Research Design And Methods
Eight- to 10-week-old db/db mice were fed normal chow and underwent SG or sham surgery wherein the mouse stomach was exposed and a 12-mm clip placed by using a LIGACLIP Multiple Clip Applier horizontally across the greater curvature of the stomach. The excluded part of the stomach was excised. Sham surgeries included the abdominal incision and closure of body wall and skin. Mice were fasted the day before surgery and the day of surgery and then returned to normal chow. Lean controls were db/+ littermates of the db/db experimental group.
Clamp studies, triglycerides, cholesterol, and nonesterified fatty acid measurements were performed by the mouse phenotyping core of the Diabetes Research Center at the University of Pennsylvania. The joint ethics committee of the Hebrew University and Hadassah Medical Center and the institutional animal care and use committee of the University of Pennsylvania approved the animal experiments carried out in Jerusalem and Philadelphia, respectively. Values shown are mean ± SEM. See the Supplementary Data for additional information.
When Is Surgery Recommended
Bariatric surgery is available on the NHS for people who meet certain criteria. These include:
- you have a BMI of 40 or more, or a BMI between 35 and 40 and an obesity-related condition that might improve if you lost weight
- you’ve tried all other weight-loss methods, such as dieting and exercise, but have struggled to lose weight or keep it off
- you agree to long-term follow-up after surgery such as making healthy lifestyle changes and attending regular check-ups
How Does Sleeve Gastrectomy Act
During the procedure, approximately 85% of the stomach is removed in such a way as to remain only a thin tube-like stomach with a thickness equal to that of your thumb. Thus, the amount of food that can be consumed at a time is considerably reduced so that the patient feels satiety earlier. This is the restrictive effect of the procedure.However, sleeve gastrectomy is not only a restrictive operation, but also a procedure with hormonal and metabolic effects. The removed part of the stomach is the part that produces the hunger-triggering hormone Ghrelin. Removal of this part reduces the amount of appetite-inducing hormone in the blood, and generally leads to suppressed appetite.Since the natural mechanism of the digestive system is not intervened in, digestion and absorption functions continue normally after sleeve gastrectomy. Therefore, it poses a much lower risk of vitamin and mineral deficiencies in comparison with surgical procedures that intervene in absorption.
Read Also: How Much Is Insulin At Walmart
Description Of Surgical Procedures And Their Rationale
The major distinction between bariatric procedures relies on their mechanisms of action and comprises purely restrictive, malabsorptive or combination techniques. Of note, the length of the upper gastrointestinal tract bypass is thought to play a major role in determining the magnitude of weight loss and metabolic outcomes . Among various techniques, the following four are the most studied in terms of safety and efficacy to promote weight loss and improve metabolic state and overall health .
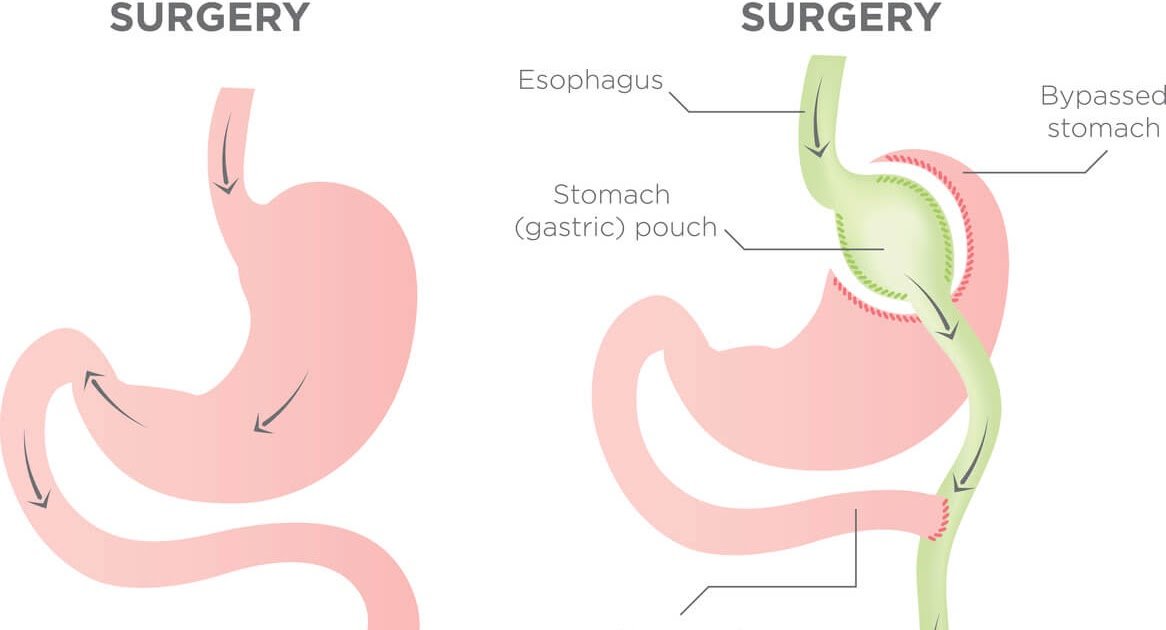
Fig. 1
Graphical presentation of the four best established and standardized types of bariatric surgery. a Laparoscopic adjustable gastric banding, b Roux-en-y gastric bypass, c Vertical sleeve gastrectomy and d Biliopancreatic diversion
Laparoscopic adjustable gastric banding involves encircling the upper part of the stomach with a silicone adjustable band with an inflatable balloon at the inner surface connected with a port placed subcutaneously, through which pressure on the vagal afferent intraganglionic laminar endings can be adjusted by adding or retracting fluid .
Who Is A Candidate For Diabetes Surgery
A great deal of scientific evidence supports the use of diabetes surgery in patients with BMI of 30 and greater. If you have type 2 diabetes and a BMI of 30 and above, you may qualify for diabetes treatment through surgery. The decision to pursue surgery is made on an individual basis and you can work with your doctors to determine if surgery is a good choice to treat your diabetes.
Want to know more? Read Who is a Candidate for Surgery?
You May Like: How To Get Rid Of Diabetes Stomach Fat
Will Insurance Cover It
Many insurance companies do cover weight loss surgery, since studies show that weight loss surgery could help treat type 2 diabetes.
Your insurance company may ask you to go on a weight loss program first. This will show that you tried to lose the weight before choosing surgery.
If you donât have coverage, the surgery can cost between $11,500 and $26,000. You can deduct it from your federal income taxes.
How Does Bariatric Surgery Affect Blood Sugar Levels
Stacy Brethauer, MD, a surgeon at The Ohio State University Wexner Medical Center in Columbus, says that bypass operations stimulate increased production of gut hormones that regulate the appetite. According to an article published in May 2018 in Surgery for Obesity and Related Diseases, those hormones include glucagon-like peptide-1 and peptide-YY . Anytime you deliver nutrients to the bottom part of the bowel more quickly, which is what you do with those operations, it stimulates the bowel to produce more of those hormones, Dr. Brethauer says.
GLP-1 causes your pancreas to produce more insulin after you eat, thereby helping with blood sugar control, according to the Hormone Health Network. Brethauer notes that popular oral diabetes drugs known as GLP-1 receptor agonists brands include Victoza and mimic the action of GLP-1 in the body and help to keep your blood sugar from rising too high. Meanwhile, the small intestine produces PYY before releasing it into the bloodstream after you eat. This hormone tells your brain when youve eaten enough, helping you feel full and curbing overeating, per the Hormone Health Network.
Altered gut hormones also may be the cause of a rare complication of bypass surgeries, particularly Roux-en-Y procedures, known as postprandial hyperinsulinemic hypoglycemia, or severely low blood sugar after eating, according to a position statement published in December 2017 in Surgery for Obesity and Related Diseases.
Read Also: Lantus Insulin Patient Assistance Program
Glucose Homeostasis After Bariatric Surgery And Special Concerns In T1dm
As bariatric surgery has only recently been considered as a therapeutic option for T1DM, evidence concerning the possible mechanisms through which it impacts glucose metabolism has been obtained from studies on human and animal models with T2DM. Weight loss, calorie restriction and gastrointestinal hormone modulation are some of the mechanisms which have been described to play an important role in the remission of T2DM after bariatric surgery . The effect of these mechanisms in T1DM has not yet been elicited due to the different pathogenesis comparing to T2DM. However, the fact that bariatric surgery results in a significant reduction of insulin requirements and an, at least modest, reduction in HbA1c in T1DM patients, implies the existence of a shared background between these two types of the disease on which surgery exerts mutually beneficial effects. The discrepancies, nevertheless, in the post-operative glycemic control in T1DM are a serious concern that needs to be elucidated. To discuss these concerns, a brief presentation of the main mechanisms through which surgery acts on glucose metabolism is required.
How To Treat Diabetes From The Inside Out
Each intervention contact focused on a behavioral topic related to weight loss. After three years, 40 percent of the bypass subjects were in remission from type 2 diabetes or had prediabetes, as were 29 percent of the lap band participants. None of the people who lost weight from intensive lifestyle changes were in remission or had prediabetes.
After three years, participants who underwent surgery were less reliant on medication, while medication use did not change among the lifestyleweight loss group. Of those who were using meds at baseline, 65 percent of the bypass group and 33 percent of the lap band group had ceased using diabetes medication.
Don’t Miss: Are Omelettes Good For Diabetics
How Does Bariatric Surgery Cure Type 2 Diabetes
We know that bariatric surgery puts type 2 diabetes into remission what we dont know is how it does it.
It’s clear that healthy weight loss plays a significant role in reducing blood sugar levels in Type 2 diabetics, and bariatric surgery has been proven to be the most effective way for obese patients to lose significant body weight.
But, there are additional factors at work. Many see an instant reversal of their diabetes immediately after gastric bypass surgery or gastric sleeve surgery before they lose any weight. This is what science doesn’t fully understand.
One theory suggests that bypassing or removing part of the stomach immediately impacts the way glucose is processed in the digestive system. Another claims that by shunting food directly to the lower intestine, a substance called glucagon-like peptide 1 is stimulated, which can increase insulin production. Scientists also speculate that hormones that prompt hunger such as peptide Y may be dulled by rearranging the anatomy of the gut. In other words, if people crave less sugar, they may be able to manage their blood sugar levels better.
In any case, study after study has shown that bariatric surgery is much more effective than drug therapy alone in the management of diabetes. Long term studies show that even in the cases where patients don’t achieve remission, their glucose levels are lower than those who don’t undergo surgery.
What Are The Chances That Bariatric Surgery Will Help In My Case
This is what a review of over 620 scientific studies involving more than 100,000 patients has found: Gastric bypass surgery causes an improvement in glucose levels in virtually all cases, and full remission in 80%. Some types of bariatric surgery are more effective than others. Gastric banding, known popularly as the “Lap Band”, is the least effective, with remission rates of 50-60%, while the seldom used biliopancreatic diversion, usually reserved for the most extreme cases of obesity, has remission rates of 95%. The effects of the sleeve gastrectomy, or the gastric sleeve, is less known, but recent studies suggest that it achieves remission rates of 80% — similar to the gastric bypass.
The chance of achieving full remission depends on the severity of the disease and how long you’ve had it. A key finding in all studies is that the less time you suffer from diabetes, the more likely you’ll achieve a full reversal. Patients who have pre-diabetes those on the cusp of developing the disease achieve remission in almost all cases. Patients with severe diabetes, those who take insulin, have lower remission rates than those who only take oral medications.
The question of whether remission can be permanent is still unknown, but recent studies suggest that the benefits can be long-lasting, and that maintenance of a healthy body weight plays an important role.
Also Check: Type 1 Diabetes Immune System
Sleeve Gastrectomy Has Fewer Complications
There is ample evidence that SG has fewer post-surgical adverse events, including a new study that found interventions, hospitalizations, and complications were more common with RYGB than SG. There are clear tradeoffs between benefits and risks, says Arterburn. We have to approach this as a classic situation where you need to do good shared decision-making. People lose more weight and have better diabetes control long term with RYGB. But it is much safer to get a sleeve. Every patient has to weigh that. If a patient is really worried about safety, an informed patient might be more inclined to get a sleeve.
However, if you are having major abdominal surgery anyway, and a sleeve is more likely to result in having another surgery down the line, perhaps the better option is traditional bypass and a procedure that makes the most difference, he notes.
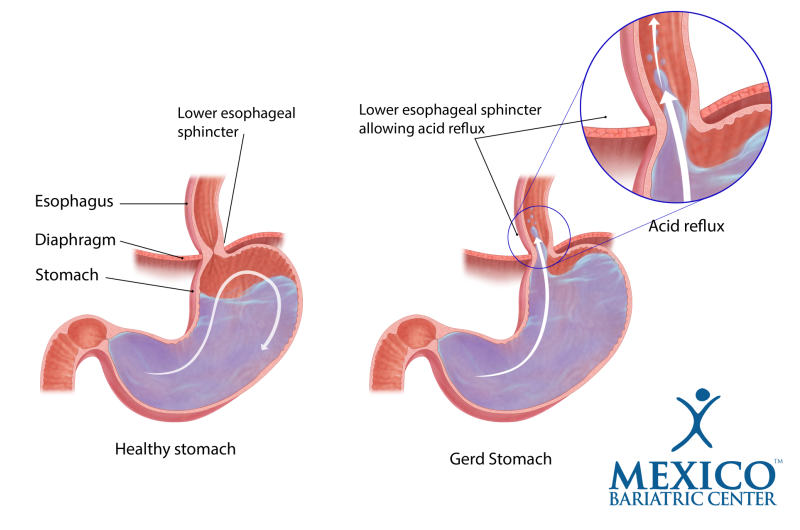
Another factor in the decision is whether the patient has gastroesophogeal reflux . Patients with GERD who are so affected they take medications are more likely to see the condition worsen after a sleeve procedure, Arterburn notes. They sometimes end up having to have further surgery to switch to a bypass, while the bypass itself can reduce reflux symptoms.
Pathophysiology Of Weight Loss And T2dm Remission After Bariatric Surgery
Metabolic surgery is able to induce and maintain substantial weight loss through a variety of mechanisms, including caloric restriction as a result of the anatomical remodelling of the gastrointestinal tract, increased meal-induced thermogenesis, modulation of hypothalamic neuronal circuits involved in energy balance and appetite regulation, altered taste, food preferences and eating behaviour patterns, as well as altered gut-brain signalling pathways .
With regard to amelioration of the metabolic milieu leading to T2DM remission, the beneficial effects of metabolic surgery are mediated to a significant extent by two important factors the hypocaloric state due to profound caloric restriction, and the significant weight loss achieved. Studies involving patients with T2DM have demonstrated that caloric restriction to the extent observed during the first 10 to 20 days after RYGB has the same immediate effect on insulin sensitivity and blood glucose levels as surgery . However, there is no enhanced incretin effect with caloric restriction alone, and it is essentially impossible for people with obesity and diabetes to maintain this drastic restriction for a prolonged period of time.
Read Also: Grams Of Sugar Per Day For Diabetic
Am I Eligible For Sleeve Gastrectomy
If according to the criteria of the International Federation for the Surgery of Obesity & Metabolic Disorders you have a weight problem within the surgical limit, if you currently have vitamin-mineral deficiencies that may cause problems with bypass and other procedures, if you have a disorder requiring the use of Prednisolone or an anti-inflammatory drug that may cause a problem during bypass surgery, if you have Crohns disease or a story of abdominal surgery, if you have heart or lung problems that may cause a problem with an operation that takes a long time, and if you are at the threshold of super morbid obesity, sleeve gastrectomy will definitely be suitable for you as the first option. The age range suitable for sleeve gastrectomy is 12 to 79 years of age.
Should Everyone With Diabetes Undergo Bariatric Surgery
Not necessarily, says Hutcher. This decision is up to the patient and the physician, but no obese patient with diabetes should be denied access to this surgery, he adds.
The bottom line is that bariatric surgery can play a big role in treating diabetes, according to Ren. If you lose weight, your diabetes will go away, and when you regain the weight, the diabetes will come back, she says. Diabetes is always lurking, and remission lasts as long as the weight loss lasts.
You May Like: Best Fiber Supplement For Diabetics
How Is The Cost Of Sleeve Gastrectomy
The cost of Sleeve Gastrectomy in the United States ranges from 13,000 to 30,000 USD. Many insurance companies have included these surgical procedures in their insurance coverage. Unfortunately, private insurance companies in our country are still insisting on keeping bariatric surgery out of their insurance coverage. On the other hand, the social security institution makes a payment that does not cover even the cost of the device used in such operations.
Address
Does Bariatric Surgery Treat Type 2 Diabetes
Doctors have found that weight-loss surgery can treat type 2 diabetes by controlling the level of sugar in the blood. Diabetes is a disease that happens when blood sugar levels are too high. Blood sugar is the primary source of energy for your cells. The glucose is able to get into cells because of the hormone called insulin. Insulin is made by the pancreas.
If your body does not make insulin or make enough insulin, the glucose cannot get to your cells and so stays in the blood. This situation, if it lasts a long time, can cause certain health problems. Complications of diabetes can be very serious. They can affect the eyes, kidneys and nerves.
Obesity is an important factor in developing diabetes. People who are severely obese have 10 times the risk of developing the disease. Foods that are high in fats and carbohydrates increases fatty acids in the blood and lipid build-up in the liver and muscles. This increases insulin resistance and inflammation. Over time, the pancreas stops making enough insulin.
Weight-loss surgery is also called bariatric surgery. There are several types. Most of the procedures can be done in a minimally invasive way, via laparoscopy. Laparoscopic surgeries involve only small incisions and very tiny instruments.
Read Also: Best Cookbook For Type 1 Diabetes
Unveiling The Magic Of Diabetes Remission After Weight
An extraordinary thing happens to some patients with type 2 diabetes who undergo weight-loss surgery: Within days of the procedure, they improve their insulin production and need fewer or no diabetes medications. Although its well established that losing weight, especially around the waistline, improves pancreas function and insulin sensitivity, it generally takes 6 months to a year after bariatric surgery before a patient sheds a substantial number of pounds. Bruce M. Wolfe, MD, professor of surgery at Oregon Health and Science University School of Medicine, recalled one remarkable case in which a patient who required 400 daily units of insulin prior to gastric bypass surgery needed none on the day she was discharged from the hospital.Continue reading > >
Outcomes In Weight Loss
Bariatric surgery offers a significant reduction in body mass index in patients with obesity and T1DM which is sustained in long term. Czupryniak et al. were the first to show a marked improvement in the mean BMI of three women with obesity who underwent RYGB from 42.2 kg/m2 preoperatively to 33.5 kg/m2 post-operatively in a follow-up period of ~7 years. After an ~3-years follow-up time, mean reductions in BMI were 11.1, 8.3, and 9.4 kg/m2 in other cohorts . In a relatively large cohort of 32 subjects with obesity studied for 4.6 years, the mean percentage of total weight loss at 12 months after surgery was 30.4%, with a slight decrease at 5 years, reaching 28.1% . Cumulatively, a meta-analysis by Chow et al. , including 86 patients in total, showed a reduction in BMI of 13.42 kg/m2 post-operatively. Another meta-analysis by Ashrafian et al. , including 142 patients in total, showed a mean BMI decrease of 11.04 kg/m2, in a mean follow-up time of 31.8 months. In general, similar results have been demonstrated by every study on the field regardless of the type of intervention applied, the number of patients or the follow-up period .
Also Check: What Is The Average Cost Of An Insulin Pump