Insulin Secretion Function And Impairment
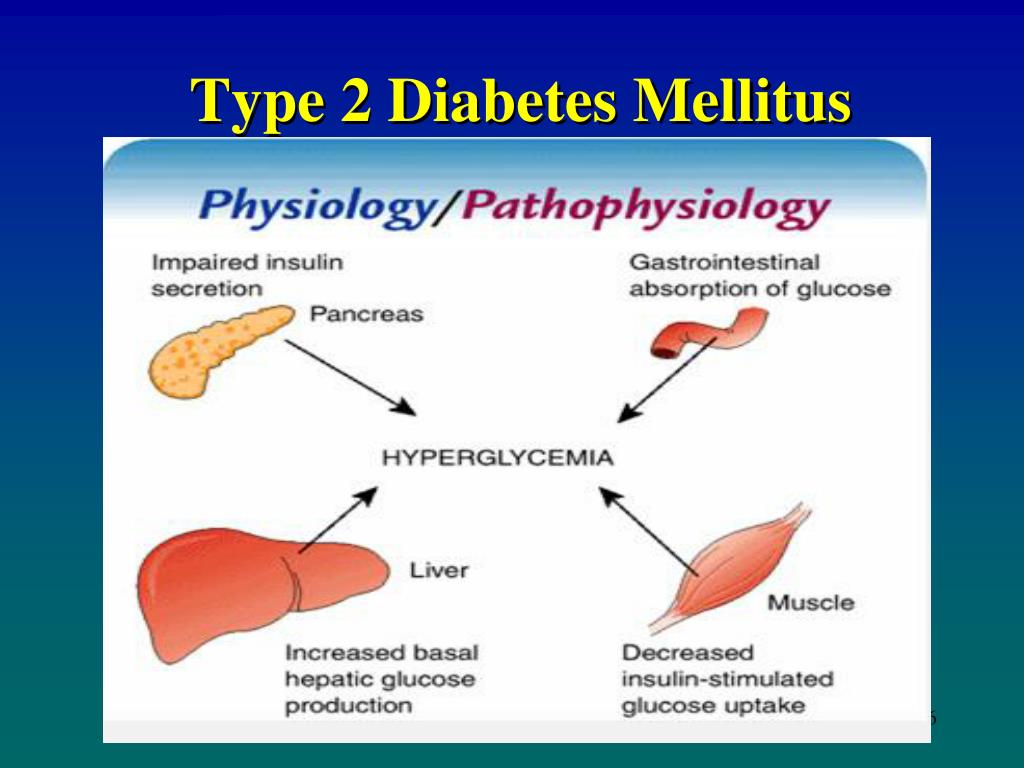
Insulin is synthesized and produced by – cells in the pancreas. It is a peptide hormone regulates the metabolism of fat and carbohydrate in the body. It helps glucose absorption from the circulation by fat tissue and skeletal muscles. Figures 1 and 2 .
Figure 1.
14 ].
Insulin is secreted from the secretory cells by priming reaction. Each cell contains thousands of secretory vesicles/granules. Less than < 5% of these cells exist to release the readily pool insulin by exocytosis followed by minimal latency of immediate releasable pool of insulin. The bulk of granules in the cell exist in a non-releasable reserve pool of insulin, which must undergo a series of ATP-, Ca2+-, and temperature-dependent reactions to release insulin .
The prevalence of Gestational diabetes is 2-3% of all pregnant women. GDM women have the same second phase insulin response as women with normal oral GTT. But, the first phase-insulin secretion is reduced with intravenous glucose and has a later peak rise with OGTT. Both groups showed a decreased in IS by 50-70%, this is back to normal in postpartum period in women with normal OGTT but this is not in women with GDM. In the same period, the latter group also demonstrated a persistent and excessive proinsulin secretion. Women with GDM have also a substantial increase in insulin secretion with OGTT or a meal compared to the same women in postpartum period. But this rise is less in women with GDM compared with pregnant women who retain normal OGTT .
Extrapancreatic Tissues Involvement In T2d: Aetiology/pathogenesis And Post
Whilst it is firmly established that pathological pancreatic function and peripheral tissue insulin resistance are central to T2D aetiology/pathogenesis, there is increasing evidence that other extrapancreatic pathologies may contribute.30,191,192 The diabetic phenotype includes systemic pathology, such as in the CVS, skeletal muscle, nervous system , skin, kidneys and gastrointestinal tract , which further exacerbates the disease phenotype and/or induces post-diagnosis complications.30, However, research evidence over the last few decades suggests that some of these pathologies manifest during the prediabetic phase and is possibly therefore involved in both the disease pathogenesis and aetiology.191,192 For example, skin and liver pathology can manifest during the prediabetic stage, and even in individuals with metabolic syndrome before islet beta-cell dysfunction occurs.191,196
|
Figure 7 A summary of the pathological effects that T2D has on different organs and systems throughout the body, some of which directly contribute to the disease-associated dyslipidaemia/hyperglycaemia and subsequent clinical symptoms. This figure and information in its legend are with data adapted from these studies.94,105,106,111,,206,214,,225,228,232,241,,331 |
Pearls And Other Issues
- T1DM is characterized by the autoimmune destruction of pancreatic beta cells in the majority.
- T2DM is caused due to duel defects in insulin resistance and insulin secretion.
- Gestational diabetes is associated with maternal as well as fetal complications.
- Exercise and a healthy diet are beneficial in both type 1 and type 2 diabetes mellitus.
You May Like: Do Type 2 Diabetics Take Insulin Shots
Is Banana Good For Diabetes
Bananas are a safe and nutritious fruit for people with diabetes to eat in moderation as part of a balanced, individualized diet plan. A person with diabetes should include fresh, plant food options in the diet, such as fruits and vegetables. Bananas provide plenty of nutrition without adding many calories.
Insulin Secretion And Metabolism
The homeostasis of glucose is maintained by a balance of hepatic glucose production and peripheral glucose uptake and utilization. Glucose is the key regulator of insulin secretion by the pancreatic beta cell. Other metabolic end products such as ketones, amino acids, enteric peptides and neurotransmitter also influence insulin release.
Insulin is secreted in a pulsatile pattern with small secretory bursts every 10 minutes superimposed upon greater amplitude oscillations of about 80-150 minutes. After a meal, bursts of insulin secretion usually last for two to three hours prior to returning to baseline levels.
Once insulin is released into the portal venous system, the liver degrades half of the secreted insulin. The remaining insulin enters the systemic circulation to reach the target binding sites. Activation of insulin receptors induces synthesis of glycogen, synthesis of proteins, lipogenesis and regulation of various genes in insulin-responsive cells.
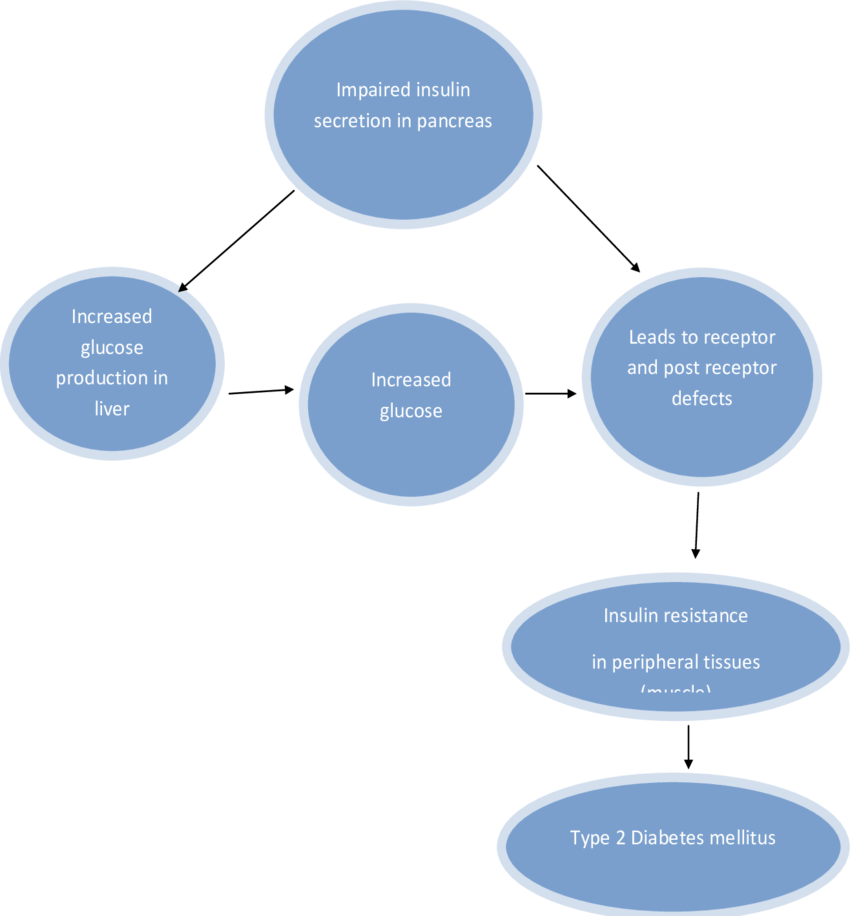
There are three pathophysiologic mechanisms, which are central to the development of Type II diabetes mellitus: impaired insulin secretion, peripheral insulin resistance, and excessive hepatic glucose production. In the early phase of this disease, despite the presence of insulin resistance, blood glucose may remain normal due to compensatory increase in insulin secretion by the remaining beta cells. Once this compensatory mechanism is exhausted, derangements in blood glucose concentrations become evident.
Read Also: Foods Good For Kidney Disease And Diabetes
What Is The Pathophysiology Of Dementia
Dementia is a symptom of a variety of specific structural brain diseases as well as several system degenerations. Alzheimers disease presently is the commonest cause in the developed world, causing a cortical-subcortical degeneration of ascending cholinergic neurons and large pyramidal cells in the cerebral cortex.
Factors That May Have Contributed To T2dm Development
Certain aspects of the patients life could have contributed to the development of the disease. His social history shows that he does not use illicit drugs or smokes, but drinks occasionally when out with friends. The consumption of beer and spirits has been associated with increased risk of abnormal glycemic profiles associated with pre-diabetes and T2DM . This study also found that low alcohol use reduced the T2DM risk in females. In this study, the risk of developing T2DM was higher in samples that consumed spirits than those with a moderate wine intake. Therefore, the patients occasional alcohol use could have predisposed him to T2DM.
Another risk factor relevant to this case is genetics. The patients father has a history of T2DM, an important factor in the pathogenesis of the disease. Family history accounts for the high T2DM incidence of up to 40% in first-degree relatives compared to non-first-degree relatives . The heritable genetic component relates to genes involved in glucose metabolism or homeostasis. Heritable mutations in the insulin receptor genes, such as the KCNQ1 gene, have been associated with impaired insulin secretion and resistance . The patient may have inherited genetic abnormalities that affected insulin function or secretion from his father, predisposing him to T2DM.
You May Like: Free Insulin For Type 1 Diabetes
What Is The Pathophysiology Of Type 2 Diabetes Mellitus
In a state of health, normoglycemia is maintained by fine hormonal regulation of peripheral glucose uptake and hepatic production. Type 2 diabetes mellitus results from a defect in insulin secretion and an impairment of insulin action in hepatic and peripheral tissues, especially muscle tissue and adipocytes. A postreceptor defect is also present, causing resistance to the stimulatory effect of insulin on glucose use. As a result, a relative insulin deficiency develops, unlike the absolute deficiency found in patients with type 1 diabetes. The specific etiologic factors are not known, but genetic input is much stronger in type 2 diabetes than in the type 1 form.
References
American Diabetes Association. Summary of Revisions: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020 Jan. 43 :S4-S6. .
World Health Organization. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. August 22, 2013. Available at .
World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: Report of a WHO/IDF consultation. January 14, 2006. Available at .
American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020 Jan. 43 :S14-S31. .
Increase Hepatic Glucose Production
In type II diabetes mellitus, insulin resistance in the liver reflects the failure of hyperinsulinemia to suppress gluconeogenesis. This results in fasting hyperglycemia and decreased glycogen storage by the liver in the post-prandial state. Increased hepatic glucose production occurs early in the disease course of diabetes, likely after the onset of insulin secretory abnormalities and insulin resistance in the skeletal muscle.
Hepatic glucose production is regulated by two rate-limiting enzymes namely, glucose 6-phosphatase catalytic subunit, encoded byG6PC and phosphoenolpyruvatecarboxykinase, encoded by PCK1 and PCK2. As the expression of these enzymes is suppressed by insulin, it has been widely held that patients with type II diabetes would have increased expression of G6PC and PCK, due to hepatic insulin resistance.
Read Also: Can We Cure Type 2 Diabetes
Adipokine Balance And Cvd Risk
Adipose tissue dysfunction as a result of T2DM can result in an imbalance between pro-inflammatory and anti-inflammatory adipokines, and is one of the mechanisms of T2DM complications. Several studies indicate that adipokines are related to IR, and can result in endothelial dysfunction, and pro-inflammatory and pro-atherogenic states .
Omentin is an adipokine secreted from white adipose tissue and is involved in glucose homeostasis . Omentin circulates in the blood , and is associated with reduced levels in T2DM patients . In vitro studies have shown that omentin enhances insulin-stimulated glucose uptake in human adipocytes by AKT signaling pathway activation . In humans, an inverse correlation between omentin levels and IR is seen, both at the protein and mRNA levels . Additional studies show that omentin has anti-inflammatory properties, diminishes cytokine expression , and is negatively associated with systemic inflammatory markers such as TNF and IL-6 .
Vaspin is an adipokine that inhibits proteases responsible for IR and protects against atherosclerosis and plaque development . It has been shown that T2DM patients have higher serum vaspin levels than healthy controls. Higher vaspin levels are associated with a 1.7-fold increased risk of CVD . High vaspin is also associated with increased severity of coronary artery disease .
Insulin Secretion: Physiological And Dysfunctional Mechanisms Leading To T2dm
4.1.1. -Cell Physiology
To safeguard proper -cell function, cellular integrity must be ensured and the mechanisms and pathways implicated in the physiology of -cell must be tightly regulated .
-cells are responsible for insulin production, which is synthesized as pre-proinsulin. In the maturation process, pre-proinsulin undergoes a conformational modification carried out with the help of several proteins in the endoplasmic reticulum to yield proinsulin . Afterwards, proinsulin is translocated from the ER to the Golgi apparatus , entering into immature secretory vesicles and being cleaved into C-peptide and insulin .
Additionally, Ca2+ signals can be amplified by the RY receptors and may play important roles in stimulus- insulin secretion coupling by virtue of their strategic locations within the cell and their ability to mediate Ca2+ induced Ca2+ release . RYR amplifies Ca2+ signals when the channel is sensitized by messenger molecules generated from the nutrient metabolism or ligand-binding and are involved in the amplification of insulin secretion .
4.1.2. Mechanisms Leading to -Cell Dysfunction
4.1.3. Pathological Conditions Perpetuating T2DM
Nutritional Factors
Physical Activity
Gut Dysbiosis
Metabolic Memory
Mitochondrial Dysfunction
Also Check: Type 2 Diabetes Occurs When
Circadian System As A Novel Therapeutic Target In T2dm
Growing evidence suggests that therapeutic strategies designed to enhance circadian clock function may be beneficial for the prevention and treatment of metabolic disorders such as T2DM. First, as outlined in the current review, cell-autonomous circadian clocks orchestrate the regulation of physiological functions required for maintenance of normal glucose homesosis . Correspondingly, phenotypical characteristics of many clock gene mutant mice recapitulate the pathophysiology commonly observed in patients with T2DM, such as insulin resistance, excessive hepatic glucose production, ectopic fat accumulation, impaired insulin secretion, and β-cell loss . Second, pathogenesis of obesity and T2DM per se is linked with impairments in circadian regulation both at the level of central and peripheral circadian oscillators . Thus development of obesity and T2DM in humans is evidenced by disrupted circadian physiology . Indeed, obese diabetic rodents are characterized by disrupted behavioral and metabolic circadian rhythms associated with suppression of CLOCK-BMAL1 transactivation and impaired function of circadian oscillators in peripheral tissue . Moreover, ectopic expression of CLOCK and BMAL1 in insulin-sensitive tissues has been shown to reverse insulin resistance in skeletal muscle and liver, reduce lipolysis in adipocytes, and improve glucose tolerance in mouse models of T2DM .
What Is The Main Cause Of Diabetes
What causes type 1 diabetes? Type 1 diabetes occurs when your immune system, the bodys system for fighting infection, attacks and destroys the insulin-producing beta cells of the pancreas. Scientists think type 1 diabetes is caused by genes and environmental factors, such as viruses, that might trigger the disease.
Don’t Miss: Best Type 2 Diabetes App
Classification Of Type 2 Diabetes Mellitus
The definition of type 2 diabetes mellitus, previously termed noninsulin-dependent diabetes mellitus, was recently modified by the American Diabetes Association. Several criteria may be used independently to establish the diagnosis: 1) a 75-g oral glucose tolerance test with a 2-h value of 200 mg/dL or more, 2) a random plasma glucose of 200 mg/dL or more with typical symptoms of diabetes, or 3) a fasting plasma glucose of 126 mg/dL or more on more than one occasion . Fasting glucose values are preferred for their convenience, reproducibility, and correlation with increased risk of microvascular complications.
The term impaired fasting glucose has been defined as fasting plasma glucose of 110 or more and 125 mg/dL or less . Impaired glucose tolerance is defined as a 2-h plasma glucose value of 140 or more and of less than 200 mg/dL during an oral glucose tolerance .
Individuals with impaired fasting glucose and IGT are considered to be at high risk for the development of diabetes and macrovascular disease . Although one third of these patients will eventually develop diabetes, dietary modification and exercise can lower the risk of progression from impaired glucose tolerance to type 2 diabetes and may also prevent the development of IGT in nondiabetic individuals at high risk . Pharmacological agents may also be of benefit in limiting the progression from IGT to diabetes .
Is Egg Good For Diabetes
Eggs are a versatile food and a great source of protein. The American Diabetes Association considers eggs an excellent choice for people with diabetes. Thats primarily because one large egg contains about half a gram of carbohydrates, so its thought that they arent going to raise your blood sugar.
Read Also: How Much Sugar A Day To Get Diabetes
Circadian Organization Molecular Structure And Entrainment
The majority of organisms have evolved optimal physiological functionality under environmental conditions created by daily changes in the light-dark cycle. The driving force behind biological adaptation to changes in LD cycle is precipitated by the evolutionary development of the circadian system. The primary utility of the circadian system is to promote adaptation and organismal fitness in response to 24-h environmental cycles . A key aspect of circadian physiology is its intrinsic nature, suggesting the presence of an internal cell-specific temporal program that anticipates and regulates behavioral, physiological, genetic, and metabolic cycles appropriate for the outside environment . Thus evolutionary origins of the circadian system appear to be selected to promote organismal adaptation to diurnal changes in oxidative environment, UV-mediated DNA damage, as well as optimal diurnal regulation of cellular energetics and metabolism . Indeed, a functional circadian system has been shown to provide a clear fitness advantage to organisms from diverse living phyla such as plants , bacteria , yeast , and mammals .
What Does Metformin Do Exactly
Metformin lowers your blood sugar levels by improving the way your body handles insulin. Its usually prescribed for diabetes when diet and exercise alone have not been enough to control your blood sugar levels. For women with PCOS, metformin lowers insulin and blood sugar levels, and can also stimulate ovulation.
Also Check: List Of Insulins For Diabetes
What Is Type 2 Diabetes
Type 2 diabetes is a lifelong disease that keeps your body from using insulin the way it should. People with type 2 diabetes are said to have insulin resistance.
People who are middle-aged or older are most likely to get this kind of diabetes. It used to be called adult-onset diabetes. But type 2 diabetes also affects kids and teens, mainly because of childhood obesity.
Type 2 is the most common type of diabetes. There are about 29 million people in the U.S. with type 2. Another 84 million have prediabetes, meaning their blood sugar is high but not high enough to be diabetes yet.
Insulin Resistance In Adipose Tissue
Resistance to the antilipolytic action of insulin
Lipolysis in adipose tissue is exquisitely insulin sensitive: in normal subjects, rates of glycerol production are half-maximally suppressed at a plasma insulin concentration just exceeding fasting concentrations. Triglyceride breakdown is increased and plasma NEFA concentrations are higher in patients with type 2 diabetes than in normal subjects studied at comparable insulin levels, suggesting that adipose tissue is also affected by insulin resistance . However, unrestrained lipolysis to a degree that could lead to ketoacidosis does not occur spontaneously in type 2 diabetes, because insulin deficiency is not sufficiently profound.
Increased NEFA concentrations may contribute to worsening of hyperglycaemia because of multiple interactions between NEFA and glucose metabolism. Increased concentration of NEFA reflects increased NEFA turnover, which increases delivery to the liver, where NEFA can be deposited as triglycerides . In the liver, NEFA also stimulate glucose production, especially via gluconeogenesis. A large increase in plasma NEFA concentrations can decrease insulin-stimulated glucose uptake and NEFA may be deposited as triglycerides in skeletal muscle .
Adiponectin deficiency
You May Like: Diabetes Injection Pen For Weight Loss
Prognosis In Intensive Therapy
In the UKPDS, more than 5000 patients with type 2 diabetes were followed up for up to 15 years. Those in the intensely treated group had a significantly lower rate of progression of microvascular complications than did patients receiving standard care. Rates of macrovascular disease were not altered except in the metformin-monotherapy arm in obese individuals, in which the risk of myocardial infarction was significantly decreased.
In the 10-year follow-up to the UKPDS, patients in the previously intensively treated group demonstrated a continued reduction in microvascular and all-cause mortality, as well as in cardiovascular events, despite early loss of differences in glycated hemoglobin levels between the intensive-therapy and conventional-therapy groups. The total follow-up was 20 years, half while in the study and half after the study ended.
Other, shorter studies, such as Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation and the Veterans Affairs Diabetes Trial , showed no improvement in cardiovascular disease and death with tight control .
A British study indicated that the HbA1c level achieved 3 months after the initial diagnosis of type 2 diabetes mellitus predicts subsequent mortality. In other words, according to the report, aggressive lowering of glucose after diagnosis bodes well for long-term survival.