Genetics Of Type 1 Diabetes Comes Of Age
Diabetes Care
Maria J. Redondo, Patrick Concannon Genetics of Type 1 Diabetes Comes of Age. Diabetes Care 1 January 2020 43 : 1618.
Younger age at diagnosis often reflects a greater influence of genetic factors in disease. Type 1 diabetes, which develops most frequently in childhood but can also present in adult life, is a prime candidate to explore the relationships among risk loci, age at diagnosis, and genetic contribution to disease. Type 1 diabetes genetic risk scores are inversely correlated with age at diagnosis. Studies have suggested age-related heterogeneity in the association of established risk alleles with type 1 diabetes, although no consistent pattern has developed. Further investigations into the genetic factors that influence age of clinical onset may refine our understanding of type 1 diabetes pathogenesis and provide opportunities for individualized preventive therapies.
The Role Of Autoantibodies In The Development Of T1d
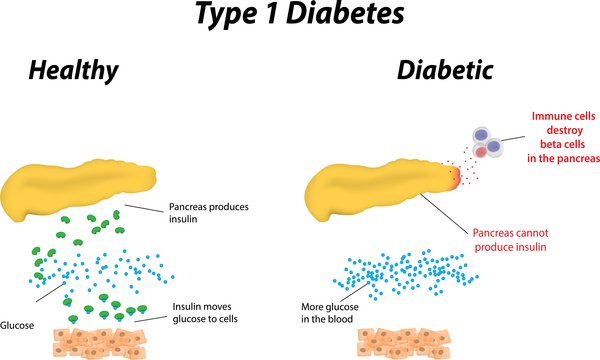
During the immune activation and immune response involved in T1D, the immune system mistakenly attacks cells in the pancreas , leading to the development of a single diabetes-related autoantibody . Almost all individuals who develop two or more of these diabetes-related autoantibodies will eventually be diagnosed with T1D . But TrialNet is working to change that.
The Role Of Genetics In Type 2 Diabetes
If youve been diagnosed with type 2 diabetes, theres a good chance that youre not the first person with diabetes in your family. Youre more likely to develop the condition if a parent or sibling has it.
Several gene mutations have been linked to the development of type 2 diabetes. These gene mutations can interact with the environment and each other to further increase your risk.
Type 2 diabetes is caused by both genetic and environmental factors.
Scientists have linked several gene mutations to a higher diabetes risk. Not everyone who carries a mutation will get diabetes. However, many people with diabetes do have one or more of these mutations.
It can be difficult to separate genetic risk from environmental risk. The latter is often influenced by your family members. For example, parents with nutrient-dense and balanced eating habits are likely to pass them on to the next generation.
On the other hand, genetics plays a big part in determining weight. Sometimes behaviors cant take all the blame.
Don’t Miss: Grocery Shopping List For Type 2 Diabetes
Can You Reduce Your Risk
If you have a family history of gestational diabetes or type 2 diabetes, there are ways to reduce your risk of developing the disease.
Maintain a healthy weight or lose weight. If you are overweight, particularly in the abdominal area, losing weight will reduce your risk. Even modest weight reduction, about 5% to 10% weight loss, can reduce your risk.
While weight gain is important for a healthy pregnancy, people who are pregnant should try to gain weight slowly rather than excessively. This will help prevent gestational diabetes.
Stay active. Aim to exercise at least 150 minutes per week and avoid sitting for long periods of time.
Eat more plants. Add more fruits, vegetables, legumes, nuts, seeds, and whole grains to your diet, and cut out processed, pre-packaged foods where possible.
Health maintenance and regular checkups are important. If you’ve recently gained weight or are feeling very sluggish and tired, you may be experiencing high blood sugar, which is characterized by insulin resistance.
Hypoglycemia And Diabetic Ketoacidosis
These 2 conditions are common complications of diabetes, and youll need to know how to handle them. Meet with your doctor for step-by-step instructions. You may want to bring a family member with you to the appointment so they learn the steps too.
Hypoglycemia can happen quickly and needs to be treated quickly. Its most often caused by:
- Too much insulin.
- Waiting too long for a meal or snack.
- Not eating enough.
- Getting extra physical activity.
Talk to your doctor if you have low blood sugar several times a week. Your treatment plan may need to be changed.
Diabetic ketoacidosis is a serious complication of diabetes that can be life-threatening. DKA develops when you dont have enough insulin to let blood sugar into your cells. Very high blood sugar and low insulin levels lead to DKA. The two most common causes are illness and missing insulin shots. Talk with your doctor and make sure you understand how you can prevent and treat DKA.
You May Like: What Gauge Are Insulin Needles
How Body Shape Affects Type 2 Diabetes Risk
Dr. Miller points to promising research on genetic risk scoring thats taking place through Trialnet, an international research consortium focused on type 1 diabetes that is supported by the National Institutes of Health and private organizations.
The biggest challenge in that area of research that baffles most scientists is: Why do some patients who have demonstrated positive autoantibodies not go on to develop type 1 diabetes? Miller says. Thats the area of greatest interest because if you can identify some factor in those patients that is protective, that keeps individuals with positive autoantibodies from killing off their beta cells, then perhaps you could prevent them from developing type 1 diabetes.
In the meantime, even without genetic testing, it is wise to pay attention to your family history and risk factors for diabetes. Not every case of diabetes is preventable, but neither is your DNA your destiny in every instance.
Type 1 Diabetes And Genetics Average Risks
- Mother with diabetes increases risk of diabetes by 2%
- Father with diabetes increases risk of diabetes by 8%
- Both parents with diabetes increases risk by 30%
- Brother or sister with diabetes increases risk by 10%
- Non-identical twin with diabetes increases risk by 15%
- Identical twin with diabetes increases risk by 40%
Don’t Miss: What Diet Is Best For Type 1 Diabetes
Type 1 Diabetes Genetic Risk Score
The Type 1 Diabetes Genetic Risk Score is a novel tool that can help differentiate Monogenic diabetes from type 1 diabetes in patients treated with insulin from diagnosis
The type 1 diabetes genetic risk score is a new addition to our testing pathway to identify individuals in whom genetic testing for monogenic diabetes is indicated when clinical features and autoimmune markers are equivocal. This test provides independent information to autoantibody and C-peptide testing and because it is a DNA based test the result does not change with time.
Indication of Type 1 Diabetes Genetic Risk Score:
Clinical suspicion of monogenic diabetes in patients who are currently insulin treated.
Methods:
Type 1 diabetes is a polygenic disease and common genetic variants have been identified that contribute to type 1 diabetes susceptibility. We genotype these variants and combine the risk of the individual variants that are present in a person to create a composite score that reflects an individuals genetic susceptibility to type 1 diabetes .
The likelihood of a patient having type 1 diabetes is based on the clinical information provided and the type 1 diabetes genetic risk score.
Sample types:
EDTA blood for Type 1 diabetes genetic risk score, autoantibody testing and monogenic diabetes genetic testing.
DNA for Type 1 diabetes genetic risk score and monogenic diabetes genetic testing only.
Other Things To Consider
Sometimes people who have a family history of gestational diabetes can develop diabetes during pregnancy despite their efforts to keep weight gain within a healthy range, exercise, and eat a fiber-rich diet. Do not beat yourself up if this happens.
Pregnancy hormones and insulin resistance can make controlling blood sugar in pregnancy difficult for some people with genetic risk. Your medical team will help you reach your blood sugar goals during pregnancy to make sure that you and your baby are healthy and thriving.
Once you have delivered your baby, your blood sugars should go back to normal. But it’s still important to continue to eat a well-balanced diet, maintain a healthy weight, and exercise these steps can help reduce your risk of developing type 2 diabetes later in life.
Although type 1 diabetes cannot be prevented or cured, if you are genetically predisposed to type 1 diabetes, regular vaccinations and wellness visits will be important.
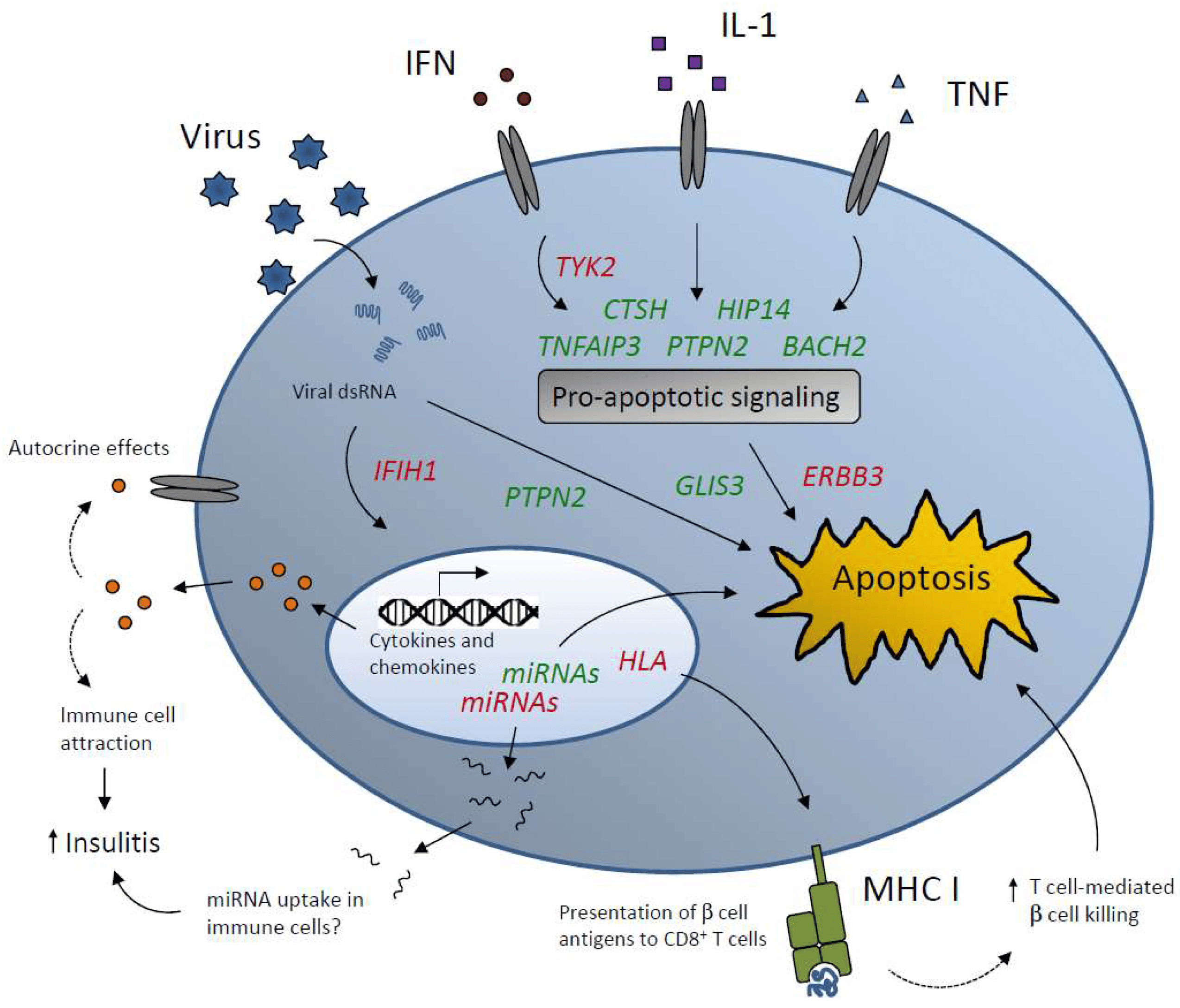
There is no vaccine to prevent type 1 diabetes, but some research suggests that viruses can trigger type 1 diabetes in people that are predisposed. Therefore, preventing catching these viruses may reduce the risk of developing diabetes.
Understanding the warning signs of type 1 diabetes will also help prevent a dangerous situation like diabetic ketoacidosis.
Read Also: Type 2 Diabetes Occurs When
Identification Of T1d Associated Snps
Single nucleotide polymorphisms associated with T1D were selected from the manually curated Catalog of Published Genome-Wide Association Studies 1 . These SNPs represent the 60 susceptibility regions that are typically associated with T1D. Equally sized sets of control SNPs were randomly selected from the SNP database using a Python script.
Type 1 Diabetes Genetics Consortium
Number of Subjects in Study Archive: 34754 Study Design: Case Control and Affected Sib Pair Conditions: Diabetes Mellitus, Type 1 Division: DEM Does it have dialysis patients: No Data Package Version Number: 7 DOI: 10.82404/3cnv-h072
How to cite this dataset: Rich, Stephen . Type 1 Diabetes Genetics Consortium . NIDDK Central Repository. https://doi.org/10.82404/3cnv-h072
Data availability statement: Data from the Type 1 Diabetes Genetics Consortium reported here are available for request at the NIDDK Central Repository website, Resources for Research , .
Read Also: Omnipod Tubeless Insulin Pump Cost
What Leads To Diabetes
Type 1 and type 2 diabetes have different causes, but there are two factors that are important in both. You inherit a predisposition to the disease, then something in your environment triggers it.
Thats right: genes alone are not enough. One proof of this is identical twins. Identical twins have identical genes. Yet when one twin has type 1 diabetes, the other gets the disease, at most, only half the time. When one twin has type 2 diabetes, the other’s risk is three in four at most.
Identifying Genetic Links To Type 1 Diabetes
Rich and his team launched this study to identify genetic factors that increase the risk of type 1 diabetes. It builds on work they have been doing for decades.
In the early 2000s, Rich formed an international multicenter group called the Type 1 Diabetes Genetics Consortium to investigate the genetics of type 1 diabetes. At that time, he and his fellow researchers had identified 15 to 18 sites in the genome associated with a genetic risk of type 1 diabetes. Studies from the consortium pinpointed about 40 sites.
In the latest study, published last June in Nature Genetics, Rich and his colleagues identified 75 to over 100 sites.
“We’ve gone from knowing about half the genetic risk of type 1 diabetes to nearly all of the genetic risk,” Rich says. “And that’s very powerful, because now we can think about how to use that information to screen populations of children for type 1 diabetes risk. Those at high genetic risk could go on to have autoantibody testing to determine whether an autoimmune process is already ongoing. If it is, we can look at how far along that autoimmune process has gone and whether we can do anything about it.”
You May Like: Swelling Of Feet And Ankles In Diabetics
Is There A Diabetes Gene
Scientists have not identified one gene which causes type 1 diabetes. Instead, they’ve discovered mutations in a tribe of genes called the human leukocyte antigen complex. Specific combinations of these mutations seem to confer a higher risk of developing type 1 diabetes.
“These mutations are associated with changes in one’s immune system which stimulates an autoimmune destruction of the insulin-producing cells of the pancreas leading to type 1 diabetes,” Deena Adimoolam, MD, a specialist in endocrinology and preventative medicine in New Jersey tells Health.
Specifically, these genes, which are located on chromosome 6, help the immune system identify which compounds are natural to the body and which shouldn’t be there. Without this ability, the immune system has no way to tell which compounds are friends and which are foes.
This same gene complex is also involved in other autoimmune diseases, which may explain another feature of type 1 diabetes.
“Patients with type 1 diabetes can have other autoimmune diseases,” says Dr. Olansky. “They probably have a similar pathway.”
But the changes in HLA genes only explain about 40% of the genetic risk for type 1 diabetes. There are other genes that can not only increase the risk but also lower the risk. “There are a lot of other genes that modify that risk and make it greater or lesser,” says Dr. Olansky.
Is Type 1 Diabetes Hereditary
We are also unsure about whether type 1 diabetes is hereditary or not. While 90 per cent of people who develop type 1 diabetes have no relative with the condition, genetic factors can pre-dispose people to developing type 1 diabetes.
Certain gene markers are associated with type 1 diabetes risk. A child born with these will have the same risk of developing type 1 diabetes as a child with siblings with type 1 diabetes. However, having the marker alone is not enough to cause someone to develop type 1 diabetes it is thought that an additional trigger causes type 1 diabetes to develop.
Read Also: Signs And Symptoms Of Diabetes Mellitus
What Is The Difference Between Type 1 And Type 2 Diabetes
There are two main forms of diabetes, type 1 and type 2.
There also is gestational diabetes in pregnant women too, but we will not be focusing on that type today.
Type 1 diabetes is when your body doesnt produce enough insulin which helps to control the amount of sugar in your blood.
Type 2 diabetes is when your body doesnt produce enough insulin or when the insulin doesnt work properly.
Type 2 diabetes, which is the most common form, usually starts with insulin resistance, meaning your cells dont take in the proper amount of insulin.
When type 2 diabetes is allowed to progress, your body then may lack enough insulin to be healthy.
Type 2 diabetes is usually diagnosed in adults over the age of 40, but it is now being seen in younger people as well.
Diagnosis And Management Of Adult
Correctly identifying diabetes etiology and type is difficult, and misclassification may occur in up to 40% of adults presenting with type 1 diabetes . Reasons underlying misclassification are multiple and include 1) lack of awareness that the onset of type 1 diabetes is not limited to children 2) the overwhelming majority of people developing diabetes as older adults have type 2 diabetes, contributing to a confirmation bias 3) typical clinical criteria, such as BMI and metabolic syndrome, can be poor discriminators, especially as rates of obesity in the overall population increase 4) clinical characteristics of adult-onset type 1 diabetes can masquerade as type 2 diabetes, given their slow metabolic progression and risk of metabolic syndrome , so that the distinction between types of diabetes may be blurred and 5) lack of awareness of and accessibility to biomarkers that may serve as tools to distinguish type 1 diabetes and type 2 diabetes.
Don’t Miss: How To Lower Blood Sugar Quick
Family History Of Type 1 Diabetes
Although more than 85% of patients with T1D lack a positive family history for the disease, there is high familial clustering with a mean prevalence of 6% in siblings compared to 0.4% in the US white population. The familial clustering can be calculated as the ratio of the risk to siblings over the disease prevalence in the general population, and thus s = 6/0.4 = 15 .
The risk for T1D in siblings of patients is 15-fold higher than the risk for T1D in the general population, which suggests that genetic factors play an important role in disease susceptibility. The pattern of inheritance is complex, and the development of disease is thought to be determined by an interaction between genetic predisposition and environmental triggers. Concordance rates for T1D in monozygous twins with long-term follow-up is > 50%, compared to 6%10% in dizygous twins, which is similar to what is found in nontwin siblings. With long-term followup, at least two-thirds of initially discordant monozygous twins show evidence of persistent -cell autoantibodies and/or diabetes .
Development of islet autoimmunity and diabetes in monozygotic twins
Among first-degree relatives, siblings are at a higher risk than offspring offspring of diabetic fathers are at a higher risk than offspring of diabetic mothers . In addition, DR3/4 siblings who share both HLA haplotypes identical by descent with their diabetic DR3/4 sibling are at a higher risk than those sharing 1 or no haplotypes .
Expression Qtls Contribute To Tissue
We hypothesized that disease-relevant biological processes are fundamentally dependent on mRNA levels, with the cross-tissue variability of gene expression providing an important avenue for understanding disease etiologies. Therefore, we analyzed the tissue-specific contributions of T1D-associated eQTLs to tissues. Consistent with our hypothesis, eQTL effects were distributed differently across human tissues . Tibial artery and lower leg skin tissues have been linked to peripheral arterial disease in diabetic patients . Both tibial artery and lower leg skin were observed to have the highest proportion while brain substantia nigra tissue displayed the lowest proportion of eQTLs .
FIGURE 3. T1D-associated eQTL effects are tissue-specific. T1D-associated eQTLs are differentially distributed across human tissues. The differential distribution is epitomized by the relative proportions of HLA and non-HLA associated eQTLs in different tissues. A complete summary of all GTEx tissues with significant eQTLs is presented in Supplementary Figure 1. The relative contributions of HLA associated T1D eQTLs to tissue specific effects. Relative contribution was calculated . The mean HLA contribution was 28.16 ± 8.79%. eGenes within tissues with high or low HLA contributions were enriched for biological pathways associated with immune pathways. Biological pathway enrichment was performed using the Reactome pathways database , with significant for immune response pathways.
Read Also: What Are The Beginning Symptoms Of Diabetes