Genome Wide Association Studies On Type 2 Diabetes
Until the early 2000s, so many candidate genes and linkage studies have been done but only succeeded in identifying very few susceptibility loci and the coming of genome wide association studies which focuses on searching single nucleotide polymorphisms that happen more frequent in people having a certain disease brought an interesting twist and is thought to be a breakthrough concerning the genetic research on Type 2 diabetes . Genes such KLF14, ENPP1, ADAMTS9, ADIPOQ, IRS, GCKR, SREBF1, FTO HNF4A, NOTCH2, IGF2BP2, CDKAL1, JAZF1, SCL30A8, HHEX, TCF7L2, EXT2, FTO and many others have been identified by this approach. By 2009 GWAS had identified 19 more SNPs associated with the Type 2 diabetes and this number increased to more than 60 SNPs by 2016 in Asian and European ancestry alone with researchers not only identified the variants and the genes involved but also validated the effects conferred by these reported common variants in different populations as conferred impacts may differ or might be the same but with substantial differences in allele frequencies as it is the evident with Chinese and European populations on variants in IGF2BP2, CDKAL1, JAZF1, SCL30A8, HHEX, TCF7L2, EXT2, and FTO and Europeans and North African Arabs in variants in TCF7L2 and other genes which made it possible to conclude that biological actions and activities of common variants may be similar in different ethnic groups.
What Are Other Risk Factors For Type 2 Diabetes
In addition to genetics and lifestyle choices, there are other risk factors for type 2 diabetes. These include age, ethnicity, and preexisting medical conditions such as prediabetes, which is having high glucose levels but not at diabetic levels, or polycystic ovary syndrome . You are also more likely to develop type 2 diabetes if you have a history of gestational diabetes or if you are overweight or obese. Certain ethnicities are more likely to develop type 2 diabetes including African Americans, Native Americans, Asian Americans, and Latino Americans. Age can be a factor as your risk of developing type 2 diabetes starts to increase in your mid-40s and raises even more after the age of 65.
Summary And A Way Forward
The promise of precision medicine is based on the individual or groups of individuals. The approach incorporates aspects of family history , lifestyle, and environment, such that the health care provider can customize interventions, diagnostics, and therapeutics to permit a healthier life for the patient and reduce health care utilization and costs. In diabetes, there are numerous forms of the disease at presentation, ranging from monogenic to those with complex etiologies that require exogenous insulin for survival, to the most common form that itself results from dysregulation of multiple, incompletely understood metabolic processes.
Monogenic diabetes is currently the form of diabetes that is most relevant for the application of precision medicine in terms of diagnosis and treatment. However, the growing understanding of monogenic diabetes alone will not lead to much change in clinical practice. Practical application of this information requires several additions to diabetes management as it occurs in most places. It is also important to recognize that the distribution of various forms of monogenic diabetes relative to type 1 diabetes or type 2 diabetes may differ across global populations. As a preliminary proposal, this expert panel suggests that three programs are needed to accomplish and sustain population-based diagnosis and management of these disorders.
Recommended Reading: Medtronic Vs Tandem Insulin Pump
Type 2 Diabetes Causes
Type 2 diabetes has several causes: genetics and lifestyle are the most important ones. A combination of these factors can cause insulin resistance, when your body doesnt use insulin as well as it should. Insulin resistance is the most common cause of type 2 diabetes.
Genetics Play a Role in Type 2 DiabetesLifestyle Is Very Important, Too
Genes do play a role in type 2 diabetes, but lifestyle choices are also important. You can, for example, have a genetic mutation that may make you susceptible to type 2, but if you take good care of your body, you may not develop diabetes.
Say that two people have the same genetic mutation. One of them eats well, watches their cholesterol, and stays physically fit, and the other is overweight and inactive. The person who is overweight and inactive is much more likely to develop type 2 diabetes because certain lifestyle choices greatly influence how well your body uses insulin.
- Lack of exercise: Physical activity has many benefitsone of them being that it can help you avoid type 2 diabetes, if youre susceptible.
- Unhealthy meal planning choices: A meal plan filled with high-fat foods and lacking in fiber increases the likelihood of type 2.
- Overweight/Obesity: Lack of exercise and unhealthy meal planning choices can lead to obesity, or make it worse. Being overweight makes it more likely that youll become insulin resistant and can also lead to many other health conditions.
Insulin Resistancenot Type 2 Risk Factors
Challenges In Diagnosis And Management
The presence of a monogenic form of diabetes should be considered when a patient does not seem to fit with the more common presentations of type 1 or type 2 diabetes. Decades of research on different populations have shown that any stringently defined set of features will be too restrictive to identify all people who carry a highly penetrant genetic variant. Such criteria, originally associated with the research by Stefan S. Fajans on MODY , have typically included onset before the age of 2535 years, lack of insulin dependency , absence of obesity or other signs of insulin resistance, and dominant inheritance over several generations. The absence of pancreatic islet-specific autoantibody titers associated with type 1 diabetes has now become another important measure. No approach will be sensitive enough to accurately detect every case or specific enough to ensure that genetic testing is not performed on patients who turn out not to have a monogenic diagnosis.
Selecting Appropriate Individuals for Genetic Screening
There are also barriers to making a diagnosis for certain individuals who are very likely to have MODY, such as those with diabetes who are first- or second-degree relatives of people with known monogenic diabetes. Evaluation of close relatives has not been a priority in diabetes care and can be challenging, especially when they receive health care from a different medical team or live far away.
Accessing Genetic Testing
Taking Appropriate Clinical Action
You May Like: Does One High A1c Mean Diabetes
What Are Monogenic Forms Of Diabetes
Some rare forms of diabetes result from mutations or changes in a single gene and are called monogenic. In the United States, monogenic forms of diabetes account for about 1 to 4 percent of all cases of diabetes.1,2,3,4 In most cases of monogenic diabetes, the gene mutation is inherited from one or both parents. Sometimes the gene mutation develops spontaneously, meaning that the mutation is not carried by either of the parents. Most mutations that cause monogenic diabetes reduce the bodys ability to produce insulin, a protein produced in the pancreas that helps the body use glucose for energy.
Neonatal diabetes mellitus and maturity-onset diabetes of the young are the two main forms of monogenic diabetes. NDM occurs in newborns and young infants. MODY is much more common than NDM and usually first occurs in adolescence or early adulthood.
What Is Maturity Onset Diabetes Of The Young
MODY is a monogenic form of diabetes that usually first occurs during adolescence or early adulthood. MODY accounts for up to 2 percent of all cases of diabetes in the United States in people ages 20 and younger.3
A number of different gene mutations have been shown to cause MODY, all of which limit the ability of the pancreas to produce insulin. This leads to high blood glucose levels and, in time, may damage body tissues, particularly the eyes, kidneys, nerves, and blood vessels.
Clinical features of MODY depend on the gene mutations a person has. People with certain types of mutations may have slightly high blood sugar levels that remain stable throughout life, have mild or no symptoms of diabetes, and do not develop any long-term complications. Their high blood glucose levels may only be discovered during routine blood tests. However, other mutations require specific treatment with either insulin or a type of oral diabetes medication called sulfonylureas.
MODY may be confused with type 1 or type 2 diabetes. In the past, people with MODY have generally not been overweight or obese, or have other risk factors for type 2 diabetes, such as high blood pressure or abnormal blood fat levels. However, as more people in the United States become overweight or obese, people with MODY may also be overweight or obese.
Also Check: Max Sugar Per Day For Diabetics
Are There Environmental Triggers For Type 1 Diabetes
About 25% of Caucasians have HLA types that are clearly associated with the risk of type 1 diabetes, but only about 1% of the total population actually develops type 1, says Dr. Olansky. What’s more, only about 5% of those who have the actual mutations develop the condition.
So why do these gene mutations raise the risk for some folks and not for others?
Again, experts’ knowledge is still in its infancy, but there seem to be environmental triggers that set the genes in motion. No one knows exactly what those triggers are but there are a number of candidates.
Certain pregnancy-related factors that have been associated with type 1 diabetes include having a mother older than 25 years, preeclampsia, neonatal respiratory disease, and jaundice, says Dr. Dr. Adimoolam.
Certain viruses have also been implicated, namely rubella and coxsackievirus, as has vitaminD deficiency and even exposure to cold weather.
But just as no one gene explains type 1 diabetes, likely no one environmental trigger will either.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
Screening In The Pediatric Population
Making a correct diagnosis of MODY in pediatric diabetes is important because these patients will spend almost their whole life living with diabetes, and increasing attention is directed to this problem. However, the correct diagnosis often is made years after an incorrect initial diagnosis, when assumed type 1 diabetes fails to progress. Making a MODY diagnosis close to the initial diagnosis of diabetes is a priority.
Currently, recognition of possible MODY cases is based on clinical features at follow-up rather than on any sort of assessment at the time of diabetes diagnosis. There is clear evidence of the need for systematic testing the multicenter SEARCH for Diabetes in Youth study in the U.S. showed that HNF1A, HNF4A, and GCK mutations accounted for 1.2% of diabetes cases in the pediatric population, but the vast majority of these patients with MODY were misdiagnosed and inappropriately treated with insulin. Screening procedures or algorithms based on islet autoantibodies that are reliable discriminatory factors at diagnosis could be used to direct genetic testing for MODY sooner. Using such protocols would reduce delays in recommended treatment and potentially reduce both personal and clinical costs.
You May Like: Diabetes Test App For Android
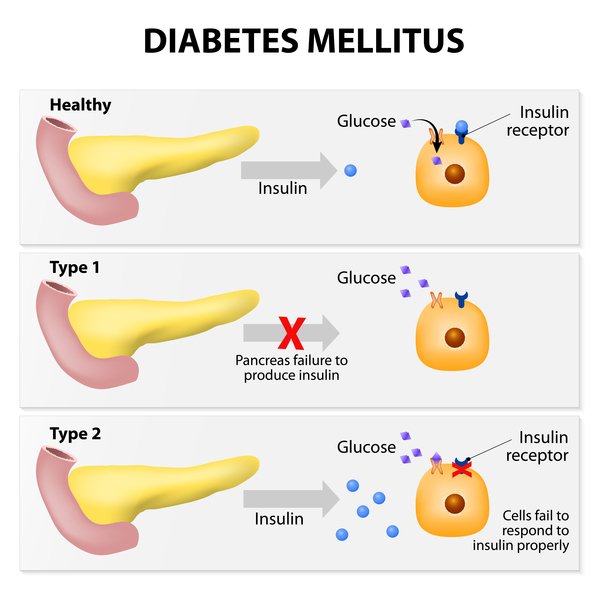
What Is The Difference Between Type 1 And Type 2 Diabetes
There are two main forms of diabetes, type 1 and type 2. There also is gestational diabetes in pregnant women too, but we will not be focusing on that type today. Type 1 diabetes is when your body doesnt produce enough insulin which helps to control the amount of sugar in your blood. Type 2 diabetes is when your body doesnt produce enough insulin or when the insulin doesnt work properly. Type 2 diabetes, which is the most common form, usually starts with insulin resistance, meaning your cells dont take in the proper amount of insulin. When type 2 diabetes is allowed to progress, your body then may lack enough insulin to be healthy.
Type 1 diabetes is usually diagnosed in children and young adults and is the leading cause of pediatric diabetes. It is also known as juvenile diabetes or insulin-dependent diabetes. Type 2 diabetes is usually diagnosed in adults over the age of 40, but it is now being seen in younger people as well.
Genetics And The Stages Of Type 1 Diabetes
The onset of T1D symptoms is the clinical manifestation of the disease process that results from the interaction of predisposing genetic factors with environmental exposures, which eventually leads to a T-cell mediated, B-cell facilitated, autoimmune attack on beta-cells. The presence of islet cell autoantibodies is presently the earliest and more robust biomarker of islet autoimmunity. Autoantibody responses to at least two islet antigens define the first stage of T1D at this point remissions are rare. Stage 2 T1D is defined as the presence of two or more islet autoantibodies and dysglycemia, that is, glucose metabolism abnormalities that do yet not meet diabetes criteria. Stage 3 develops when the established glycemic thresholds for diabetes diagnosed are exceeded. Although remissions after Stage 1 are rare, the risk and rate of progression vary based upon genetics, age at seroconversion, autoantibody titers and body mass index .
Also Check: The Best Protein For Diabetics
Diabetes Is A Complicated Condition Which Can Take Many Different Forms In Addition To The More Common Types Of Diabetes
About 2% of people have these other types of diabetes. These include different types of monogenic diabetes, cystic fibrosis-related diabetes, and diabetes caused by rare syndromes. Certain medications such as steroids and antipsychotics could lead to other types of diabetes, as well as surgery or hormonal imbalances. Unfortunately, many of these people are misdiagnosed leading to delays in getting the right treatment.
Were proud of the research we have supported to ensure better diagnosis and treatments for all types of diabetes, and its taught us a lot about the condition. You can find out more information on the different types of diabetes below:
Identification Of Spatial Eqtl
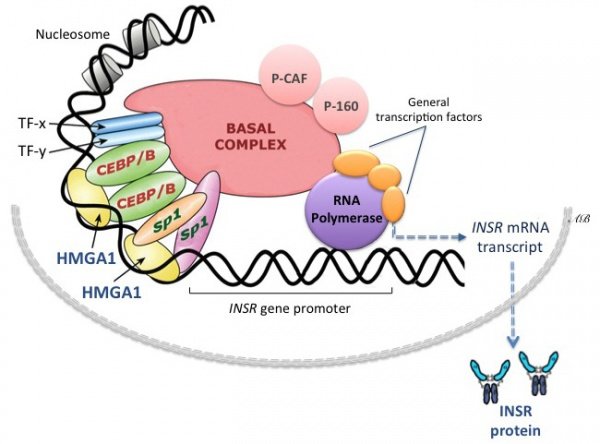
We used the Contextualizing Developmental SNPs in 3-Dimensions algorithm as described in to identify SNPs associated with the spatial regulation of gene transcript levels through physical interactions. Briefly, the CoDeS3D modular python scripts integrate Hi-C contact libraries from published sources to identify spatial co-localization of two DNA fragments, with one fragment marking the queried SNP. Gene-containing restricted fragments that are in physical contact with fragments containing the queried SNPs are identified as spatial pairs to the SNPs. Finally, the resultant spatial SNP-gene pairs are queried in the Genotype-Tissue Expression database to identify SNPs that are associated with transcript levels of genes through physical interaction at FDR< 0.05.
Here, we integrated extensive Hi-C contact libraries to identify all possible tissue, cell type and developmental stage-specific chromatin interactions based on the emerging evidence that complex diseases culminate from systems-level perturbations,. First, the spatial interactions were identified from Hi-C contact libraries captured from: primary human tissues primary and immortalized immune cell-types and embryonic stem cells, including cell lines representing embryonic germ layers . Next, the regulatory potential of the identified SNP-gene pairs was tested through the integration of expression QTL information from 47 human tissues and 2 immortalized cell-lines .
Recommended Reading: What Happens If Diabetes Is Not Treated
The Play Of Genes And Non
- Department of Nutrition and Food Hygiene, School of Public Health, China Medical University, Shenyang, China
Diabetes has been a disease of public health concern for a number of decades. It was in the 1930s when scientists made an interesting discovery that the disease is actually divided into two types as some patients were insensitive to insulin treatment then. Type 2 Diabetes which happens to be the non-insulin dependent one is the most common form of the disease and is caused by the interaction between genetic and non-genetic factors. Despite conflicting results, numerous studies have identified genetic and non-genetic factors associated with this common type of diabetes. This review has summarized literature on some genes and non-genetic factors which have been identified to be associated with Type 2 diabetes. It has sourced literature from PubMed, Web of Science and Medline without any limitation to regions, publication types, or languages. The paper has started with the introduction, the play of non-genetic factors, the impact of genes in general, and ended with the interaction between some genes and environmental factors.
Genetic Factors Affecting Type 2 Diabetes
Type 2 diabetes is the most frequent kind, accounting for 9095 percent of all diabetes cases that take place due to genes. People with type 2 diabetes, like those with type 1, probably have a close diabetic family member.
If you have type 2 diabetes, youre probably not the first person in your family to develop the disease. If a parent or sibling has the disease, youre more likely to have it. The development of type 2 diabetes is linked with several genetic factors. These gene variants can interact with each other and the environment to raise your risk.
In general, mutations in any gene involved in glucose regulation can raise your risk of developing type 2 diabetes. These genes include the regulation of
- the process of glucose production
- the production and control of insulin, and
- how the body detects glucose levels.
Type 2 includes some symptoms that develop or show diabetes genetics as:
- Urination ,
Don’t Miss: Diabetes Kidney Failure Life Expectancy
What Treatments Are Available For Type 2 Diabetes
While there is no cure for type 2 diabetes, treatments are available to help you manage the disease. These include medications, insulin therapy, and lifestyle changes. Medications used to treat type 2 diabetes include those used for glucose control, aspirin to help prevent cardiovascular disease, and blood pressure medications. Insulin therapy, such as insulin injections or an insulin pump, is also a common treatment for type 2 diabetes and may be needed if you are unable to control your blood glucose levels with medications alone. Lifestyle changes that can help manage type 2 diabetes include eating a healthy diet, exercising regularly, and maintaining a healthy weight. If you have difficulty making these changes on your own, there are many resources available to help you, including diabetes education classes, support groups, and online tools.