Disposal Of Used Insulin Syringes
Used syringes, pen needles, cannulas and lancets must be disposed of in an Australian Standards-approved sharps container, which is puncture-proof and has a secure lid. These containers are usually yellow and are available through pharmacies, local municipal councils and state or territory diabetes organisations such as Diabetes Victoria.
Procedures to dispose of sharps containers vary from state to state.
For sharps disposal information and help, you can contact:
- state or territory diabetes organisations, such as Diabetes Victoria
- state Department of Health
Insulin needs to be stored correctly. This includes:
- Store unopened insulin on its side in a fridge.
- Keep the fridge temperature between 2 and 8 °C.
- Make sure that insulin does not freeze.
- Once opened, keep it at room temperature for not more than one month and then dispose of it safely.
- Avoid keeping insulin in direct sunlight.
Extreme temperatures can damage insulin so it doesn’t work properly. It must not be left where temperatures are over 30 °C. In summer your car can get this hot so don’t leave your insulin there.
There are various insulated insulin carry bags available for transporting insulin.
Pharmacologic Approaches To Glycemic Treatment: Standards Of Medical Care In Diabetes2018
American Diabetes Association 8. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes2018. Diabetes Care 1 January 2018 41 : S73S85.
The American Diabetes Association Standards of Medical Care in Diabetes includes ADAs current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADAs clinical practice recommendations, please refer to the Standards of Care Introduction. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC.
Pancreas And Islet Cell Transplantation
Pancreas and islet cell transplantation have been shown to normalize glucose levels but require lifelong immunosuppression to prevent graft rejection and recurrence of autoimmune islet destruction. Given the potential adverse effects of immunosuppressive therapy, pancreas transplantation should be reserved for patients with type 1 diabetes undergoing simultaneous renal transplantation, following renal transplantation, or for those with recurrent ketoacidosis or severe hypoglycemia despite aggressive glycemic management . Islet cell transplantation remains investigational. Autoislet transplantation may be considered for patients requiring total pancreatectomy who meet eligibility criteria.
Recommended Reading: How Can An Ophthalmologist Help A Diabetic
Pharmacological Therapy For Type 1 Diabetes
Recommendations
-
Most people with type 1 diabetes should be treated with multiple-dose insulin injections or continuous subcutaneous insulin infusion. A
-
Consider educating individuals with type 1 diabetes on matching prandial insulin dose to carbohydrate intake, premeal blood glucose, and anticipated activity. E
-
Most individuals with type 1 diabetes should use insulin analogs to reduce hypoglycemia risk. A
-
Individuals who have been successfully using continuous subcutaneous insulin infusion should have continued access after they turn 65 years of age. E
Perioperative Blood Glucose Management
Surgical proceduresincluding the preoperative emotional stress and the effects of general anesthesia as well as the trauma of the procedure itselfcan markedly increase plasma glucose levels and induce DKA in patients with type 1 DM. In patients going to surgery who have not received a dose of intermediate-acting insulin that day, injection of one third to one half of the total daily dose as NPH insulin or 80% of the dose as glargine or detemir insulin before surgery is often effective.
At the same time, an IV infusion containing 5% glucose in either 0.9% saline solution or water should be started at a rate of 1 L over 6-8 hours . Blood glucose levels should be checked every 2 hours during the surgical procedure, and small doses of regular or rapid-acting insulin should be given if values exceed 140 mg/dL.
After the operation, check plasma glucose levels and assess for a reaction to ketones. Unless a change in dosage is indicated, repeat the preoperative dose of insulin when the patient recovers from the anesthesia, and continue the glucose infusion.
Monitor plasma glucose and ketones at 2- to 4-hour intervals, and administer regular insulin every 4-6 hours as needed to maintain the plasma glucose level in the range of 100-250 mg/dL . Continue until the patient can be switched to oral feedings and a 2- or 3-dose insulin schedule.
Postoperative IV insulin infusion after major surgical procedures is currently considered the standard of care in most hospitals.
Don’t Miss: How Does Diabetes Lead To Renal Failure
How Much Insulin Do You Need
In type 1 diabetes, most people need a total of 0.5 – 0.8 units of insulin per kilogram of body weight each day. Roughly half this insulin is needed for food intake, and half is the basal rate. In DAFNE half is therefore taken as long-acting insulin and this is divided into two injections of Levemir insulin. One injection when you get up in the morning, and the other in the evening at bedtime. For most people, this is about 24 units in 24 hours.
The amount of background insulin does not depend on what you eat, and the dose should be low enough to allow you to miss meals without the risk of low glucose , whilst still keeping the glucose levels within the target range.
The remainder of the total daily dose is taken at meal times, as a quick acting insulin. Sometimes these are given as insulin mixtures, but not in the DAFNE program.
Insulin Dosing In Type 1 Diabetes
Aka: Insulin Dosing in Type 1 Diabetes, Insulin Dosing in Type I Diabetes
II. Dose: Initial Dosing with basal/Bolus Insulin
III. Dose: Conversion from mixed Insulin
IV. Management: Adjustments
Also Check: How Much Does It Cost To Make Insulin
Total Daily Insulin Requirement:
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
Slowing Progress Of Recent
In animal models of autoimmunity, treatment with a target antigen can modulate aggressive autoimmunity. However, a trial of antigen-based immunotherapy with 2 or 3 doses of glutamic acid decarboxylase formulated with aluminum hydroxide vaccine for 4-12 weeks in patients with newly diagnosed type 1 DM did not alter the course of loss of insulin secretion during the first year.
A phase 3 trial using an anti-CD3 monoclonal antibody, teplizumab, found an encouraging trend toward preservation of beta-cell function with reduction in daily insulin requirements in patients with recently diagnosed type 1 DM. However, rash was almost 3 times more common in treated patients than in those receiving placebo.
A study by Orban et al found that costimulation modulation of activated T cells with abatacept slowed reduction in beta-cell function over a 2-year period of administration. However, this effect was reduced after 6 months of treatment, suggesting that T-cell activation lessens over time. Further studies are needed.
Read Also: Best Bread For Diabetics To Eat
Example #: Formulas Commonly Used To Create Insulin Dose Recommendations
This example illustrates a method for calculating of your background/basal and bolus doses and estimated daily insulin dose when you need full insulin replacement. Bear in mind, this may be too much insulin if you are newly diagnosed or still making a lot of insulin on your own. And it may be too little if you are very resistant to the action of insulin. Talk to your provider about the best insulin dose for you as this is a general formula and may not meet your individual needs.
The initial calculation of the basal/background and bolus doses requires estimating your total daily insulin dose:
Pharmacologic Therapy For Type 2 Diabetes
Recommendations
See Section 12 for recommendations specific for children and adolescents with type 2 diabetes. The use of metformin as first-line therapy was supported by findings from a large meta-analysis, with selection of second-line therapies based on patient-specific considerations . An ADA/European Association for the Study of Diabetes position statement Management of Hyperglycemia in Type 2 Diabetes, 2015: A Patient-Centered Approach recommended a patient-centered approach, including assessment of efficacy, hypoglycemia risk, impact on weight, side effects, costs, and patient preferences. Renal effects may also be considered when selecting glucose-lowering medications for individual patients. Lifestyle modifications that improve health should be emphasized along with any pharmacologic therapy.
Also Check: Surgical Treatment For Type 2 Diabetes
Example #: Carbohydrate Coverage At A Meal
First, you have to calculate the carbohydrate coverage insulin dose using this formula:
CHO insulin dose = Total grams of CHO in the meal ÷ grams of CHO disposed by 1 unit of insulin .
For Example #1, assume:
- You are going to eat 60 grams of carbohydrate for lunch
- Your Insulin: CHO ratio is 1:10
To get the CHO insulin dose, plug the numbers into the formula:
CHO insulin dose =
- The carbohydrate coverage dose is 6 units of rapid acting insulin.
- The high blood sugar correction dose is 2 units of rapid acting insulin.
Now, add the two doses together to calculate your total meal dose.
Carbohydrate coverage dose + high sugar correction dose = 8 units total meal dose!
The total lunch insulin dose is 8 units of rapid acting insulin.
Glycemic Control During Serious Medical Illness And Surgery
Serious medical illness and surgery produce a state of increased insulin resistance and relative insulin deficiency. Hyperglycemia can occur even in patients without diabetes as a consequence of stress-induced insulin resistance coupled with the use of dextrose-containing IV fluids. Increases in glucagon, catecholamines, cortisol, and growth hormone levels antagonize the effects of insulin, and the alpha-adrenergic effect of increased catecholamine levels inhibits insulin secretion. Counterregulatory hormones also directly increase hepatic gluconeogenesis.
Much less is known about optimal blood glucose levels in hospitalized patients with preexisting diabetes whose hyperglycemia reflects both their diabetes and a stress response to illness. Nonetheless, it is clear that management of hospitalized patients with preexisting diabetes requires modification of treatment regimens to compensate for both the decreased caloric intake and the increased physiologic stress. Near-normal blood glucose levels should be maintained in medical and surgical patients with diabetes, for the following reasons:
-
To prevent the development of ketosis
-
To prevent electrolyte abnormalities and volume depletion secondary to osmotic diuresis
-
To prevent the impairment of leukocyte function that occurs when blood glucose levels are elevated
-
To prevent the impairment of wound healing that occurs when glucose levels are elevated
Read Also: Best Type 1 Diabetes Snacks
Factors That Speed Insulin Absorption
Variation in insulin absorption can cause changes in blood glucose levels. Insulin absorption is increased by:
- injecting into an exercised area such as the thighs or arms
- high temperatures due to a hot shower, bath, hot water bottle, spa or sauna
- massaging the area around the injection site
- injecting into muscle this causes the insulin to be absorbed more quickly and could cause blood glucose levels to drop too low.
Glycemic Control During Pregnancy
Because pregnant patients with type 1 DM are at risk for multiple poor maternal and fetal outcomes, it is essential to provide these patients with prepregnancy counseling, good glycemic control before and during pregnancy, and a complete medical evaluation. High-risk possibilities include exacerbation of existing hypertension, renal insufficiency, retinopathy, and more frequent congenital anomalies. These patients should be referred to obstetricians specializing in high-risk pregnancies.
Despite advanced age, multiparity, obesity, and social disadvantage, patients with type 2 DM were found to have better glycemic control, fewer large-for-gestational-age infants, fewer preterm deliveries, and fewer neonatal care admissions than patients with type 1 DM. This finding suggests that better tools are needed to improve glycemic control in patients with type 1 DM.
Read Also: Best Diet For Type One Diabetes
Pharmacological Therapy For Type 2 Diabetes
Recommendations
-
Metformin, if not contraindicated and if tolerated, is the preferred initial pharmacological agent for type 2 diabetes. A
-
Consider initiating insulin therapy in patients with newly diagnosed type 2 diabetes and markedly symptomatic and/or elevated blood glucose levels or A1C. E
-
If noninsulin monotherapy at maximum tolerated dose does not achieve or maintain the A1C target over 3 months, then add a second oral agent, a glucagon-like peptide 1 receptor agonist, or basal insulin. A
-
A patient-centered approach should be used to guide the choice of pharmacological agents. Considerations include efficacy, cost, potential side effects, weight, comorbidities, hypoglycemia risk, and patient preferences. E
-
For patients with type 2 diabetes who are not achieving glycemic goals, insulin therapy should not be delayed. B
An American Diabetes Association/European Association for the Study of Diabetes position statement evaluated the data and developed recommendations, including advantages and disadvantages, for antihyperglycemic agents for patients with type 2 diabetes. A patient-centered approach is stressed, including patient preferences, cost, and potential side effects of each class, effects on body weight, and hypoglycemia risk. Lifestyle modifications that improve health should be emphasized along with any pharmacological therapy.
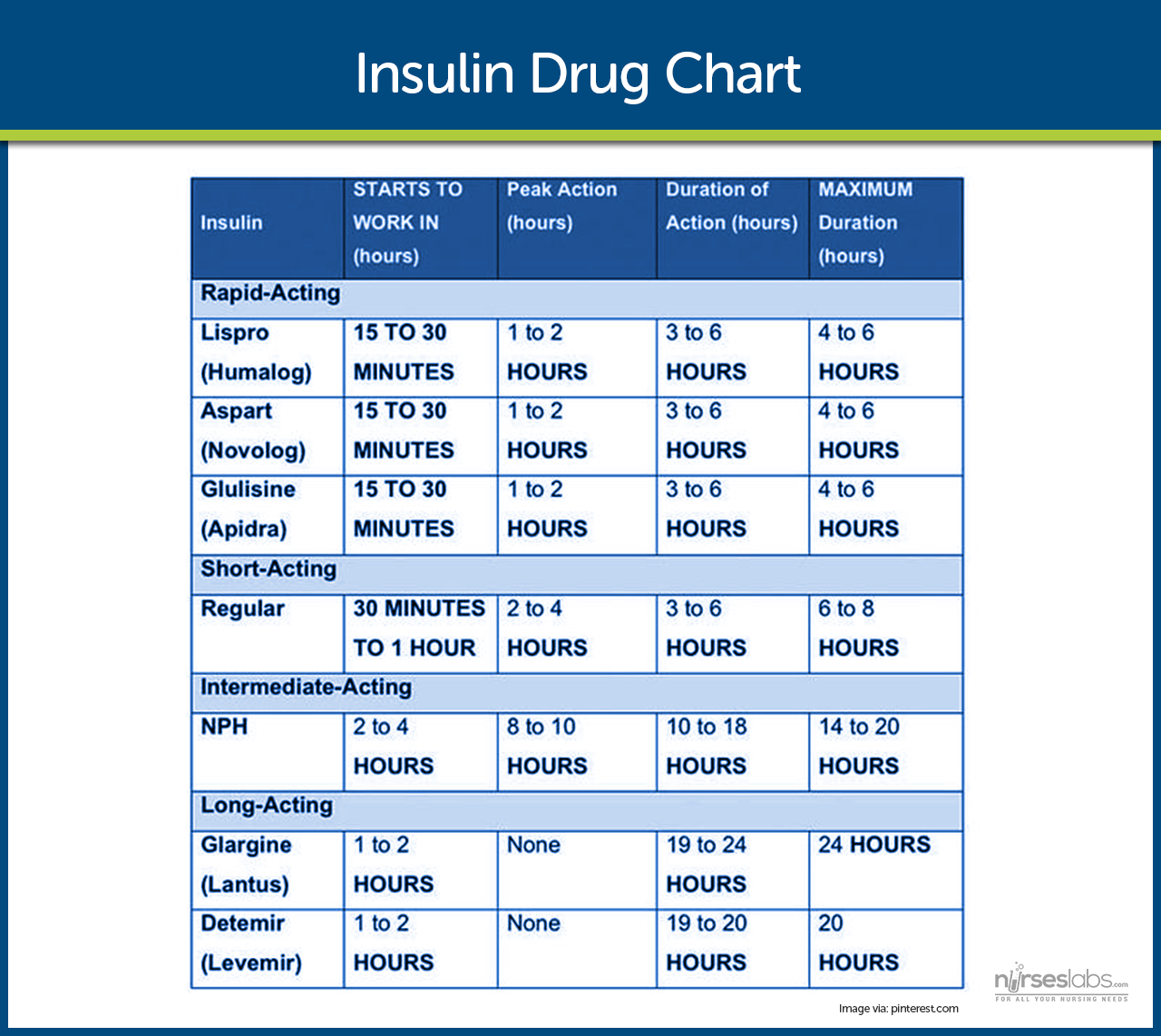
Types Of Insulin Where To Inject It And The Best Methods For Insulin Delivery
role of insulinshort- and long-term complicationsYour diabetes treatment team is there to help you. Patients’ Guide to Managing Your Child’s Type 1 Diabetes
This article will provide a basic overview of insulin. You can also visit our Patients’ Guide to Insulin for more information as well as read more in the section on Type 1 Diabetes Treatments, which has a chart providing more detail about the types of insulin that your doctor may prescribe.
You May Like: Type 1 Diabetes Blurred Vision
Dawn And Somogyi Phenomena
The dawn phenomenon is the normal tendency of the blood glucose to rise in the early morning before breakfast. This rise, which may result from the nocturnal spikes in growth hormone that cause insulin resistance, is probably enhanced by increased hepatic gluconeogenesis secondary to the diurnal rise in serum cortisol.
In some patients, however, nocturnal hypoglycemia may be followed by a marked increase in fasting plasma glucose with an increase in plasma ketones . Thus, both the dawn phenomenon and the Somogyi phenomenon are characterized by morning hyperglycemia, but the latter is considered to be rebound hyperglycemia.
The existence of a true Somogyi phenomenon is a matter of debate. Most endocrinologists now believe this phenomenon reflects waning of insulin action with consequent hyperglycemia.
In cases of the dawn phenomenon, the patient should check blood glucose levels at 2:00-4:00 AM. The dawn and Somogyi phenomena can be ameliorated by administering intermediate insulin at bedtime.
First Some Basic Things To Know About Insulin:
- Approximately 40-50% of the total daily insulin dose is to replace insulin overnight, when you are fasting and between meals. This is called background or basal insulin replacement. The basal or background insulin dose usually is constant from day to day.
- The other 50-60% of the total daily insulin dose is for carbohydrate coverage and high blood sugar correction. This is called the bolus insulin replacement.
Bolus Carbohydrate coverage
The bolus dose for food coverage is prescribed as an insulin to carbohydrate ratio.The insulin to carbohydrate ratio represents how many grams of carbohydrate are covered or disposed of by 1 unit of insulin.
Generally, one unit of rapid-acting insulin will dispose of 12-15 grams of carbohydrate. This range can vary from 6-30 grams or more of carbohydrate depending on an individuals sensitivity to insulin. Insulin sensitivity can vary according to the time of day, from person to person, and is affected by physical activity and stress.
Bolus High blood sugar correction
The bolus dose for high blood sugar correction is defined as how much one unit of rapid-acting insulin will drop the blood sugar.
Generally, to correct a high blood sugar, one unit of insulin is needed to drop the blood glucose by 50 mg/dl. This drop in blood sugar can range from 30-100 mg/dl or more, depending on individual insulin sensitivities, and other circumstances.
You May Like: Diabetes And Lower Back Pain
You’ll Need To Calculate Some Of Your Insulin Doses
You’ll also need to know some basic things about insulin. For example, 40-50% of the total daily insulin dose is to replace insulin overnight.
Your provider will prescribe an insulin dose regimen for you however, you still need to calculate some of your insulin doses. Your insulin dose regimen provides formulas that allow you to calculate how much bolus insulin to take at meals and snacks, or to correct high blood sugars.
Initiation Of Insulin Therapy
The initial daily insulin dose is calculated on the basis of the patients weight. This dose is usually divided so that one half is administered before breakfast, one fourth before dinner, and one fourth at bedtime. After selecting the initial dose, adjust the amounts, types, and timing according to the plasma glucose levels. Adjust the dose to maintain preprandial plasma glucose at 80-150 mg/dL .
The insulin dose is often adjusted in increments of 10% at a time, and the effects are assessed over about 3 days before any further changes are made. More frequent adjustments of regular insulin can be made if a risk of hypoglycemia is present.
Carbohydrate counting may be used to determine the meal-time insulin dose. Because patients may experience hyperglycemic episodes despite strict adherence to carbohydrate counting, particularly after meals that are high in protein or fat, Australian researchers developed an algorithm for estimating the mealtime insulin dose on the basis of measurements of physiologic insulin demand evoked by foods in healthy adults. The researchers showed that use of this algorithm improved glycemic control.
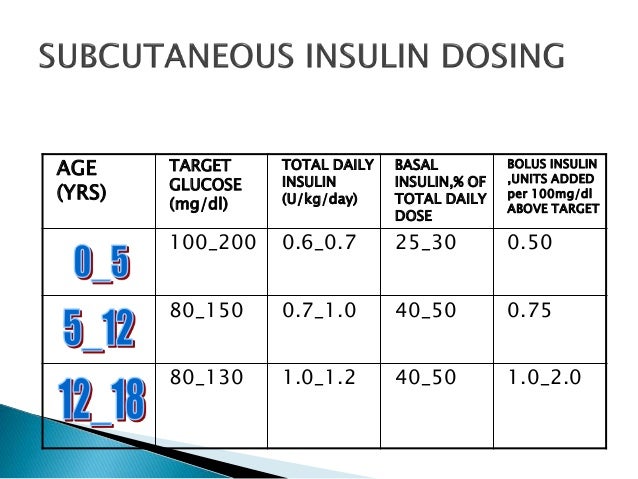
Initiation of insulin therapy in children
Multiple daily injections
Continuous subcutaneous insulin infusion
Changes in altitude may affect delivery from insulin pumps. During the flight of a commercial airliner , excess insulin delivery of 0.623% of cartridge volume was demonstrated as a result of bubble formation and expansion of preexisting bubbles.
You May Like: What Are The Beginning Symptoms Of Diabetes