What Do The New Diabetes Guidelines Of Acp Suggest
The American College of Physicians has issued some diabetes recommendations for patients across the world. These new diabetes recommendations are mainly focused on a protein known as haemoglobin HbA1c or A1C, which has been the biggest measurement for diabetes patients to ascertain their average blood sugar levels.
It is worth mentioning that sugar or glucose binds to haemoglobin while travelling through to the bloodstream of a patient.
Also Read:6 Surprising Benefits of Sabja Seeds
Standard : Dsmes Team
All members of a DSMES team will uphold the National Standards and implement collaborative DSMES services, including evidence-based service design, delivery, evaluation, and continuous quality improvement. At least one team member will be identified as the DSMES quality coordinator and will oversee effective implementation, evaluation, tracking, and reporting of DSMES service outcomes.
The DSMES team may include one or a variety of healthcare professionals. The evidence recommends that inclusion of dietitians, nurses, pharmacists, or all other disciplines with special certifications that demonstrate mastery of diabetes knowledge and training, such as Board Certified in Advanced Diabetes Management and Certified Diabetes Care and Education Specialists , can support all DSMES services, including clinical assessment .
To maintain competence and expertise in the expanding diabetes care and education services, all DSMES team members are required to participate in and have documented continuing education, specific to the role they serve within the team . For services outside of the scope of practice of the DSMES team or services, the DSMES team should document communication with referring physicians/other qualified healthcare professionals to support person-centered care.
Dietary And Lifestyle Management
Dietary advice for people with diabetes and CKD should include consumption of a balanced, healthy diet that is high in vegetables, fruits, whole grains, fiber, legumes, plant-based proteins, unsaturated fats, and nuts and lower in processed meats, refined carbohydrates, and sweetened beverages. Nutritional recommendations may have to be adjusted for conditions such as hyperkalemia as well as personal and cultural preferences. Daily dietary protein intake should be maintained at 0.8 g per kg, which is recommended for all people. Neither higher- nor lower-protein diets are advised, although people on dialysis should have daily dietary protein intake of 1.0 to 1.2 g per kg to offset muscle catabolism. Sodium intake should be limited to less than 2 g per day or less than 5 g of sodium chloride.
Lower levels of physical activity are common and associated with worse clinical outcomes. Moderate-intensity physical activity for at least 150 minutes per week and reduction in sedentary activity are recommended.
In addition to further increasing cardiovascular risk, cigarette smoking is associated with kidney disease progression, and patients should be advised to quit smoking.
Don’t Miss: Diabetes Feet Tingling At Night
Acp Recommends Moderate Blood Sugar Control Targets For Most Patients With Type 2 Diabetes
Philadelphia, March 6, 2018 Patients with type 2 diabetes should be treated to achieve an A1C between 7 percent and 8 percent rather than 6.5 percent to 7 percent, the American College of Physicians recommends in an evidence-based guidance statement published today in Annals of Internal Medicine.
An A1C test measures a persons average blood sugar level over the past two or three months. An A1C of 6.5 percent indicates diabetes.
ACPs analysis of the evidence behind existing guidelines found that treatment with drugs to targets of 7 percent or less compared to targets of about 8 percent did not reduce deaths or macrovascular complications such as heart attack or stroke but did result in substantial harms, said Dr. Jack Ende, president, ACP. The evidence shows that for most people with type 2 diabetes, achieving an A1C between 7 percent and 8 percent will best balance long-term benefits with harms such as low blood sugar, medication burden, and costs.
ACP recommends that clinicians should personalize goals for blood sugar control in patients with type 2 diabetes based on a discussion of benefits and harms of drug therapy, patients preferences, patients general health and life expectancy, treatment burden, and costs of care.
More than 30 million Americans have diabetes, and 90 percent to 95 percent of them have type 2 diabetes. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it.
Approved Weight Loss Medications
Nearly all FDA-approved medications for weight loss have been shown to improve glycemic control in patients with type 2 diabetes and delay progression to type 2 diabetes in patients at risk. Medications approved by the FDA for the treatment of obesity are summarized in Table 8.2 in the complete 2022 Standards of Care.
You May Like: Do I Have Type 2 Diabetes
Standards Of Medical Care In Diabetes2022 Abridged For Primary Care Providers
American Diabetes Association Standards of Medical Care in Diabetes2022 Abridged for Primary Care Providers. Clin Diabetes 1 January 2022 40 : 1038.
The American Diabetes Associations Standards of Medical Care in Diabetes is updated and published annually in a supplement to the January issue of Diabetes Care. The Standards are developed by the ADAs multidisciplinary Professional Practice Committee, which comprises expert diabetes health care professionals. The Standards include the most current evidence-based recommendations for diagnosing and treating adults and children with all forms of diabetes. ADAs grading system uses A, B, C, or E to show the evidence level that supports each recommendation.
-
AClear evidence from well-conducted, generalizable randomized controlled trials that are adequately powered
-
BSupportive evidence from well-conducted cohort studies
-
CSupportive evidence from poorly controlled or uncontrolled studies
-
EExpert consensus or clinical experience
Ace Inhibitors And Angiotensin Receptor Blockers Are Recommended For Hypertension In People With Type 2 Diabetes And Coronary Artery Disease
ACE inhibitors and ARBs are used to reduce blood pressure in people with diabetes. ADA is now recommending these medications as the first line of defense for high blood pressure in people with coronary artery disease.
During pregnancy, the recommended blood pressure target was reduced to 110-135/85 mmHg, to reduce the risk of hypertension associated with pregnancy.
These updates are posted in chapter 10 of the 2021 ADA Standards of Care.
Also Check: Does High Blood Sugar Mean You Are Diabetic
How Are New Diabetes Recommendations Different From The Older Ones
The new ACP recommendations clearly contradict decades old beliefs and diabetes guidelines that suggested that if a patient has an HbA1c level of over 7 percent, he/she is at an elevated risk of suffering from severe diabetes complications, like diabetic retinopathy and neuropathy.
People who have not been diagnosed with diabetes have their HbA1c level below 5.7 percent, while the healthiest people measure even below 5 percent, which means that their blood sugar would very rarely have gone lower or higher than the 70 to 130 mg/dl range.
The doctors, for diagnosis purposes, suggest that a person whose HbA1c levels is higher than 5.7 percent, he/she is suffering from prediabetes, and if the HbA1c level is above 6.5 percent, it means that the person is diabetic.
Interestingly, ACP believes that people intentionally allow their blood sugar levels to stay high constantly to measure an HbA1c level between 7 and 8 percent, which clearly translates into blood sugar levels being between 150 and 200 mg/dl, which is way above the healthy limits.
Well, ACP is suggesting to aim for higher blood sugar targets because the studies have shown inconsistency in people showing complications when their HbA1c was in this higher range. The complications only appeared among the patients who had an excess amount of protein in their urine, meaning a pre-existing kidney disease.
Summary
Prediabetes And Type 2 Screening Should Start At Age 35
The ADA now recommends that adults who do not have diabetes symptoms should be screened for prediabetes and type 2 diabetes starting at age 35. This change comes after the US Preventive Services Task Force lowered its recommended screening age from 45 to 35 years in August, 2021. Of the estimated 34 million US adults with diabetes in 2018, about one in five was undiagnosed. The CDC estimates that 88 million people in the US have prediabetes and that most of them dont know it and have not been made aware by their healthcare providers.
The prevalence of diabetes is rising there are many people with type 2 diabetes who are undiagnosed, and it is occurring at younger and younger ages, said Gabbay. I saw a patient who was diagnosed with diabetes after seeing his eye doctor, who determined that he already had significant retinopathy, eventually losing vision in one eye. He presumably had diabetes for a number of years but never knew it. This should not have to happen, which is why this change is important.
The guidelines also added new screening recommendations for pregnant women and those planning a pregnancy. Those at risk for diabetes who are planning to become pregnant should be screened before conception or, if not screened before conception, before they are 15 weeks pregnant. The standards also urge healthcare professionals to consider screening all those who are currently pregnant or planning to become pregnant regardless of diabetes risk.
Also Check: Patho Of Type 2 Diabetes
Healthcare Providers Are Encouraged To Individualize Diabetes Care
While the Standards focus on general protocols for treating all people with diabetes, they stress the importance of individualized care based on peoples unique needs.
Putting the person, rather than their diabetes, at the center of healthcare can help improve person-provider relationships as well as physical and mental health outcomes, and it can reduce the stigma people with diabetes experience in healthcare.
Diet Physical Activity And Behavioral Therapy
Recommendations
8.5 Diet, physical activity, and behavioral therapy to achieve and maintain 5% weight loss is recommended for most people with type 2 diabetes and overweight or obesity. Additional weight loss usually results in further improvements in control of diabetes and CV risk. B
8.6 Such interventions should include a high frequency of counseling and focus on dietary changes, physical activity, and behavioral strategies to achieve a 500750 kcal/day energy deficit. A
8.9 Evaluate systemic, structural, and socioeconomic factors that may impact dietary patterns and food choices, such as food insecurity and hunger, access to healthful food options, cultural circumstances, and SDOH. C
8.10 For those who achieve weight loss goals, long-term weight maintenance programs are recommended when available. Such programs should, at minimum, provide monthly contact and support, recommend ongoing monitoring of body weight and other self-monitoring strategies, and encourage regular physical activity . A
8.11 Short-term dietary intervention using structured, very-low-calorie diets may be prescribed for carefully selected individuals by trained practitioners in medical settings with close monitoring. Long-term, comprehensive weight maintenance strategies and counseling should be integrated to maintain weight loss. B
8.12 There is no clear evidence that dietary supplements are effective for weight loss. A
You May Like: Once Per Week Diabetes Injection
New Diabetes Guideline Reflects Change In Glucose Therapy Considerations
We were unable to process your request. Please try again later. If you continue to have this issue please contact .
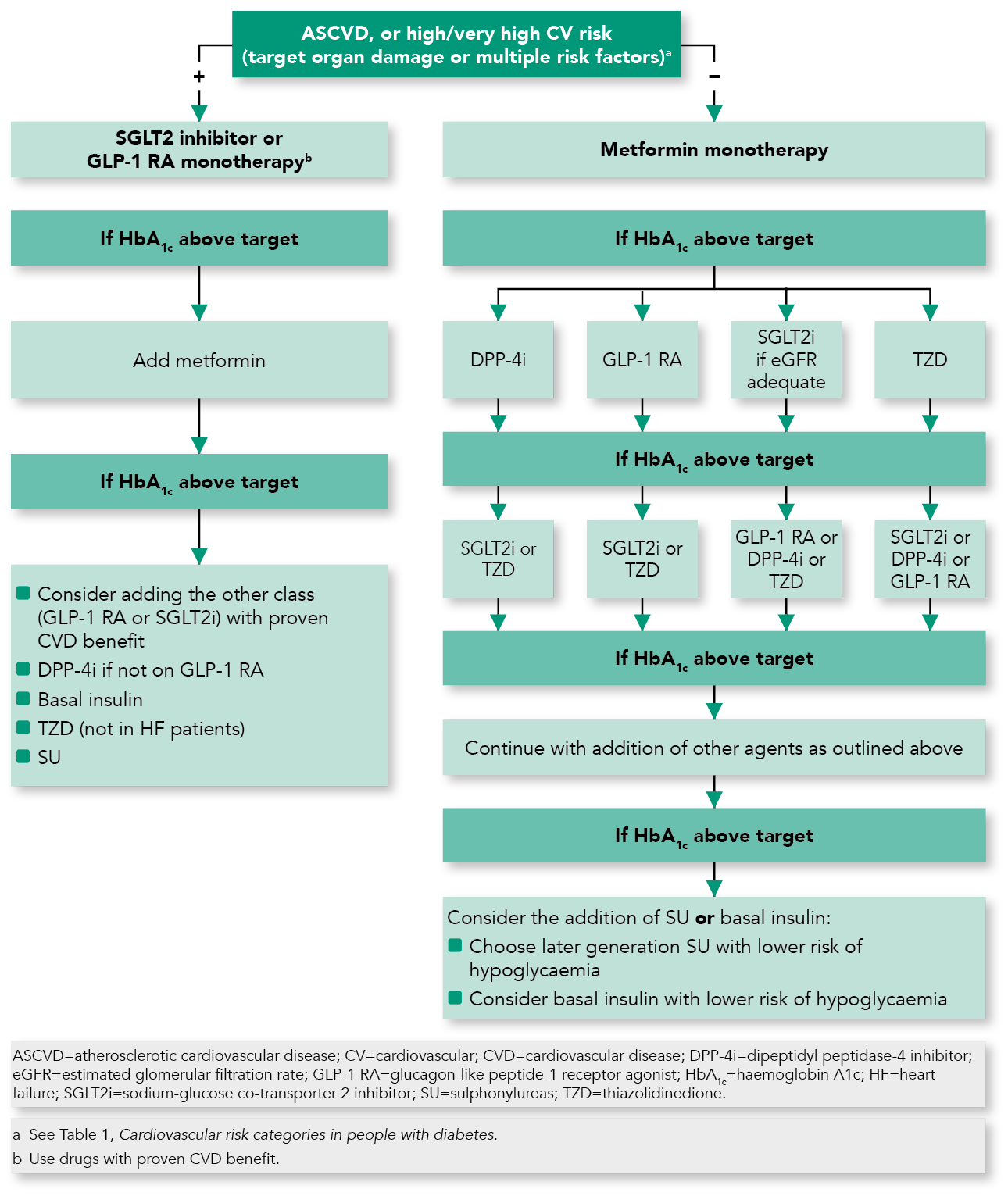
The American Diabetes Association recently published its 2020 Standards of Medical Care in Diabetes. Perhaps one of the most important updates in the guidance for primary care physicians is that medications that have evidence of improving cardiovascular and renal outcomes are now recommended in at-risk patients independent of the need for additional glucose lowering, an expert told Healio Primary Care.
The recommendations given a grade of A, B, C or E, depending on the level of evidence behind each recommendation also provide insight on managing CVD and strategies for following the chronic care model.
Data indicate that PCPs treat at least 90% of the 24 million patients in the United States with diabetes. Healio Primary Care interviewed several experts about the most important takeaways from the guideline for PCPs.
Adding glucose therapies
In the past, the ADA has recommended adding glucose-lowering therapies to regimens to lower A1C levels in patients who were at risk for CVD or renal disease, according to Joshua J. Neumiller, PharmD, chair of the ADAs Professional Practice Committee, which oversees annual updates to the Standard of Care.
Some other recommendations related to glucose assessment include:
Kevin M. Pantalone
Neumiller added that the Standards of Care provides several tools to help PCPs with these recommendations.
Managing CVD
Randy Wexler
Cvd And Risk Management
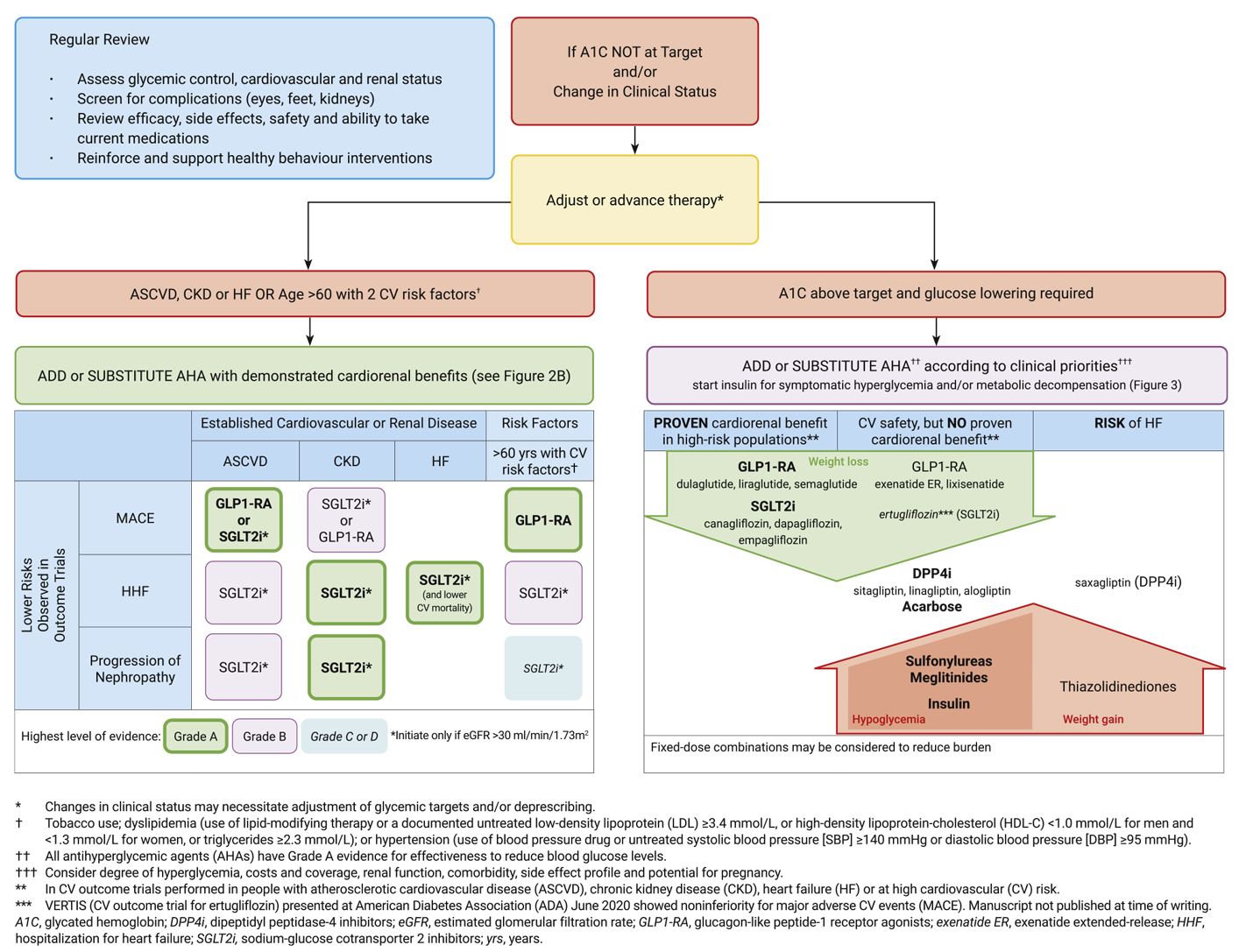
ASCVDdefined as coronary heart disease, cerebrovascular disease, or peripheral arterial disease presumed to be of atherosclerotic originis the leading cause of morbidity and mortality for individuals with diabetes. Controlling individual CV risk factors helps prevent or slow ASCVD in people with diabetes. HF is another major cause of morbidity and mortality from CVD. Studies show HF is twofold higher in people with diabetes compared to those without.
Risk factors, including duration of diabetes, obesity/overweight, hypertension, dyslipidemia, smoking, a family history of premature coronary disease, CKD, and the presence of albuminuria, should be assessed at least annually in all patients with diabetes to prevent and manage both ASCVD and HF.
Don’t Miss: Mens Low Cut Diabetic Socks
Management Of Diabetes In Pregnancy
The prevalence of diabetes in pregnancy has been increasing in the United States in parallel with the worldwide epidemic of obesity. Specific risks of diabetes in pregnancy include spontaneous abortion, fetal anomalies, preeclampsia, fetal demise, macrosomia, neonatal hypoglycemia, hyperbilirubinemia, and neonatal respiratory distress syndrome, among others. Diabetes in pregnancy may increase the risk of obesity, hypertension, and type 2 diabetes in offspring later in life.
Diabetes Technology Use In Hospitals
Before the COVID-19 pandemic, people with diabetes were not always allowed to use their CGMs, insulin pumps, and AID systems while hospitalized, but the guidelines for using these devices have become more flexible in recent years to prevent the spread of COVID-19, though they vary from institution to institution. Its important for people with diabetes and their loved ones to continue to advocate for the use of these technologies in hospitals.
The ADAs 2022 guidelines discuss in-hospital technology use for all people who are able to safely use their devices in the hospital setting.
The ADA also lowered the age to screen for prediabetes and type 2 diabetes to 35 years, encouraged healthcare providers to individualize care, and recommended COVID-19 vaccines for all adults with diabetes.
You May Like: Can Someone With Type 1 Diabetes Join The Military
Why New Guidelines For The Prevention And Management Of Diabetes
It is a very exciting time for diabetes care and education and Canada! In early April, Diabetes Canada released the 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. More importantly, many new tools and resources have also been developed to assist healthcare professionals to individualize patient care, provide diabetes self-management education, and set and support goals with a diabetes action plan.
Still other tools for patients have been developed to provide guidance for you as you work toward becoming diabetes self-managers! It is very exciting with this set of guidelines to see an increased awareness of effective screening for and treatment of diabetes, guidance on complication screening and prevention, the role of diabetes self-management education and support, goal setting, assessment of diabetes-related stress, and awareness of the importance of the diabetes healthcare team.
National Standards For Diabetes Self
Diabetes Care
Jody Davis, Amy Hess Fischl, Joni Beck, Lillian Browning, Amy Carter, Jo Ellen Condon, Michelle Dennison, Terri Francis, Peter J. Hughes, Stephen Jaime, Ka Hei Karen Lau, Teresa McArthur, Karen McAvoy, Michelle Magee, Olivia Newby, Stephen W. Ponder, Uzma Quraishi, Kelly Rawlings, Julia Socke, Michelle Stancil, Sacha Uelmen, Suzanne Villalobos 2022 National Standards for Diabetes Self-Management Education and Support. Diabetes Care 1 February 2022 45 : 484494.
The National Standards define timely, evidence-based, quality DSMES services that meet or exceed the Centers for Medicare & Medicaid Services quality standards. While the acronym DSMES is used in the literature and in current practice, it is important to note that the term diabetes self-management training is exclusively used when describing the Medicare benefit for diabetes self-management. The Medicare benefit for DSMT was established by the Balanced Budget Act of 1997 with a final rule published on 29 December 2000, implementing the BBA provisions and DSMT regulations . The DSMT benefit has reimbursement guidelines outside of the National Standards.
Don’t Miss: Renal Cysts And Diabetes Syndrome
Standard : Delivery And Design Of Dsmes Services
DSMES services will utilize a curriculum to guide evidence-based content and delivery, to ensure consistency of teaching concepts, methods, and strategies within the team, and to serve as a resource for the team. DSMES teams will have knowledge of and be responsive to emerging evidence, advances in education strategies, pharmacotherapeutics, technology-enabled treatment, local and online peer support, psychosocial resources, and delivery strategies relevant to the population they serve.
The options for delivery of DSMES have grown dramatically in recent years as technology has been incorporated into healthcare, and simultaneously as more people have become comfortable using technology for communication, teaching, and learning. Various modes of delivery can support increased communication between PWD and the DSMES team and improve diabetes-related outcomes. Strong evidence supports DSMES delivery through virtual, telehealth, telephone, text messaging, and web-based/mobile phone applications .
Pathophysiology of diabetes and treatment options
Healthy coping
Reducing risk
Problem solving and behavior change strategies
DSMES follow-up and ongoing support
Return To Care Letter Template
Research shows Canadians access to the health-care system has changed over the course of the pandemic and that many patients have not sought care when probably they should have. For people living with diabetes, delayed or deferred care can contribute to a higher risk of short- and long-term complications which, in time, may lead to poorer outcomes.
Diabetes Canada has created a letter that you can send to your patients to help facilitate a reconnection and encourage the return to regular diabetes appointments. Routine check-ins will help decrease the likelihood of adverse health impacts to your patients. You can customize the template or send it as is. The letter is available in English, French, Simplified Chinese and Punjabi.
Recommended Reading: Where Can I Put My Insulin Shot