Risks And Side Effects
Possible risks and side effects of anti-VEGF injections include:
- eye irritation or discomfort
- floaters or a feeling of having something in your eye
- watery or dry, itchy eyes
There’s also a risk that the injections could cause blood clots to form, which could lead to a heart attack or stroke.
This risk is small, but it should be discussed with you before you give your consent to treatment.
The main risk with steroid injections is increased pressure inside the eye.
Evidence Of Recovery Before Protocol Change
Although the principal goal of photocoagulation treatment is to prevent visual loss, not to improve vision, there were eyes with some evidence of recovery, defined as VA â¥5/200 at any subsequent visit at 1, 2 or 3 consecutively completed follow-up visits. The percentage of eyes with some evidence of recovery at each visit were 28.6%, 12.2% and 7.7% in untreated eyes compared with 48.8%, 28.6% and 20.8% in treated eyes, respectively. Therefore, it appeared that recovery of VA was more frequent in treated than untreated eyes.
Stage : Mild Nonproliferative Diabetic Retinopathy
In this early stage of diabetic retinopathy, also known as background retinopathy, there are not yet any symptoms. But when an eye doctor examines you, some tiny microaneurysms may be present. What an eye specialist may notice are extremely small bulges in blood vessels that may leak ever so slightly.
You May Like: How To Wear An Insulin Pump
Scenario : Pdr With Single Nve
Janssin et al in their retrospective series found that 40% of the eyes with PDR had a single NVE. It is important to access the extent of non-perfusion in these eyes. A wider extent of non-perfusion would warrant closer follow-up. Presence of NVE is an indication of PRP. However, in a select group of patients with no tractional element and those who have demonstrated good compliance with regular follow-up, intravitreal anti-VEGFs can be tried. Although, intravitreal anti-VEGFs have shown to improve severity of diabetic retinopathy over time, studies based on FFA and OCTA analysis have shown no significant change in macular ischaemia on follow-up.61 PRP on the other hand has been noted to have significant improvement in vessel density of superficial and deep capillary plexuses for fovea and para foveal retina and constriction of FAZ on OCTA.32 PDR with single NVE is presented in Figure 1A.
Treatment Of Diabetic Retinopathy
-
Control of blood glucose and blood pressure
-
For macular edema, intraocular injection of antivascular endothelial growth factor drugs, intraocular corticosteroid implants, focal laser, and/or vitrectomy
-
For high-risk or complicated proliferative retinopathy, anti-VEGF drugs, panretinal laser photocoagulation and sometimes vitrectomy
-
Recalcitrant diabetic macular edema
Don’t Miss: Is Red Cabbage Good For Diabetics
Stage : Proliferative Diabetic Retinopathy
These patients had NPDR that has progressed to PDR, and they exhibit either neovascularization of the disc/elsewhere or vitreous/preretinal hemorrhage.2,5-7
These patients require immediate referral to a retina specialist for further testing and treatment. Peripheral neovascularization is usually treated with laser panretinal photocoagulation .7 They also often receive anti-VEGF intravitreal injections that may be performed in conjunction with PRP.7
Figure 4. This patient with type 2 diabetes was treated with laser PRP in the periphery for PDR in both eyes.
Until their disease stabilizes, these patients need to be monitored monthly by a retina specialist.7 Thereafter, they may be seen every 6 to 12 months.7
Communicate all findings to the patients PCP and/or endocrinologist. A phone call is warranted if the patient has new-onset PDR.
How Often Should You Have Your Eyes Examined
- If you have just been diagnosed with diabetes you should have your eyes examined promptly.
- If you have diabetes you should have your eyes examined regularly.
- If you are pregnant and have diabetes it is important to be seen by an ophthalmologist during your first trimester because pregnancy can accelerate the progression of diabetic retinopathy.
You May Like: How To Check If I Have Diabetes
Non Proliferative Diabetic Retinopathy Treatment
The goal of any treatment is to slow or stop the progression of the disease. In the early stages of non-proliferative diabetic retinopathy, regular monitoring may be the only treatment. Diet and exercise and controlling blood sugar levels can help control the progression of the disease.
Laser : If the disease advances, the blood vessels can leak blood and fluid into the retina, leading to macular edema. Laser treatment can stop this leakage. Focal laser photocoagulation involves using a laser to target a specific leaky vessel in the macula to keep macular edema from worsening.
What Causes Diabetic Retinopathy
Damaged blood vessels can cause vision loss when fragile, abnormal blood vessels grow and leak blood into the center of the eye. This advanced stage is called proliferative retinopathy. Also, fluid can leak into the center of the macula of the eye, where sharp, straight-ahead vision occurs. The macula swells and vision becomes blurry.
You May Like: Does Low Blood Sugar Cause High Blood Pressure
Stages Of Non Proliferative Diabetic Retinopathy
Mild non proliferative diabetic retinopathy swelling in small areas of the blood vessels in the retina.
Moderate non proliferative diabetic retinopathy some of the blood vessels in the retina will become blocked leading to hemorrhages
Severe non proliferative diabetic retinopathy more blocked blood vessels, which lead to areas of the retina no longer receiving adequate blood flow
Systemic Approach To Treat Diabetic Retinopathy
The best treatment for diabetic retinopathy is prevention. Keeping blood sugar levels and blood pressure under control can slow the development or progression of the disease. In most cases, additional ocular treatment is necessary when more advanced complications present, such as macular edema or new blood vessel growth.
Award-winning retinal specialists provide a systemic approach to treating diabetic retinopathy using the newest diagnostic and therapeutic strategies.
You May Like: Does One High A1c Mean Diabetes
Stage : Severe Nonproliferative Diabetic Retinopathy
At this stage, your eye has hemorrhages within the retina in all four quadrants, as even more blood vessels become blocked. With not enough blood going to the retina, the body in turn may signal for the growth of new blood vessels.
Unfortunately, there is a high likelihood that you will develop the progressive stage of diabetic retinopathy within one year.
Join Forces To Deliver Proper Care

As the number of US patients with diabetes grows, it is important for optometrists to collaborate with PCPs, endocrinologists, and retina specialists on managing these patients disease. This teamwork, combined with effective communication among caregivers and with patients, will enhance the care that they receive.
- 1. Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984 102:520-526.
- 2. American Optometric Association. Evidence-based Clinical Practice Guideline: Eye Care of the Patient With Diabetes Mellitus. www.aoa.org/optometrists/tools-and-resources/evidence-based-optometry/evidence-based-clinical-practice-guidlines/cpg-3–eye-care-of-the-patient-with-diabetes-mellitus. Accessed May 2, 2019.
- 3. Stratton IM, Kohner EM, Aldington SJ, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001 44:156-163.
You May Like: How To Keep Your Blood Sugar Stable
Laser Treatment For Proliferative Diabetic Retinopathy
The abnormal new blood vessels of proliferative diabetic retinopathy are treated with panretinal laser photocoagulation or PRP. During this procedure, the peripheral retina, which is not receiving adequate blood flow, is treated, in order to stop the development of abnormal blood vessels.
This treatment requires many laser applications, and thus may be divided into two or more separate sessions. Treatment stops the formation of new abnormal blood vessels and in most cases causes existing ones to shrink. PRP does not improve vision, but it can prevent the blinding complications of diabetic retinopathy in the majority of cases. Side effects include some loss of peripheral and color vision and a decrease in night vision. Some patients experience blurry vision, which can be temporary or continue indefinitely. Regardless of these side effects, PRP has been shown to decrease the risk of vision loss.
How Is Nonproliferative Diabetic Retinopathy Treated
Not all forms of nonproliferative diabetic retinopathy require treatment to the eyes, but all patients require continued care and blood sugar control through their primary care provider. If the diabetic damage includes a significant degree of swelling in the central portion of the retina, a condition called diabetic macular edema, medical therapy with injections of drugs in the eye or laser therapy may be recommended for the eyes involved. Injections of medications have become the most common modern treatment for diabetic macular edema and have the greatest chance for arresting the progression of the diabetic damage and in some cases restoring some lost vision. Laser photocoagulation is also a common treatment for nonproliferative diabetic retinopathy with macular edema. In this kind of procedure, painless brief spots of bright light are used to treat the retina to reduce further loss of vision from diabetic macular edema. Laser surgery may need to be repeated several times. If the diabetic retinopathy progresses beyond the nonproliferative stage to the proliferative stage, a different type of laser therapy may be recommended.
In 2020, we joined together with other elite retina-only practices and formed Retina Consultants of America, now the premier national retina provider in the USA.
Don’t Miss: How To Raise Glucose Levels
What Are The Symptoms Of Diabetes
In the early stages, most people experience no signs of diabetes-related retinopathy. You may not experience vision changes until the condition is severe. For some people, symptoms come and go.
Symptoms of diabetes-related retinopathy include:
- Blurred or distorted vision.
- Poor night vision .
- Small dark spots or streaks in your vision.
- Trouble reading or seeing faraway objects.
Treatments For Advanced Diabetic Retinopathy
For diabetic retinopathy that is threatening or affecting your sight, the main treatments are:
- laser treatment to treat the growth of new blood vessels at the back of the eye in cases of proliferative diabetic retinopathy, and to stabilise some cases of maculopathy
- eye injections to treat severe maculopathy that’s threatening your sight
- eye surgery to remove blood or scar tissue from the eye if laser treatment is not possible because retinopathy is too advanced
You May Like: What To Give Diabetic With Low Blood Sugar
Is Diabetic Retinopathy Treatment Right For Me
At Vitreous Retina Macula Consultants of New York, one of our ophthalmologists and retina specialists will meet with you during your consultation to assess your situation. We will explain each treatment options pros and cons and suggest which diabetic retinopathy treatment in New York is right for you. VRMNY specializes in treating all medical and surgical retinal conditions, emphasizing diabetic retinopathy, the leading cause of retinal vision loss. Request an appointment online or call the internationally-renowned retina specialists and best-rated Diabetic Retinopathy Doctors at 861-9797 to schedule your private consultation.
Treatment For Diabetic Retinopathy
Laser surgery is the most common form of treatment for diabetic retinopathy. The laser seals the blood vessels and stops their growth. This diabetic retinopathy treatment method improves vision and prevents further vision loss by helping reduce swelling of the retina and inhibiting new blood vessel formation in the retina. Laser surgery is a painless in-office procedure that can be done in less than 30 minutes.
Laser surgery is not effective once the vitreous is clouded with blood. For these cases, a vitrectomy is performed. A vitrectomy is a treatment option for diabetic retinopathy and involves surgically removing the clouded vitreous and replacing it with a clear artificial solution such as saline . Ongoing diabetic retinopathy treatment includes regular checkups, controlling your blood sugar, medication and blood pressure management, and a healthy, balanced diet.
Also Check: Is Type 2 Diabetes Reversible With Diet And Exercise
Literature Searches And Study Selection
The search question posed in the commissioning brief was:
What is the clinical and cost-effectiveness of pan-retinal laser treatment in the management of non-proliferative diabetic retinopathy ?
The patient groups specified were those with early stages of NPDR versus the control or comparator treatment of PRP at PDR , in any appropriate setting.
Our scoping searches gave a very low retrieval of studies that would be relevant to this search question, but did show that there were recent developments in types of laser and in the use of laser and drug combinations. Therefore, in the draft protocol we proposed a wider scope for this Technology Assessment Report than had been envisaged in the commissioning brief. This was approved by the NIHR Evaluation, Trials and Studies Coordinating Centre after being supported by the external referees. The decision problem was subsequently expanded to become:
Treatment of non-proliferative diabetic retinopathy: a review of pan-retinal photocoagulation, other forms of laser treatment, and combinations of photocoagulation and anti-VEGF drugs or inject steroids.
However, the broader searches revealed that there were no RCTs that compared patients at the NPDR level to those at later stages of PRP. Indeed, the most relevant and largest study done addressing the timing of PRP laser in the treatment of DR, the ETDRS, grouped together patients with moderate to severe NPDR and early PDR, and did not report outcomes on these groups separately.
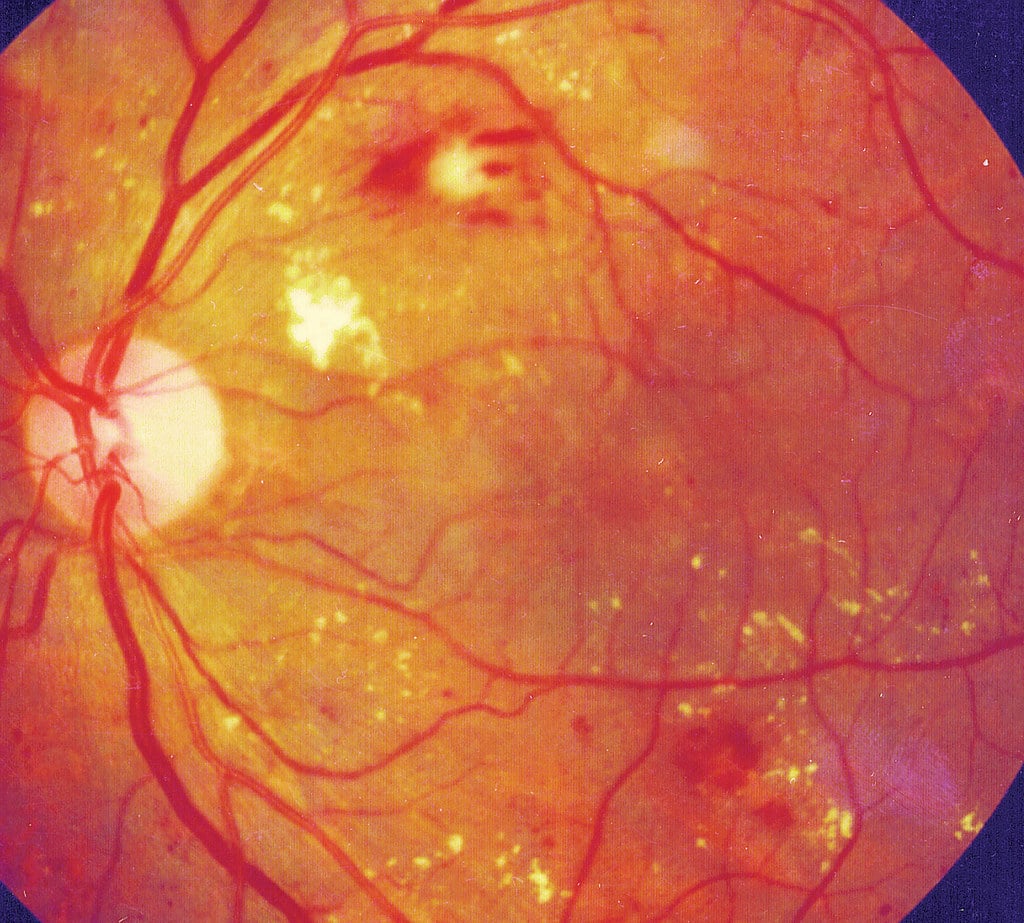
Stage : Moderate Npdr
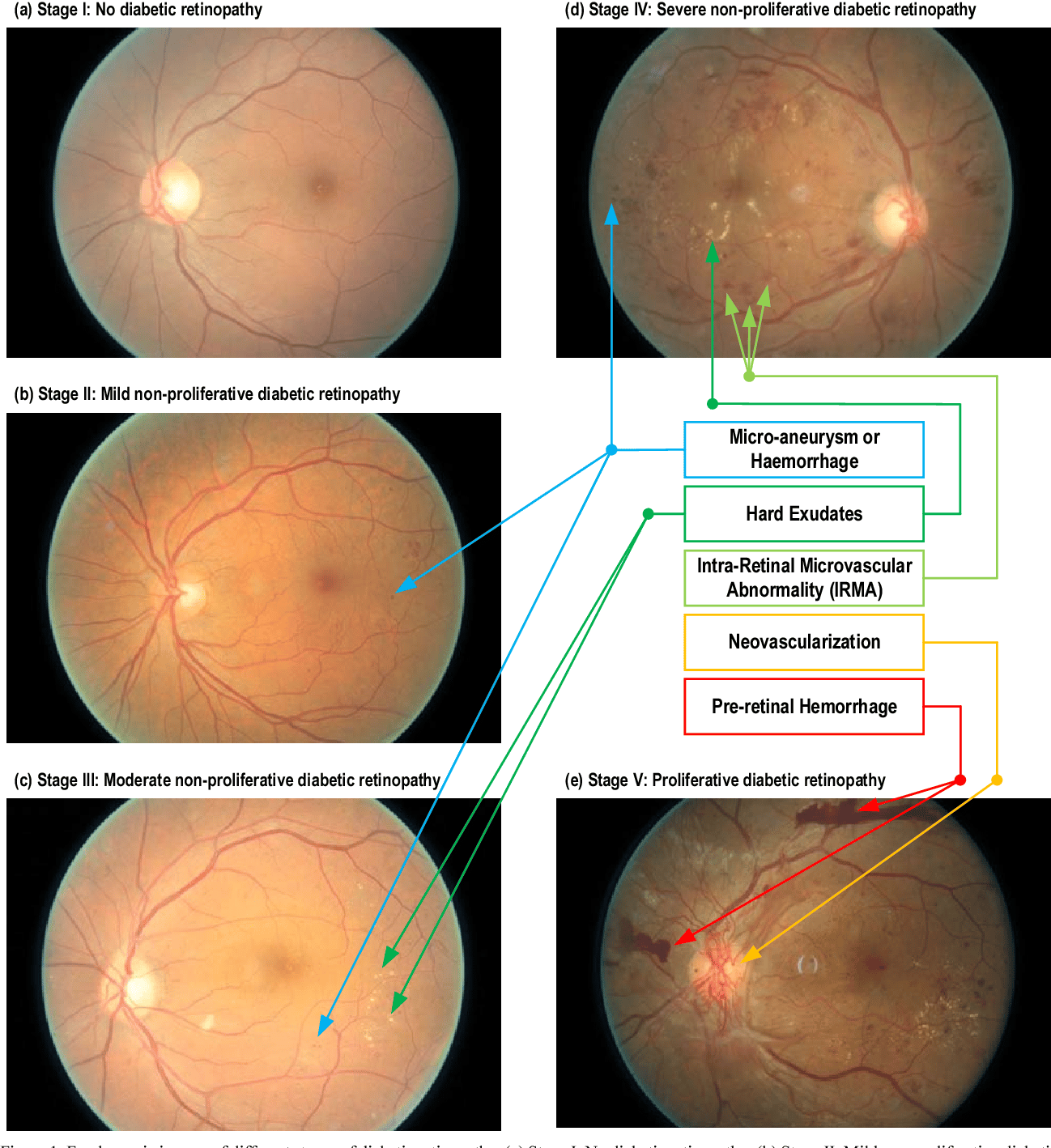
These patients have hemorrhages or MAs in one to three retinal quadrants and/or cotton wool spots, hard exudates, or venous beading .2, 5-7
Figure 2. This patient with type 2 diabetes has moderate NPDR and macular edema. Note the MA and hard exudates within the macula and the moderate, scattered dot hemorrhages throughout both the inferior and superior arcades.
Patients with moderate NPDR should be seen every 6 to 8 months.2,7 There is a 12% to 27% risk that they will develop proliferative diabetic retinopathy within 1 year.2 The use of fundus photography is suggested for these patients, and you may obtain macular OCT images at your discretion if you suspect DME. These patients do not need to be referred to a retina specialist unless you have confirmed DME or you believe OCT imaging is warranted but do not have access to this technology.
Again, it is important to educate these patients on the findings and what they suggest about the disease process. Depending on their recent blood sugar control and last diabetes examination with their PCP or endocrinologist, it may be necessary to refer patients back to those providers sooner than scheduled so that they can consider changes in treatment.
Recommended Reading: Type 1 Diabetes Blood Sugar Levels
My Vision Seems Fine Can I Still Have Diabetic Retinopathy
Yes. Often there are no visual symptoms in the early stages of nonproliferative diabetic retinopathy. The vision usually deteriorates as progressive damage occurs to the vessels in the central part of the retina, called the macula. Diabetic injury to the blood vessels in the macula can cause swelling or ischemia nerve damage from lack of blood flow. It is important not to wait for symptoms to occur before having your eyes examined for diabetic damage. Treatments to preserve your vision from diabetic damage are much more successful if the disease is consistently monitored and treated in its earlier stages
Dos And Donts In Managing Diabetic Retinopathy:
- DO watch your diet to control blood sugar levels.
- DO remember that untreated diabetic retinopathy can cause severe vision loss and blindness.
- DO remember that macular edema may need focal laser treatment more than once.
- DO call your health care provider if you have symptoms of uncontrolled diabetes .
- DO call your health care provider if you notice vision changes.
- DONT smoke or drink alcohol.
- DONT wait until you have symptoms. Get yearly eye examinations.
- DONT forget that proliferative retinopathy and macular edema can develop without symptoms.
Also Check: Simple Diabetic Diet Meal Plan
Diabetic Retinopathy: Symptoms Treatment Prevention
Diabetic retinopathy is when diabetes causes retinal damage, potentially affecting vision.
The retina is a tissue layer at the back of the eye that captures and sends information to the brain, enabling you to see. Damage can occur when retinal blood vessels swell, leak or clog.
When your retina malfunctions due to diabetes, you may experience a degree of vision loss. Early treatment and diabetes control can halt or even reverse retinopathy, preventing complete blindness.
What To Look For
Patients with NPDR generally present with hemorrhages of varying sizes, microaneurysms , hard exudates, soft exudates intraretinal microvascular abnormalities , and venous looping or beading.2,5,6 MAs are saccular outpouchings of retinal capillaries that have been weakened by a loss of intramural pericytes.4 The weakened capillary walls can leak or rupture, causing hemorrhages.2 IRMAs are either new vessel growth within the retina or preexisting vessels with proliferative endothelial cells that are moving through areas of nonperfusion. Presence of IRMA indicates ischemia and is a precursor to neovascularization.2 Venous looping and beading are caused by severe retinal hypoxia and indicate an increased risk for progression to neovascularization.2 When patients with diabetes are in your chair, its important to gather as much information about their condition as possible .
Also Check: How Many People In The Us Have Type 1 Diabetes
How Is The Diagnosis Of Nonproliferative Diabetic Retinopathy Made
The first step is a careful eye exam where both pupils are dilated. To supplement the direct examination of your eye with lights and lenses, the circulation of the retina can be carefully assessed with a special test called a fluorescein angiogram. This is a photographic study of the back of the eye performed after an orange-colored dye is injected in a vein in the hand or arm. The dye circulates through the body into the eye to highlight abnormal vessels, or where treatment may be needed. In addition, the degree and extent of damage to the center of the retina, called the macula, can be evaluated by a painless retina imaging system called an optical coherence tomography scan .
Screening Of Patients For Dr
Sight-threatening DR is an important cause of visual impairment in patients with diabetes and one of the most common causes of avoidable blindness. Regular dilated fundus examination is the first step in the identification and management of STDR.24 Patients with no DR and mild NPDR are considered non-referable, whereas patients with or above moderate NPDR with or without macular oedema are considered referable DR Identification of DR in the early stages not only helps in preventing blindness but is also cost-effective for patients . The main aim of screening for DR is timely detection of STDR.25
Also Check: Onetouch Verio Flex Blood Glucose Meter