. Other factors in ulceration are ischemia, callus formation, and edema. Although infection is rarely implicated in the etiology of diabetic foot ulcers, the ulcers are susceptible to infection once the wound is present. Many of the risk factors for foot ulcer are also predisposing factors for amputation, because ulcers are primary causes leading to amputation.5,7,9 Recognized risk factors for diabetic foot ulceration are listed in Table 1.4
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
Practice Proper Wound Care
You cant ignore your diabetic wound and expect it to heal on its own. The very fact that you have diabetes automatically makes wound healing more difficult. By practicing proper diabetic wound care, you will protect your wound from infection and help the healing process continue.
Proper wound care is different for every patient. The size, age, and condition of your wound determine the specific type of care you need to accelerate healing. A few possible wound care options include collagen skin substitutes, foam dressing, calcium alginates, and enzyme applications.
Also Check: What Are The Symptoms Of A Diabetic Foot
Check And Wash Your Feet Daily
In addition to wearing the right shoes, be sure to check your feet, or ask a spouse or friend to check your feet, every single day. Diabetic nerve damage makes it much harder for you to feel any pain caused by wounds, so only a visual inspection will reveal signs of injury. Look carefully for cuts, cracks, and blisters. Check closely around the nails since this area is especially vulnerable to infection.
Also make sure to wash your feet at least once a day with warm water and dry them afterwards. Its important to dry between each individual toe so that moisture doesnt accumulate and breed bacteria. Take this time to gently trim your toenails in a way that prevents ingrown nails. Moisturize your feet after washing to minimize cracking and chafing as well.
Complications Of Untreated Diabetic Ulcers
If a diabetic ulcer is not adequately treated, the risk of infection can significantly increase. Abscesses, the spread of disease, gangrene, and eventual amputation are all possible outcomes of poorly treated or neglected diabetic ulcers.
Diabetic foot ulcers can quickly become severe conditions. By treating them as soon as possible, the condition can be remedied before the chance of infection. Serious wounds will not go away on their own and will require prompt attention.
Fortunately, diabetic ulcers can be easily detected. Unlike ulcers that form on the inside of the body, these wounds can be seen and felt. A diabetic ulcer’s symptoms include foot pain, discoloration or numbness, and a deepening wound that will not heal with time. Diabetic ulcers occur in those who have diabetes. The diagnosis of diabetes combined with painful wounds on the bottom of the feet is a good indication that a diabetic ulcer needs treatment.
Don’t Miss: Best App To Track Diabetes
How Emuaid Works To Eliminate Your Diabetic Ulcer Symptoms
Why Are Diabetics Prone To Foot Ulcers And Other Chronic Wounds
Diabetic patients are more prone to developing chronic wounds for a few reasons. Two of the most influencing factors are nerve damage and blood circulation issues that are common among diabetic patients.
Nerve damage, or neuropathy, tends to occur in patients who have a longer history with diabetes because elevated blood glucose levels damage nerves over time. Neuropathy causes patients to experience reduced, or lack of, sensation in the areas affected.
Many patients can sustain trauma or develop an infection without realizing it because theyre unable to feel pain in the area. Further, neuropathy commonly affects the feet, so a wound on the bottom of the foot can escalate quickly because the patient cannot feel or see the wound easily.
Blood circulation issues also can increase the risk for developing chronic wounds, as well as making the wounds more prone to infection. High blood glucose levels cause the narrowing of blood vessels, which constricts blood supply, Estocado said. Adequate blood supply is essential to normal wound healing. The secondary effect of impaired blood supply is a decrease in white blood cells, which are responsible for fighting infection and maintaining a strong immune system.
You May Like: Normal A1c For Non Diabetics
You May Like: What Can People With Type 2 Diabetes Eat
From Injury Or Blister To Ulcer
If a person with decreased sensation gets a blister or other injury, they may not notice it and it can develop into an ulcer.
Neuropathy:Neuropathy is a general term for nerve dysfunction. Peripheral neuropathy is the most common type of neuropathy in people with diabetes and typically affects the nerves of the feet, legs, and sometimes the arms and hands.
People with diabetes are at increased risk for peripheral neuropathy if they have a history of hyperglycemia and have had diabetes for a long time. Other risk factors for neuropathy include smoking and genetic predisposition.
Over time elevated blood sugar levels can affect nerve functioning and nerve signaling. Small nerve dysfunction results in the inability to feel pain, and large fiber dysfunction causes disturbances in balance, which can increase the risk of falls.
If a person has neuropathy and injures their foot without feeling it, they may not notice it until it gets much worse. Recurrent, unnoticed injuries to the foot can increase the risk of Charcot foot, in which progressive destruction of the bones and joints leads to foot deformity.
Autonomic neuropathy can cause a decrease in sweating, resulting in dry feet. Having dry feet can increase the risk of developing calluses. While calluses are healthy, if you have lost sensation, they can grow deeper cause damage to the skin surface known as breakdown, putting the foot at risk of blisters or ulcers.
Who Can Get A Diabetic Foot Ulcer
Anyone who has diabetes can develop a foot ulcer. Native Americans, African Americans, Hispanics and older men are more likely to develop ulcers. People who use insulin are at a higher risk of developing a foot ulcer, as are patients with diabetes-related kidney, eye, and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.
Read Also: Low Carb Meal Plan For Diabetics Type 2
Make Sure You Dont Have An Infection:
- This is an area where your podiatrist can work with an infectious disease doctor. If you have any redness around your wound or drainage from the center of your wound, you likely have an infection of the current. In the short term, it is essential to start taking antibiotics and to get antibiotic medication onto this site. This can be life-threatening if allowed to continue for lengthy periods of time without improving.
- If you have redness or drainage developing around your ulcer, dont waste any time, this is the single most urgent thing you can do, dont be someone who loses their leg because they waited one or two days too long.
Recommended Reading: Normal A1c Levels Non Diabetics
What Are Leg Ulcers

Leg ulcers are sores that develop on broken or injured skin. Usually, they are more prominent right above the ankles, on the inner side of your legs.
Other than skin injuries, leg ulcers may also develop as a result of an underlying medical condition. The diseases which may lead to the development of leg ulcers are discussed briefly below.
Recommended Reading: Is Plant Based Diet Good For Diabetics
Type 2 Diabetes Can Be A Devastating Diagnosis Says Expert
We use your sign-up to provide content in ways youve consented to and to improve our understanding of you. This may include adverts from us and 3rd parties based on our understanding. You can unsubscribe at any time. More info
It is hard to put a specific number on the amount of people living with type 2 diabetes in the UK because many people will currently have it without knowing it. Thats because the condition can be subtle or symptomless for many years. Perceptible changes can crop up if rising blood sugar levels a feature of type 2 diabetes start to interfere with bodily processes.