Total Daily Insulin Requirement
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
How To Take Bolus Insulin
Bolus insulin can be given via syringe, pen, inhalation, pod, pump, and patch pump.
When taking bolus insulin, you will need to calculate how much to dose according to either your meal size, the number of carbs in your meal, or how much you need to correct high blood sugars. For information on how to inject insulin, specifically, check out our guide here.
With your doctor, you can determine how much insulin you need on other factors including your weight and activity levels. Your doctor may also help you determine your insulin-to-carb ratio and insulin corrective factors, which will help you figure out how much insulin to take per a certain number of carbs and how much insulin is needed to bring you glucose within range.
Indications For The Basal
The basal-bolus insulin regimen should be considered in the following scenarios :
Suboptimal blood glucose control with oral glucose-lowering drugs and/or basal insulin and/or premixed insulin.
Use of oral glucose-lowering drugs is not safe due to underlying organ dysfunction.
Initiation or escalation of oral glucose-lowering drugs is likely to cause delay in achieving normoglycaemia and adversely affect clinical outcomes.
Transition from intravenous insulin infusion to a subcutaneous insulin regimen.
Patient was already using this regimen prior to hospital admission.
Recommended Reading: T Slim Insulin Pump 3ml Cartridge
When To Consider Using Basal
If you have type 1 diabetes, you will require a combination therapy called basal-bolus insulin. This therapy includes an injection of rapid or fast-acting insulin before meals, as well as a daily injection of background basal insulin. Because your body doesnt make insulin, its key to work with your doctor to come up with an effective treatment approach.
Research Design And Methods
In this multicenter, prospective, open-label, randomized study, we enrolled 130 nonsurgical, insulin-naive patients with a known history of diabetes for > 3 months, aged 1880 years, and admitted to medical general services with a blood glucose level between 140 and 400 mg/dl. Further inclusion criteria included diabetes treatment with either diet alone or any combination of oral antidiabetic agents and the absence of diabetic ketoacidosis . Exclusion criteria included subjects without a known history of diabetes, intensive care unit patients, the use of corticosteroid therapy, subjects expected to undergo surgery during the hospitalization course, patients with clinically relevant hepatic disease, serum creatinine 3.0 mg/dl, pregnancy, and any mental condition rendering the subject unable to understand the scope and possible consequences of the study.
This study was conducted at Grady Memorial Hospital in Atlanta, Georgia, and at the Jackson Memorial Hospital in Miami, Florida. The institutional review boards at Emory University and the University of Miami approved the study protocol. All patients were managed by members of the internal medicine residency program, who received a copy of the assigned treatment protocol. The primary care team decided the treatment for the medical problem for which patients were admitted. No follow-up visit after discharge was included in this study. A teaching endocrinologist rounded daily with the house officers.
Don’t Miss: How Do You Treat Diabetic Sores
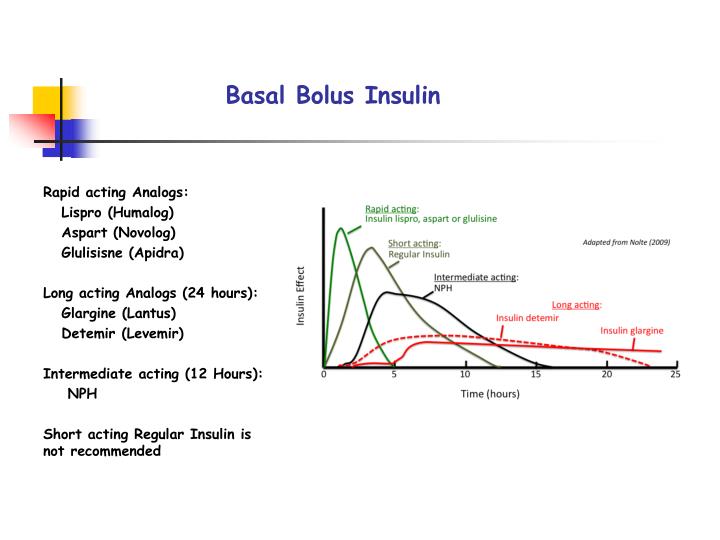
Types Of Basal Insulin
Most basal insulin is injected into the fat just under your skin. You can do that with a needle and syringe to draw the right amount of medication. You also can use prefilled disposable pens that many people find easier to use.
Basal insulin is delivered in three main types. They differ on how soon they start working , how long they last, and when the insulinâs effects peak in your body.
Your doctor may prescribe a mix of insulin types for use throughout the day, depending on how much your blood sugar rises and falls, and on your lifestyle.
Intermediate-acting
NPH . This can start working as quickly as an hour or two. It reaches its maximum effect in 4-12 hours and stays in your body for up to 24 hours.
Long-acting
Detemir and glargine . These take about 2 hours to get into your bloodstream. Effects last about 24 hours. Long-acting basal insulin doesnât really hit a peak. That can help match how your body would release insulin if it were able to.
Ultra-long-acting
Degludec and glargine u-300 . These start to work in 1-6 hours. They can last 36 hours or more. Ultra-long-acting insulin doesnât peak. That means its effect stays even instead of rising and falling.
What Is Basal Insulin Benefits Side Effects Types And Everything Else You Need To Know
Your body needs insulin to function properly, and the right dose of basal insulin may be the answer to stabilizing your blood sugar and avoiding diabetes complications.
Thinkstock
Insulin is a hormone that everyone needs. It allows the body to use sugar properly. But if you have type 1 diabetes or type 2 diabetes, your body doesnt make or use insulin properly, which means you may have to give yourself insulin injections on a daily basis.
Insulin isnt one-size-fits-all. There are different insulins you can use to control your blood sugar levels, and theyre classified by how quickly they work. Basal insulin is one type of therapy. And if you require this insulin, its important to understand how it works and how it differs from other types of the drug.
Read Also: Can Diabetics Eat Corn On The Cob
Analogue Versus Human Insulin
Glucose control, adverse effects, cost, adherence, and quality of life need to be considered when choosing a type of insulin. In general, analogue insulin is similar to human insulin in controlling diabetes, although some trials have found higher mean A1C levels in patients taking analogue insulin compared with human insulin. 17 Analogue insulin usually causes less postprandial hyperglycemia and delayed hypoglycemia. 18,19 In a recent meta-analysis, glycemic control was not improved with analogue insulin compared with human insulin, but nocturnal hypoglycemia was reduced.17
An industry-funded cost-effectiveness analysis found that the increased cost of medication is more than off set by the reduction in hypoglycemic events. 20 However, the analysis assumed a cost differential of 14 percent, which is inconsistent with current pricing . 20,21 Cost-effectiveness analyses have differed regarding the long-term cost savings of using analogue insulin in patients with type 2 diabetes, with industry-sponsored studies finding reduced cost22 and government-sponsored studies finding no cost reduction. 23 Measures of adherence and quality of life have been improved with analogue insulin compared with human insulin. 24,25
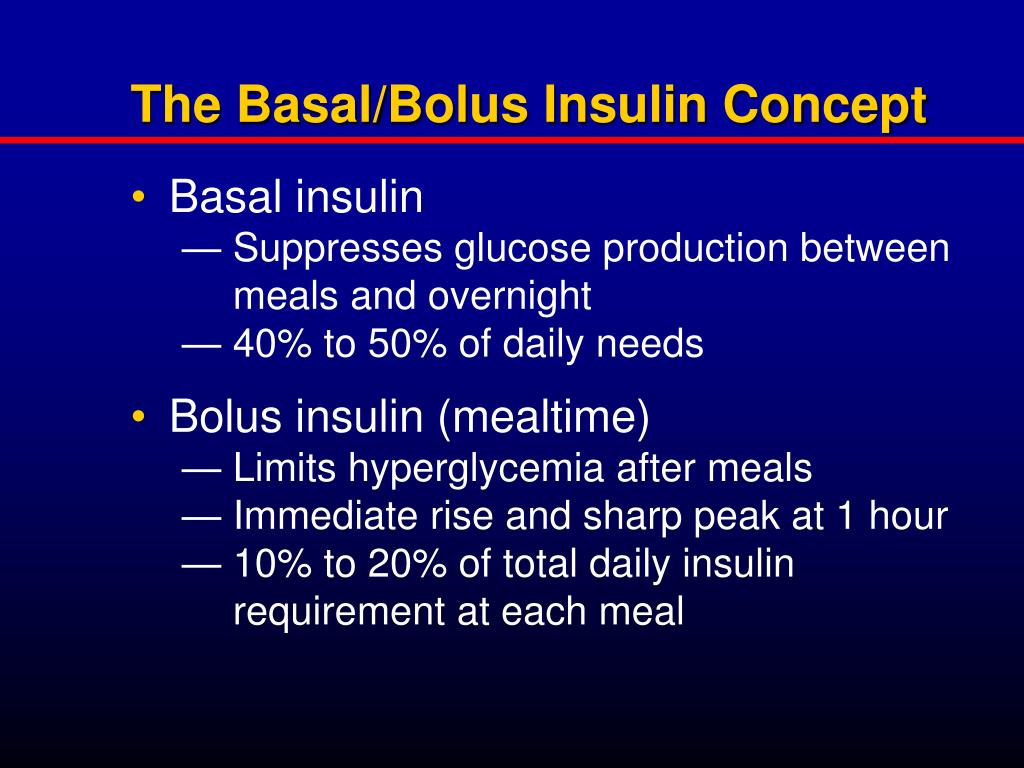
Whats The Difference Between Basal And Bolus Insulin
Along with basal insulin, bolus insulin is a treatment option for type 2 diabetes.
While basal insulin works as a background insulin to supply your body with insulin during periods of fasting, bolus insulin is a rapid or fast-acting insulin that works quickly, but theres a catch: Its blood-sugar-lowering effect doesnt last as long.
Also Check: Type 2 Diabetes Blood Sugar Range
Understanding The Type Of Adjustment Needed
There are four main types of adjustments that can be made to achieve optimal blood glucose control these are: prandial insulin adjustments correctional insulin adjustments, basal insulin adjustments and meals and snacks adjustments. These are described in detail in the following sections.
Prandial Insulin Adjustments
It is also important to understand that the postprandial blood glucose value should not be lower than the preprandial blood glucose value as this situation increases the chances of hypoglycaemia. In such a scenario, if the meal intake was adequate and there were no other factors which could explain the fall in blood glucose , the dose of prandial insulin should be reduced. A dose reduction should be strongly considered if postprandial blood glucose is< 100 to 120 mg/dl or hypoglyceamia occurs in the postprandial period. As a general strategy, if postprandial blood glucose is less than preprandial blood glucose by 20 mg/dl , then prandial insulin should be decreased by 1 unit if the difference exceeds 20 mg/dl , prandial insulin should be decreased by 2 units . Prandial insulin adjustment is explained in the context of various case scenarios in Table 6.
Table 6 Examples of prandial insulin adjustments for a 45-year-old man receiving a total daily insulin dose of 40 units
Correctional Insulin Adjustment
Table 7 Correction factor for the use of correctional insulin in patients with uncontrolled preprandial blood glucose
Taking Nph At Bedtime In The Morning Or Both
This approach can be valuable because the insulin peaks during the predawn and afternoon hours, when its needed most. But that peak can be unpredictable depending on your meals, meal timing, and activity level. This may result in low blood sugar levels while youre sleeping or low or high blood glucose levels during daytime hours.
Don’t Miss: Medical Management Of Diabetes Mellitus
What Is The Difference Between Basal And Bolus Insulin
Basal insulin controls blood glucose throughout the day and night. On the other hand, bolus insulin controls blood glucose after eating. Therefore, this is the key difference between basal and bolus insulin. Moreover, basal insulin is slow acting and long-lasting. In contrast, bolus insulin is short-acting or mealtime insulin.
Furthermore, basal insulin is effective for 24 hours, while bolus insulin is effective for 2-4 hours. So, this is also a significant difference between basal and bolus insulin.
Method : Premix Or Split
Postprandial BG excursions can be minimized by changing basal insulin to premix or split-mix insulin that has a mixture of mealtime and intermediate action insulin .1216 The use of premixed insulin is a viable option due to its ease of use and for those who have restrictions based on the complexity of the basal-bolus regimen.7 If a patient has routine meals and prefers not to carry around insulin for lunch, the schedule of premix insulin taken at breakfast and dinner is ideal.
Don’t Miss: Where Do You Give Insulin Injections
Basic Principles Of The Basal
Rationale Basal-bolus insulin regimen implies the use of one or two doses of intermediate- or long-acting insulin and three, or rarely, four doses of short-acting insulin. The basal insulin regulates the rise in blood glucose due to endogenous glucose production through the processes of glycogenolysis and gluconeogenesis, and the bolus insulin prevents the meal-related rise in blood glucose levels.
Pharmacokinetics of Different Insulin Preparations Basal insulin can be classified into: conventional preparations, such as neutral protamine hagedorn insulin, which is intermediate acting , and insulin analogues, such as insulin detemir, insulin glargine and insulin degludec, which are intermediate or long acting . Similarly, bolus insulin can be classified into: conventional preparations, such as regular insulin, which are short acting rapid-acting insulin analogs, such as insulin lispro, insulin aspart and insulin glulisine and ultra-rapid-acting insulin analogues, such as fast-acting insulin aspart . Thus, while regular insulin provides coverage during the post-absorptive period , implying some degree of basal glucose regulation, the action of rapid-acting insulin is mainly limited to the postprandial period .
Table 1 Pharmacokinetic properties of human insulin and insulin analogues following subcutaneous injection
Calculating Basal Insulin Dose
Basal insulin dosage varies widely. Factors such as body weight, activity level, types of foods, amount of endogenous insulin, etc. all play a role. For full insulin replacement, it is generally about 50% of the patients expected Total Daily Dose , however if your patient needs basal insulin alone, you may consider starting with 0.1-0.2 u/kg/day. See for specific dosing recommendations and examples.
Don’t Miss: Type 2 Diabetes Symptoms Diet
Does My Child Need The Same Amount Of Insulin At All Times
Both basal and bolus insulin needs vary from person to person, and may be different at different times of the day. That is, your child may:
- need more basal insulin in the morning than in the afternoon. This variation can be accommodated with different programmed settings if your child uses an insulin pump on injected insulin programs the strategy is to find the best fit for the daily dose of basal insulin.
- have a different I:C ratio for breakfast than for lunch or supper. Children typically need more insulin to cover their breakfast carbs .
- have different insulin sensitivity at different times of the day. You may find that a larger correction dose is needed in the early morning than is needed in the afternoon, for example.
Understanding The Segment Of The Day When Insulin Works
Each insulin dose in the basal-bolus regimen works during a particular segment of the day. Prandial insulin administered before breakfast predominantly acts from breakfast to lunch prandial insulin given before lunch predominant acts from lunch to dinner prandial insulin given before dinner predominantly acts from dinner to midnight and basal insulin given at bedtime predominantly acts from midnight to breakfast . Although there may be some overlap in action, this broad concept helps the clinician to determine the appropriate dose adjustment based upon the demarcation of the segment during which blood glucose targets are not achieved.
Don’t Miss: Normal Blood Sugar For Type 2 Diabetes
Example #: Formulas Commonly Used To Create Insulin Dose Recommendations
This example illustrates a method for calculating of your background/basal and bolus doses and estimated daily insulin dose when you need full insulin replacement. Bear in mind, this may be too much insulin if you are newly diagnosed or still making a lot of insulin on your own. And it may be too little if you are very resistant to the action of insulin. Talk to your provider about the best insulin dose for you as this is a general formula and may not meet your individual needs.
The initial calculation of the basal/background and bolus doses requires estimating your total daily insulin dose:
Concerns About Insulin Therapy
Pain, weight gain, and hypoglycemia may occur with insulin therapy. Pain is associated with injection therapy and glucose monitoring, although thinner and shorter needles are now available to help decrease pain. Weight gain associated with insulin therapy is due to the anabolic effects of insulin, increased appetite, defensive eating from hypoglycemia, and increased caloric retention related to decreased glycosuria. In the U.K. Prospective Diabetes Study, patients with type 2 diabetes who were taking insulin gained an average of 8 lb, 13 oz , which was associated with a 0.9 percent decrease in A1C level compared with patients on conventional therapy.5
Hypoglycemia may occur from a mismatch between insulin and carbohydrate intake, exercise, or alcohol consumption. Hypoglycemia has been associated with an increased risk of dementia and may have implications in cardiac arrhythmia. 6,7 All patients should be instructed on the symptoms and treatment of hypoglycemia. American Diabetes Association guidelines recommend that the blood glucose level be checked if hypoglycemia is suspected , then treated with a fast-acting carbohydrate, such as juice or glucose tablets. The blood glucose level should be rechecked after 15 minutes to make sure it has normalized.8
Read Also: How Do You Get Type 1 Diabetes
What Is The Difference Between Basal Insulin And Bolus Insulin
Basal insulin refers to the insulin required to control your blood sugar in the absence of food intake. A certain amount of insulin is always necessary to keep the blood sugar in the normal range, even in the absence of eating for prolonged periods.
Without any insulin in the body, the starch, fat, and protein in the body will break down with severe health consequences, as occurs in people with type 1 diabetes.
The amount of insulin that the body requires in the absence of food intake is known as the basal requirement and it is pro-vided by the one or two injections of long-acting insulin that most patients give themselves each day. If a person is using an insulin pump, then it is covered by the basal setting on the pump.
Modern insulin pumps offer several basal settings in each 24-hour period, as the basal insulin production in a healthy individual varies over the course of the day, being higher in the 2-to 3-hour period before arising in the morning, for example.
Bolus insulin refers to the insulin required to remove the energy derived from a meal from the bloodstream and into the tissues, to replenish energy stores. This is typically provided by the short-acting insulin injection given just prior to eating or by the bolus setting for patients on an insulin pump.
First Some Basic Things To Know About Insulin:
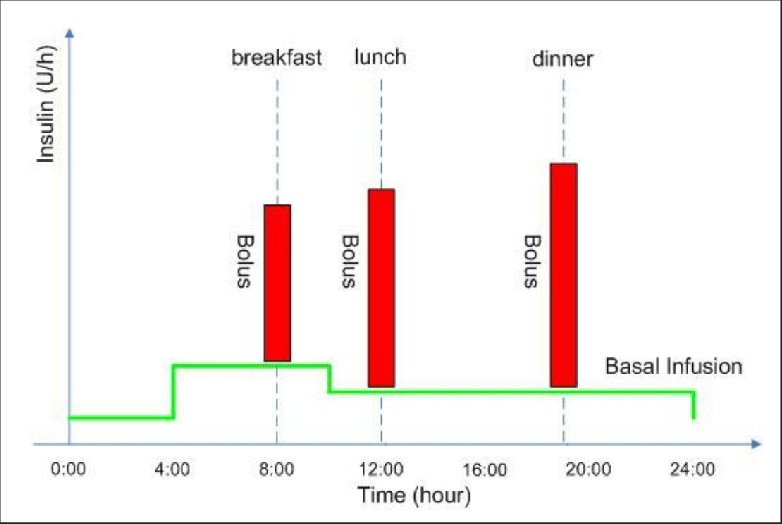
- Approximately 40-50% of the total daily insulin dose is to replace insulin overnight, when you are fasting and between meals. This is called background or basal insulin replacement. The basal or background insulin dose usually is constant from day to day.
- The other 50-60% of the total daily insulin dose is for carbohydrate coverage and high blood sugar correction. This is called the bolus insulin replacement.
Bolus Carbohydrate coverage
The bolus dose for food coverage is prescribed as an insulin to carbohydrate ratio.The insulin to carbohydrate ratio represents how many grams of carbohydrate are covered or disposed of by 1 unit of insulin.
Generally, one unit of rapid-acting insulin will dispose of 12-15 grams of carbohydrate. This range can vary from 4-30 grams or more of carbohydrate depending on an individuals sensitivity to insulin. Insulin sensitivity can vary according to the time of day, from person to person, and is affected by physical activity and stress.
Bolus High blood sugar correction
The bolus dose for high blood sugar correction is defined as how much one unit of rapid-acting insulin will drop the blood sugar.
Generally, to correct a high blood sugar, one unit of insulin is needed to drop the blood glucose by 50 mg/dl. This drop in blood sugar can range from 15-100 mg/dl or more, depending on individual insulin sensitivities, and other circumstances.
Recommended Reading: Average A1c For A Diabetic