What Are The Risks Of Islet Cell Transplantation
As with all organ and tissue transplants, rejection of the donor cells is the greatest challenge. The immune system serves to protect the body from “invading” substances that do not belong — bacteria and viruses, for example. Even though the transplanted islet cells are beneficial, the recipient’s immune system recognizes it as “foreign” and tries to destroy it. This attack on the donor tissue is called “rejection.”
All transplant recipients must take, for the rest of their life, strong drugs to suppress the immune response and prevent rejection. Many of these drugs have serious side effects. The long-term effects of these immunosuppressive or anti-rejection drugs are not yet known, but it is suspected that they may increase the risk of cancer.
Prevention Of Severe Hypoglycemic Events
Finally, the restoration of hypoglycemia awareness may be due to a behavioral training effect based on early hypoglycemia intervention through conventional therapy or transplantation rather than a direct effect of the islet graft. That would explain why some islet recipients continue to be protected from severe hypoglycemia even after the islet graft has failed, as determined by negative c-peptide levels.
With improved glycemic control and reduction of SHE, islet transplantation resulting in persistent graft function with or without insulin independence significantly improves the recipient’s quality of life. The burden of daily diabetes management has been shown to be a significant cause of distress and depression in patients with Type 1 Diabetes. This is probably most pronounced in patients that repeatedly experienced SHE and developed anxiety surrounding diabetes management.
Islet Transplantation Using Non
Because islet transplantation is considered tissue transplantation and not organ transplantation, BDD cannot be used for islet transplantation in Japan. Non-heart beating donors are a possible alternative donor source, but islet isolation from NHBD is difficult.
In order to initiate islet transplantation in Japan, we undertook research to isolate islets from NHBD using pig pancreata.- We developed the Kyoto Islet Isolation Method for NHBD pancreata, which involves: in situ cooling of the pancreas pancreatic ductal preservation using a modified Kyoto solution – two-layer pancreas preservation using modified Kyoto solution, and oxygenated perfluorocarbon and density-adjusted iodixanol-based islet purification., Using this technique, we were able to obtain an average of more than 400000 islet equivalents from a pig pancreas with more than 20min warm ischemia. Based on the Edmonton protocol, 400000IE is sufficient to transplant a patient weighing up to 80kg.
We initiated clinical islet transplantation in 2004 using the Kyoto Islet Isolation Method in Japan at the Kyoto University. Three out of five multiple infusion patients became insulin free. All transplanted patients had improved glycemic control and fewer hypoglycemic episodes. Importantly, more than 80% of the islet isolations were successful .
Read Also: Menu For Someone With Diabetes
Anterior Eye Chamber Transplantation Site
The anterior chamber of the eye has been gaining considerable interest as an alternative site for islet transplantation because of its accessibility, highly vascularized oxygen supply, and immune-privileged character. A previous study demonstrated that in mouse and non-human primate models of T1D, intraocular islet transplantation showed superior efficacy and immune modulation that improved hyperglycemia more in the long-term than that of the liver transplantation site. Although clinical trials in humans are currently planned for patients with T1D who are legally blind in the eye where the islet is to be transplanted, it is not known how the graft islets in the ACE affect vision and related neural systems. This may limit the opportunity for intraocular islet transplantation in non-blind T1D patients. Nevertheless, this transplantation method is also beneficial for the non-invasive monitoring of graft survival. It has been demonstrated that the ACE allows for adequate engraftment of tissues from the heart, muscles, pituitary gland, liver and prostate . The dense vascularization of the iris allows for rapid angiogenesis of transplanted tissue contributing to the successful engraftment and survival of the graft . This site also offers the advantage of the graft being visualized non-invasively through the see-through cornea. The same advantages of ease of access, vascularization, innervation, and immune privilege also apply for pancreatic islet transplantation into the ACE.
Leading Diabetes Treatment & Research For 100 Years
Breakthroughs made at the University of Chicago Medicine have shaped today’s treatment of diabetes. Notably, one of our researchers played a crucial role in the discovery of insulin an event that has saved countless lives of people with Type 1 diabetes. More recently, we were the first hospital in Illinois to perform a pancreas transplant for a patient with advanced diabetes. Currently, we are also testing another exciting, but experimental, treatment for Type 1 diabetes known as islet transplantation.
You May Like: I Am Type 2 Diabetes
Islet Transplantation And The Importance Of Pre
In recent years, the clinical applicability of pancreatic islet cell transplant has gained momentum as a possible alternative to pancreas transplant due to the relative safety of the procedure and approaching results similar to SPK . Allogeneic islet transplantation is indicated for patients with type 1 diabetes complicated by severe hypoglycemia and hypoglycemia unawareness or marked glycemic lability, or for patients already on chronic immunosuppression in support of a kidney transplant. In such patients, islet transplantation has been proven effective in restoring hypoglycemia awareness and abolishing severe hypoglycemic episodes . Furthermore, islet transplantation appears to be a valid option for patients with severe, unstable T1D who are not responding to intensive insulin therapy . In addition, recent observational evidence suggested that islet transplantation is not associated with increased mortality regardless of the use of long-term immunosuppressive therapy .
What Are The Risks Of Islet Transplantation
Risks of islet transplantation include
- bleeding, blood clots, and pain after the procedure
- the chance that the transplanted islets may not work well or may stop working
- side effects of anti-rejection medicines, also called immunosuppressants, which are described below
- development of antibodies against the donor cells that may make it more difficult to find an appropriate organ donor if another transplant is needed in the future
Also Check: What To Give A Diabetic When Blood Sugar Is Low
Difference Vs Pancreas Transplant
While an islet cell transplant involves the transfer of cells from a donor pancreas, a pancreas transplant involves a person receiving a whole, healthy donor pancreas. Typically, the original pancreas will remain in the body, and the surgeon will connect the new pancreas to the intestines so that it can carry out its functions.
Often, people receiving a pancreas transplant will also receive a kidney, due to frequently coexisting kidney damage relating to type 1 diabetes. Evidence notes that roughly 80% of current pancreas transplants occur with a kidney transplant, and around 73% of people who receive this transplant become insulin independent after 5 years.
However, a pancreas transplant is a more invasive procedure, and as such, carries more risk and potential complications.
Research suggests that islet cell transplants may be a more promising option due to their lower surgical risk and lower toxicity from immunosuppressants, and may provide better glycemic control. However, more research is necessary to evaluate the long-term results for this option.
Pancreas And Islet Transplantation In Type 1 Diabetes
American Diabetes Association Pancreas and Islet Transplantation in Type 1 Diabetes. Diabetes Care 1 April 2006 29 : 935.
This position statement presents the recommendations of the American Diabetes Association on pancreas and islet transplantation in patients with type 1 diabetes. The recommendations are based on an ADA technical review and recent extensive review on the subject , which should be consulted for further information.
Successful pancreas transplantation has been demonstrated to be efficacious in significantly improving the quality of life of people with diabetes, primarily by eliminating the acute complications commonly experienced by patients with type 1 diabetes . Pancreas transplantation also eliminates the need for exogenous insulin, frequent daily blood glucose measurements, and many of the dietary restrictions imposed by diabetes. Pancreas transplantation is only partially successful in reversing or stabilizing the long-term renal and neural complications of diabetes. However, this procedure is usually performed after 20 years of established diabetes. No data are available to determine whether transplantation earlier in the course of the disease would prevent complications, as would be anticipated given the results of the Diabetes Control and Complications Trial.
Also Check: Boost Or Glucerna For Diabetics
Islet Transplantation: Edmonton Protocol
The landmark trial of islet transplantation in 2000 by the Edmonton group demonstratedsuccessful reversal of diabetes in seven consecutive type I diabetes patients. Thetrial utilized induction immunosuppression with daclizumab and maintenance with a glucocorticoid-free immunosuppressiveregimen consisting of the calcineurin inhibitor tacrolimus and the mTOR inhibitorsirolimus. The islet transplant recipients had suffered from recurrent severehypoglycemia. After transplantation, insulin treatment was stopped if serum glucosereached > 200mg/dL, another transplantation was performed. All seven patientsrequired second islet transplantations, while one required a third. Theinvestigators did not observe any acute rejection and recorded only mild sideeffects due to the immunosuppression, such as sirolimus-induced superficial buccalulcerations. At 1 year of follow-up, all seven patients were insulin-independent,their serum glucose levels showed less fluctuation, and none suffered episodes ofsevere hypoglycemia. However, longer follow-up revealed progressive loss of betacell function and recurrence of diabetes. In a trial of 65 patients conducted by theEdmonton group in 2004, only 10 percent of the patients remained insulin-independentat 5 years, although partial graft function persisted in 80 percent of the patients.
When Insulin Isnt Enough: The Need For Alternative Therapies In Type Idiabetes
Type I diabetes mellitus is a chronic autoimmune disease resulting from selectivedestruction of insulin-producing beta cells in the islets of Langerhans. The absolutedeficiency of insulin results in a wide spectrum of metabolic dysfunction,particularly impaired glucose homeostasis. The discovery of insulin in 1922 was amonumental achievement, transforming type I diabetes mellitus from a death sentenceto a manageable, chronic condition. The Diabetes Control and Complications Trial confirmed that tight glucose control prevents or even reverses long-termcomplications of type 1 diabetes . However, insulin therapy itself can be life-threatening, as anoverdose can result in severe hypoglycemia. In fact, tight glucose control isassociated with more frequent episodes of hypoglycemia, especially in patientsduring acute illnesses .Many patients experience wide excursions in plasma glucose levels that lead to thesecondary complications of diabetes, since most existing insulin formulations cannotmimic the natural regulatory ability of the insulin-producing beta cells of theendocrine pancreas. Of note, more recent innovations in insulin delivery andtherapy, such as insulin degludec has been shown to potentially mimic normal body glycemiccontrol better than existing 24 hour-based regimens using long-acting insulin analogglargine .
Don’t Miss: Blood Testing Meters For Diabetes
Can Islet Cell Transplantation Be Done At Any Hospital
Because it is still considered an experimental therapy, islet cell transplantation for diabetes is not widely available. There are currently 17 U.S. centers participating in islet cell research programs. The American Diabetes Association recommends that pancreas or islet cell transplantation be performed only in certain major centers, which are best equipped to handle the complex and long-term medical and personal needs of transplant patients.
Islet Cell Transplants For Type 1 Diabetes
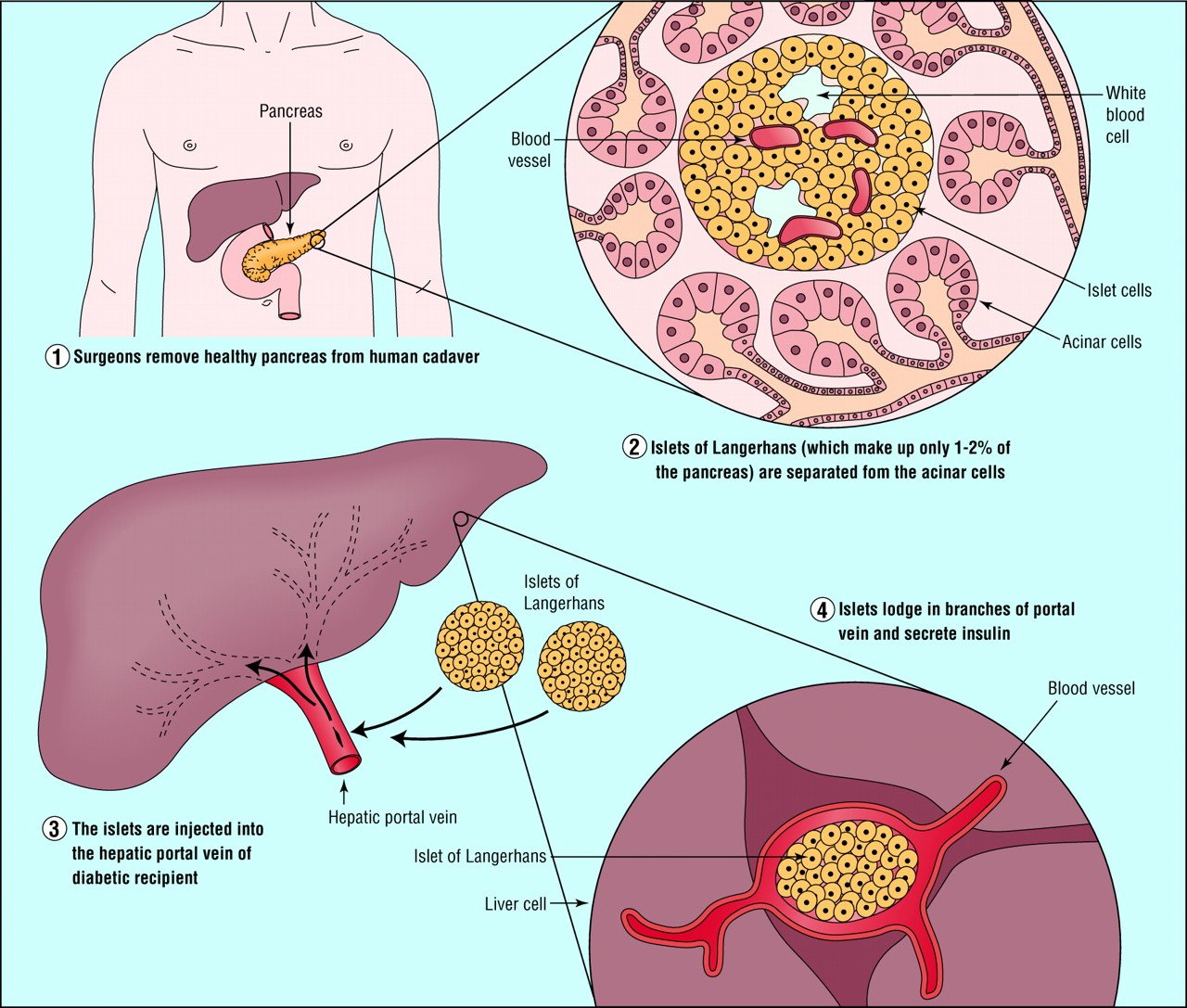
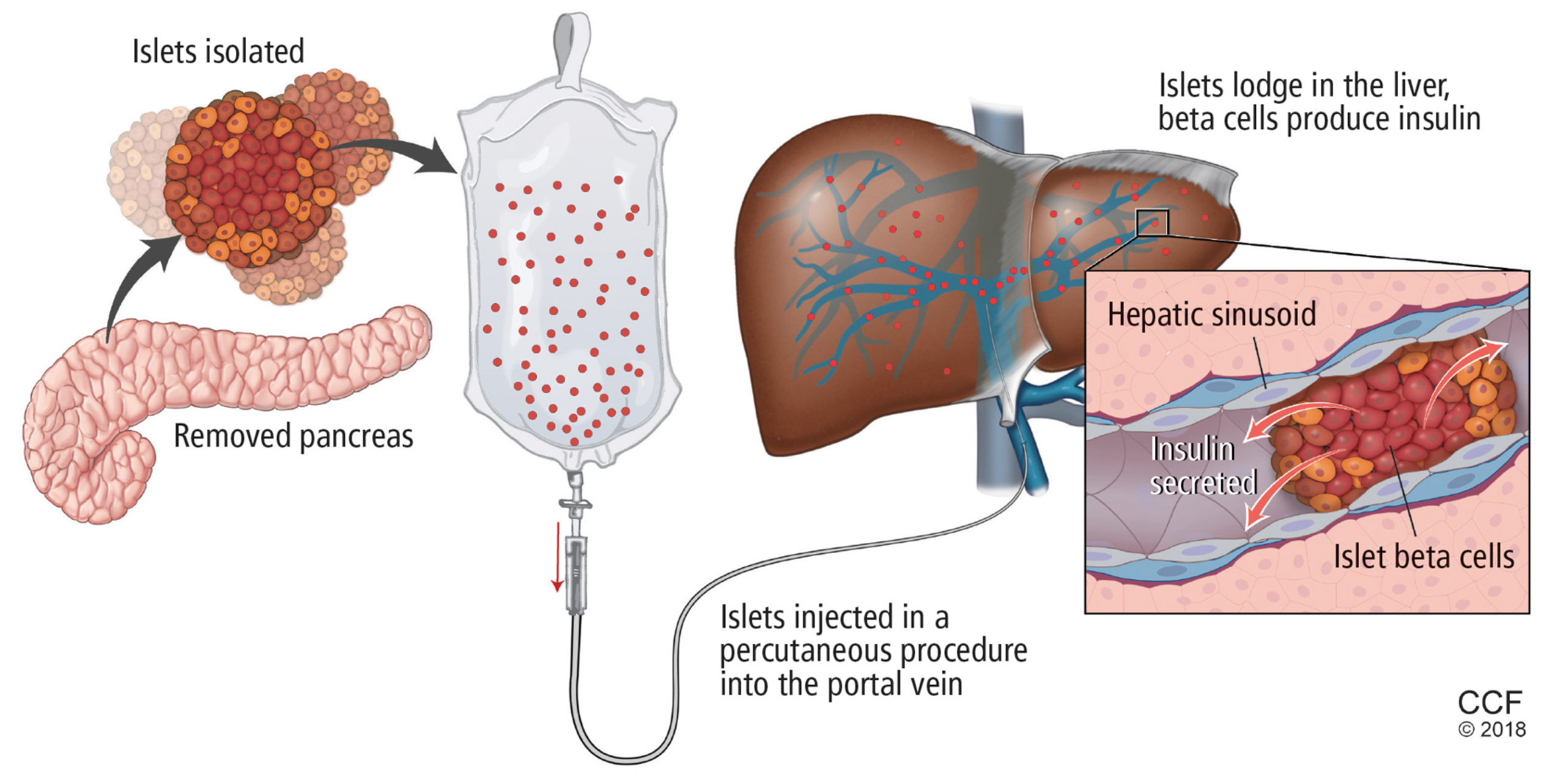
Type 1 diabetes is caused by the destruction of insulin-producing cells in the islets of the pancreas. Islet cell transplantation involves extracting islet cells from the pancreas of a deceased donor and implanting them in the liver of someone with type 1.
This minor procedure is usually done twice for each transplant patient, and can be performed with minimal risk using a needle under local anaesthetic.
In 2008, the UK launched the first government-funded islet transplant programme in the world. As of March 2015, 152 islet transplants had been performed in the UK since the launch. Islet cell transplants are now available through the NHS for people who satisfy the criteria given below.
Don’t Miss: Can You Lose Weight If You Have Diabetes
Alternative Sources Of Insulin
Improving the availability of insulin-producing cells can also be achieved through the generation of -cells from human pluripotent stem cells. In a pivotal study by DAmour et al, human pancreatic hormone-producing cells were developed in vitro from a human pluripotent stem cell source. Examination of the insulin-expressing cells in these cultures, however, revealed a polyhormonal and nonfunctional phenotype.82 Subsequent to these studies, Kroon et al developed pancreatic endoderm derived from human embryonic stem cells. Notably, functional endocrine cells were generated in vivo when pancreatic endoderm was engrafted in immune compromised mice. The insulin-expressing cells generated postengraftment exhibited properties of functional -cells and were capable of restoring normoglycemia when transplanted in diabetic mice.83 These studies were fundamental in the establishment of a robust methodology for consistent, large scale production of this cellular source by Schulz et al84 which will undoubtedly serve as a platform to circumvent cadaveric donor shortages by providing a potentially unlimited supply of insulin-producing cells for clinical application.
Role Of Regenerative Medicine And Stem Cell Research
A new, attractive approach for reversing diabetes is -cell regeneration from original pancreata. Using gene therapy for -cell regeneration has potential, yet a major concern is the use of viral vectors for gene delivery. Recently, a method was developed for gene delivery without using viral vectors. This technique involves the incorporation of plasmids into the phospholipid shell of gas-filled microbubbles, which are then infused through the veins and destroyed within the pancreatic microcirculation by ultrasound. This method is called ultrasound targeted microbubble destruction . Grayburn et al. demonstrated that delivery of betacellulin and pancreatic duodenal homeobox-1 using UTMD could reverse streptozotocin-induced diabetes in rats. Once the effectiveness of UTMD is confirmed in large animal models, it can be applied in clinical trials.
-Cell generation from embryonic stem cells or induced pluripotent stem cells is another interesting approach. If the -cells can be made from a patients own cells, immunosuppression is not necessary. The establishment of iPS cells from human tissue had a significant impact on the regenerative medicine field. Because there are ethical issues associated with the use of ES cell therapies, iPS cell research is likely to take the lead in this field. Considerable research efforts are currently underway with iPS cells. However, there are still many challenges ahead before iPS cells are considered as a potential cure for diabetes.
Also Check: Mellitus Type 2 Diabetes Definition
Alternative Islet Transplantation Sites
Today, intrahepatic islet infusion via the portal vein accounts for virtually all clinical islet transplants conducted worldwide. While percutaneous portal vein infusion offers a minimally invasive procedure with the ability to regulate glycemic levels through portal insulin delivery,70 it is not without potential procedural risks such as portal thrombosis and bleeding.71 A significant amount of intraportal islet mass is lost immediately post-transplant due to innate immune pathways involving platelet and complement activation described in the Islet engraftment section. As such, extrahepatic islet transplantation has drawn focused attention recently to identify an optimal site to achieve sustained post-transplant insulin independence.
An ideal engraftment site should provide an adequate space to accommodate a large volume of transplanted islets, within close proximity to vascular networks supplying sufficient oxygen and nutrients during the revascularization period. Moreover, the site should prevent early islet loss due to host inflammatory reactions, while also providing accessibility for transplantation procedures and retrievability, if necessary.72 Retrievability is paramount should insulin-producing stem cells therapies be translated into clinical practice.
Can Anyone With Diabetes Get An Islet Cell Transplant
Typically, candidates for islet cell transplantation are between the ages of 18 and 65, have had type 1 diabetes for more than 5 years, and are experiencing diabetes-related complications, such as frequent periods of unconsciousness due to lack of insulin and early signs of kidney problems that could lead to kidney failure.
As with all medical procedures, the benefits and risks must be weighed carefully. Transplantation is reserved for those with serious complications of diabetes.
Also Check: Type 1 Diabetes Blurred Vision
Immune Suppression Medication Regimens
On the other hand, anti-CD3, ATG and alemtuzumab may help to restore immunological tolerance towards islet antigens by enhancing Treg cells and shift the balance away from effector cells towards a tolerogenic phenotype . Toso et al. have studied the frequency of different fractions of immune cells within peripheral blood of islet recipients compared after induction of immunosuppression using either a depleting agent or a non-depleting antibody . Both alemtuzumab and ATG led to prolonged lymphocyte depletion, mostly in CD4+ cells. Unlike daclizumab, alemtuzumab induced a transient reversible increase in relative frequency of Treg cells and a prolonged decrease in frequency of memory B cells . Positive effect of alemtuzumab on Treg cells has been further proved by in vitro exposure of peripheral blood mononuclear cells to this immunosuppressant . An anti-CD3 mAb was also shown to induce regulatory CD8+CD25+ T cells both in vitro and in patients with T1D .
In the study of Bellin et al., co-administration of TNF- inhibitior at induction led to a higher insulin independence rate. This result could be attributed to the protective effect of the TNF- inhibitior against detrimental action of TNF- on transplanted islets at the time of infusion in addition to its inducing impact on Treg expansion .
Islet Cells Are Transplanted Into The Liver
In case youre wondering where doctors put the cells, that would be the portal vein, located in the upper right quadrant of your abdomen, that drains into your liver. Its used for many other procedures which means the process for transplanting and delivering into this vein is well established, explains Grunberger.
The portal vein is the easiest place to reach because its large and it provides adequate blood supply. Once transplanted, the islet cells need both oxygen and glucose for survival, which means exposing the cells to healthy blood is critical for their survival the cells can get destroyed It doesnt make a difference where you put those cells as long as there is an adequate blood supply.
Don’t Miss: How To Lower Blood Sugar Immediately Without Insulin