Can I Have A Negative Reaction To Insulin
One complication facing people with diabetes who use insulin is the potential for severe hypoglycemia, also known as insulin shock, which involves using too much insulin and causing your blood sugar to drop extremely low. This can cause coma, seizures, and heart attacks, says Dr. Powers. It requires treatment in a hospital but thankfully is highly treatable once you are there.
Challenges To Fully Automated Insulin Delivery
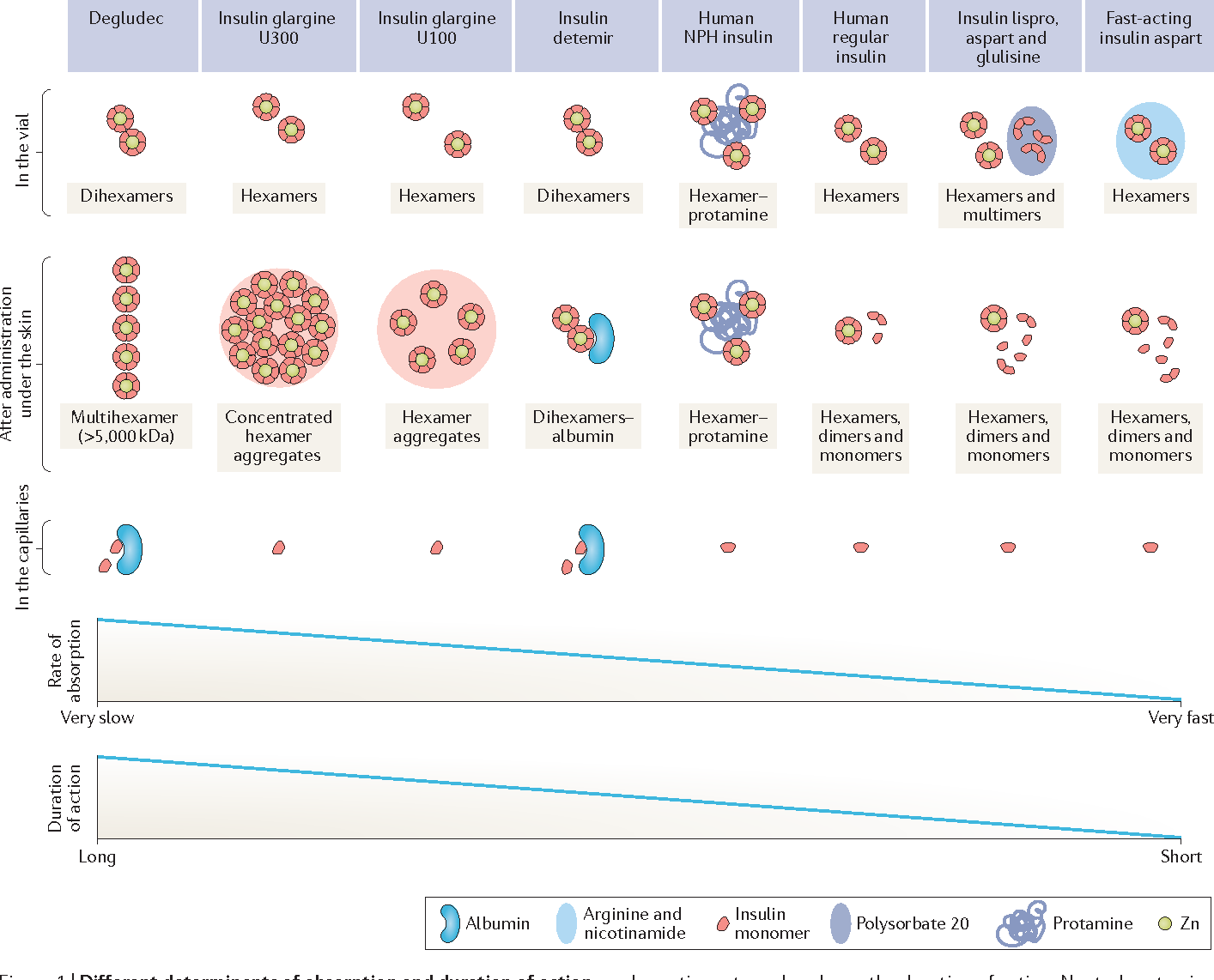
One the main challenges to achieving fully automated closed-loop insulin delivery is overcoming the kinetics of nonphysiologic subcutaneous insulin administration related to postprandial glucose excursions. Given the kinetics of subcutaneous insulin delivery, increased insulin dosing that occurs only after the glucose excursion has begun may lead to prolonged hyperglycemia. Furthermore, because of variations in physiologic insulin needs and the kinetics of current insulin formulations, increased insulin delivery can result in late hypoglycemia. Exercise can compound these challenges by altering insulin sensitivity and increasing insulin-independent glucose uptake into muscles. Several approaches have been studied to ameliorate this issue. Adjunctive therapies including pramlintide , GLP-1 receptor agonists, dipeptidyl peptidase-4 inhibitors, and sodiumglucose cotransporter 2 inhibitors have all been studied in patients with T1D with the goal of decreasing postprandial glycemic excursions and reducing the need for aggressive insulin dosing. Alternate approaches to insulin delivery, such as delivery of insulin directly to intraperitoneal space, enable faster pharmacokinetics/pharmacodynamics than subcutaneous insulin delivery. Studies examining the utility of new ultrarapid-acting insulins in AID systems have suggested decreased glycemic variability with these newer insulin analogues.
What Health Insurance Plans Cover People With Diabetes
Health insurance helps pay for medical care, including the cost of diabetes care. Your health insurance options are
- private health insurance, which includes group and individual health insurance
- government health insurance, such as Medicare, Medicaid, the Childrens Health Insurance Program , TRICARE, and veterans health care programs
Under current law, health insurance companies cant refuse to cover you or charge you more just because you have a pre-existing conditionthat is, a health problem you had before the date that new health coverage starts.
Changes to insurance rules happen often and may affect your health insurance choices. Learn more or get help with your health insurance questions through
- HealthCare.gov , the federal marketplace, 1-800-318-2596, TTY: 1-855-889-4325
- copayments and deductibles
- health care providersdo your providers participate in the plan, or will you have to change providers or pay more to see your current providers because they are out of network?
Ask for a Summary of Benefits and Coverage, which explains the plan in plain language, including free preventive services. This summary may include a coverage example for managing diabetes.
Also Check: What Is Considered Low Blood Sugar For Type 2 Diabetes
What Is The Childrens Health Insurance Program
CHIP offers free or low-cost Medicaid to children whose parents earn too much for Medicaid but not enough to pay for a private health plan. In some states, CHIP may also cover pregnant women and parents. Learn whether your family members qualify for CHIP through HealthCare.gov or your states Medicaid or CHIP agency.
Learn more about CHIP at www.insurekidsnow.gov or call 18775437669.
Options For Uninsured Patients

First, remember to check for coupons like those at Goodrx.com and patient assistance programs offered by insulin manufacturers. Major insulin manufacturers in the US offer patient assistance programs to uninsured patients and patients on Medicare Part D, so they can get their insulin for free. These programs have certain eligibility restrictions, requirements and limitations, so be sure to read the fine print before using them. More information is available below.
Then, patients sometimes ask if they can switch to an insulin that may be cheaper out of pocket. Insulins come in certain classes, like rapid-acting or long-acting insulins. But even within these classes, individual insulins may have different peak times and durations of effectiveness. While there are standard conversion recommendations when changing from one insulin to another, this process requires close observation from a physician, especially if the patient has type 1 diabetes. It may also involve the use of a continuous glucose monitorlike Dexcom, Libre, and Eversense sensorswhich are relatively new to the field of diabetes treatment.
Also Check: What’s The Treatment For Type 2 Diabetes
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you dont have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting drunk while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, dont try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. Ive had people tell me theyre tired of taking insulin, or that theyre rationing it due to cost. In type 1 diabetes, thats all it takes to end up in a life-threatening situation, says Dr. Zilbermint.
Disposal Of Used Insulin Syringes
Used syringes, pen needles, cannulas and lancets must be disposed of in an Australian Standards-approved sharps container, which is puncture-proof and has a secure lid. These containers are usually yellow and are available through pharmacies, local municipal councils and state or territory diabetes organisations such as Diabetes Victoria.
Procedures to dispose of sharps containers vary from state to state.
For sharps disposal information and help, you can contact:
- state or territory diabetes organisations, such as Diabetes Victoria
- state Department of Health
Insulin needs to be stored correctly. This includes:
- Store unopened insulin on its side in a fridge.
- Keep the fridge temperature between 2 and 8 °C.
- Make sure that insulin does not freeze.
- Once opened, keep it at room temperature for not more than one month and then dispose of it safely.
- Avoid keeping insulin in direct sunlight.
Extreme temperatures can damage insulin so it doesn’t work properly. It must not be left where temperatures are over 30 °C. In summer your car can get this hot so don’t leave your insulin there.
There are various insulated insulin carry bags available for transporting insulin.
You May Like: What To Do If You Think Your Diabetic
How To Get Free Prescriptions For Diabetes Medicine
You’re entitled to free prescriptions for your diabetes medicine.
To claim your free prescriptions, you’ll need to apply for an exemption certificate. This is known as a PF57 form. To do this:
- fill in a form at your GP surgery
- you should get the certificate in the post about a week later it’ll last for 5 years
- take it to your pharmacy with your prescriptions
Save your receipts if you have to pay for diabetes medicine before you receive your exemption certificate. You can claim the money back if you include the receipts along with your completed PF57 form.
How 2 Type 1
Do you live with type 1 diabetes? Do you care for someone who does? Whether you’ve been recently diagnosed or living with the disease for years, How 2 Type 1 is for you. This video, developed in partnership with the Diabetes Leadership Foundation, aims to provide support, knowledge, expert advice, and actionable steps to help you and others in the type 1 diabetes community thrive!
Don’t Miss: How To Get Rid Of Diabetes Stomach Fat
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
What does insulin do? Help your body turn food into energy, for starters. When you have diabetes, and youre either not producing insulin or your insulin function is off, all sorts of things can go wrong. From needles to pens to pumps to types of insulin, were here to empower you with clear answers to all your pressing questions.
In This Article:
Alvin Powers, MD, Mihail Zilbermint, MD, and Irl Hirsch, MD
The Future Of Diabetes Management
Maintaining blood glucose concentrations near the normal range is critical for successful long term health of patients with diabetes.,, , Current therapies required to achieve good glucose control in insulin-dependent diabetes are extremely demanding, requiring frequent blood control checks and calculations of insulin requirements to treat meals and glucose excursions above the target range. Once the dose is calculated, patients must manually administer the insulin by injection or using an insulin pump. The rate of insulin absorption after subcutaneous injection is slower than the absorption of carbohydrates from food, adding to the difficulty of maintaining glucose levels within the target range. Rapid-acting insulin analogs which became available in the 1990s have improved pharmacokinetic properties, but are still far from ideal, and insulin absorbance rates are highly variable from patient to patient, and even for the same patient on different occasions. This contributes to the difficulty of knowing the correct dosage of insulin for a given situation. , , Insulin’s more rapid absorption kinetics are being developed and nearing approval.
Also Check: What Gauge Are Insulin Needles
Your Right To Access Medications Devices & Supplies
If you have diabetes, we believe you should be able to get the right medication at the right time. You should have access to affordable treatments that allow you to achieve and maintain an excellent quality of life.
Access to the medications, devices and supplies that best meet your needs can reduce your risk of complications and help you to avoid hospitalizations.
Evidence-based diabetes treatments should be made available through public plans for all those who require them. Federal, provincial and territorial governments must ensure that the cost of diabetes medication, devices and supplies, and the costs associated with diabetes-related complications, are not a barrier or a burden to managing the disease.
For more information, view Diabetes Canada’s position on access to medications, devices & supplies.
How Should I Store My Insulin
- Keep current insulin at room temperature to help alleviate injection discomfort.
- Insulin can usually be stored at room temperature for about a month. Once in use, insulin pens should be stored at room temperature. Expiration dates of insulin pens can vary depending upon the type of insulin. For disposable pens, you should discard the entire device when empty or when you reach the expiration date.
- Store extra insulin in the refrigerator.
- Dont expose insulin to excessive cold or heat.
Don’t Miss: How To Care For Someone With Diabetes
Factors That Speed Insulin Absorption
Variation in insulin absorption can cause changes in blood glucose levels. Insulin absorption is increased by:
- injecting into an exercised area such as the thighs or arms
- high temperatures due to a hot shower, bath, hot water bottle, spa or sauna
- massaging the area around the injection site
- injecting into muscle this causes the insulin to be absorbed more quickly and could cause blood glucose levels to drop too low.
Help With Your Diabetes Prescription And Insulin Costs
All people with T1D should have affordable access to insulin. While sharing the resources below that can help with costs, JDRF is also fighting for changes from manufacturers, health plans, employers, and the government to make insulin more affordable. Learn more here.
Prescription costs for drugs to treat type 1 diabetes can make up a large percentage of what you pay each year for healthcare. There are a few ways you can lower your prescription and insulin costs: through state and nonprofit programs diabetes patient assistance programs offered by pharmaceutical companies medication discount cards and prescription alternatives such as biosimilar insulin.
Recommended Reading: Diabetes Kidney Failure Life Expectancy
Intraindividual Cvs Of Plasma Insulin Concentrations And Girs
The intraindividual CVs, a measure of PK/PD variability, were calculated in all four studies, comparing R+ with R- horizontal, R- up, and R- down. In the latter three studies, the greatest variability for free immunoreactive insulin Cmax and GIR Cmax occurred between R+ and R- down. This was also the case for FIRI_AUC. The GIR_AUC had the highest CV in all comparisons, the more elevated values being between R+ and R- horizontal .
What Else Can I Do To Control My Blood Glucose Levels
Food, sleep, and exercise are all of vital importance for regulating your blood sugar when you have diabetes.
Also Check: How Do Diabetics Check Their Blood Sugar
Type 1 And Celiac Disease
Its estimated that those who are Type 1 are eight to ten times more likely to suffer from celiac disease .
In fact, doctors now recommend screening for celiac or Type 1 diabetes in people already diagnosed with either of the two conditions. Both are genetic disorders that share similar genes. Both are immune-regulated and associated with autoimmune conditions like thyroiditis and rheumatoid arthritis.
Those with Type 1 and undiagnosed celiac disease often experience unstable blood glucose levels, decreased insulin requirements, weight loss, and a loss of bone density. Even after getting diagnosed and starting a gluten-free lifestyle, symptoms may take up to a year to improve as the gastrointestinal tract heals and begins to properly absorb food and nutrients.
While having celiac disease alongside Type 1 doesnt have to significantly alter or dictate your quality of life, there are a few things to have on your radar when living with both conditions, particularly around the issue of medications.
What about cold medications and celiac disease specifically?
Gluten-free Meds
- Common analgesic pain and fever reducers like Tylenol, Advil, Aleve, and Motrin
- antihistamines, decongestants, and cough/cold medicines such as Allegra, Sudafed, Dayquil, and Robitussin liquid gels and caplets
Experimental Automated Insulin Delivery Systems
Several AID systems that rely on different sets of mathematical algorithms, including proportional integral derivative, fuzzy logic, and model predictive control algorithms, are in development. These AID systems have been associated with increased time in target glucose range and in some cases with decreased mean glucose, lower HbA1c, and decreased time in the hypoglycemic range. Pivotal trials for several of these AID systems are currently ongoing, including the Omnipod Horizon hybrid closed-loop system and the Beta Bionics iLet Bionic Pancreas .
Other classes of dual hormone systems that have been studied administer pramlintide or glucagon-like peptide-1 receptor agonist in combination with insulin., Amylin is cosecreted with insulin from pancreatic beta cells and helps moderate postprandial glucose excursions by slowing gastric emptying, inhibiting glucagon secretion, and promoting satiety. A recent study examining an automated system delivering fixed dose ratio of insulin and pramlintide found increase in time in range compared with the insulin-only system. Long-term studies of bihormonal systems are needed to establish their potential benefits.
Recommended Reading: Low Carb Meal Plan For Diabetics Type 2
What Are The Drawbacks To Insulin Treatment For Diabetes
The biggest issue with insulin right now is unaffordability. A box of rapid-acting insulin can cost $400 without insurance. As so many people continue to lose their health coverage, its becoming an enormous problem, Dr. Zilbermint says.
Consistently rising costs have led some patients to ration their insulin, which can be dangerous and even deadly. The cost of testing strips is also an issue, and both have led to a black market in testing strips and insulin. Its illegal, says Dr. Zilbermint, but its happening.
Pharmacokinetics And Pharmacodynamics Of Nph Insulin In Type 1 Diabetes: The Importance Of Appropriate Resuspension Before Subcutaneous Injection
Diabetes Care
Paola Lucidi, Francesca Porcellati, Anna Marinelli Andreoli, Ilaria Carriero, Paola Candeloro, Patrizia Cioli, Geremia B. Bolli, Carmine G. Fanelli Pharmacokinetics and Pharmacodynamics of NPH Insulin in Type 1 Diabetes: The Importance of Appropriate Resuspension Before Subcutaneous Injection. Diabetes Care 1 December 2015 38 : 22042210.
Crystalline NPH insulin comes in a two-phase solution with either a solvent or a rapid-acting insulin and needs adequate mixing for complete resuspension before injection. The aim of this study was to establish pharmacokinetics and pharmacodynamics after injection of appropriately resuspended versus nonresuspended NPH insulin.
PK and PD were assessed after subcutaneous injection of NPH insulin 0.35 units/kg at steady state by pen either resuspended or nonresuspended . Eleven subjects with type 1 diabetes were studied with a randomized crossover design.
Compared with resuspended NPH insulin , nonresuspended NPH insulin resulted in profound PK/PD differences with either reduced or increased plasma insulin concentrations and PD activity . Duration of NPH insulin action was shorter in R- up but longer in R- down compared with R+ . Within-subject variability among studies was as high as 23% for PK and 62% for PD .
Recommended Reading: Type 2 Diabetes Dry Mouth