Psychological Mechanisms And Adherence
As self-management of diabetes typically involves lifestyle modifications, adherence may pose a significant self-management burden on many individuals. For example, individuals with diabetes may find themselves faced with the need to self-monitor their blood glucose levels, adhere to healthier diets and maintain exercise regimens regularly in order to maintain metabolic control and reduce the risk of developing cardiovascular problems. Barriers to adherence have been associated with key psychological mechanisms: knowledge of self-management, beliefs about the efficacy of treatment and self-efficacy/perceived control. Such mechanisms are inter-related, as one’s thoughts is likely to relate to one’s emotions , which in turn, affects one’s self-efficacy .
As diabetes management is affected by an individual’s emotional and cognitive state, there has been evidence suggesting the self-management of diabetes is negatively affected by diabetes-related distress and depression. There is growing evidence that there is higher levels of clinical depression in patients with diabetes compared to the non-diabetic population. Depression in individuals with diabetes has been found to be associated with poorer self-management of symptoms. This suggests that it may be important to target mood in treatment.
Choosing Specific Diabetes Interventions And Their Roles In Treating Type 2 Diabetes
Numerous reviews have focused on the characteristics of the specific diabetes interventions listed below . In addition, meta-analyses and reviews have summarized and compared the glucose-lowering effectiveness and other characteristics of the medications . The aim here is to provide enough information to justify the choices of medications, the order in which they are recommended, and the use of combinations of therapies. Unfortunately, there is a dearth of high-quality studies that provide head-to-head comparisons of the ability of the medications to achieve the currently recommended glycemic levels. The authors highly recommend that such studies be conducted. However, even in the absence of rigorous, comprehensive studies that directly compare the efficacy of all available glucose-lowering treatments and their combinations, we feel that there are enough data regarding the characteristics of the individual interventions to provide the guidelines below.
An important intervention that is likely to improve the probability that a patient will have better long-term control of diabetes is to make the diagnosis early, when the metabolic abnormalities of diabetes are usually less severe. Lower levels of glycemia at the time of initial therapy are associated with lower A1C levels over time and decreased long-term complications .
Can You Be Born With Diabetes Is It Genetic
You arent born with diabetes, but Type 1 diabetes usually appears in childhood. Prediabetes and diabetes develop slowly over time years. Gestational diabetes occurs during pregnancy.Scientists do believe that genetics may play a role or contribute to the development of Type 1 diabetes. Something in the environment or a virus may trigger its development. If you have a family history of Type 1 diabetes, you are at higher risk of developing Type 1 diabetes. If you have a family history of prediabetes, Type 2 diabetes or gestational diabetes, youre at increased risk of developing prediabetes, Type 2 diabetes or gestational diabetes.
Recommended Reading: Can You Reverse Diabetic Neuropathy
Articles On Treatment Options For Type 2 Diabetes
You have lots of options to manage diabetes. Food, exercise, and medication work together to bring your blood sugar under control.
Your doctor will help you figure out if you need to take medicine, which kind is right for you, and how often you should take it.
Over your lifetime, you’ll probably handle your disease in different ways. Sometimes medications stop working, and you’ll have to switch. You’ll need to adjust to changes in your body as you age. And researchers are looking for new diabetes medicines and ways to treat it.
How To Initiate Diabetes Therapy And Advance Interventions
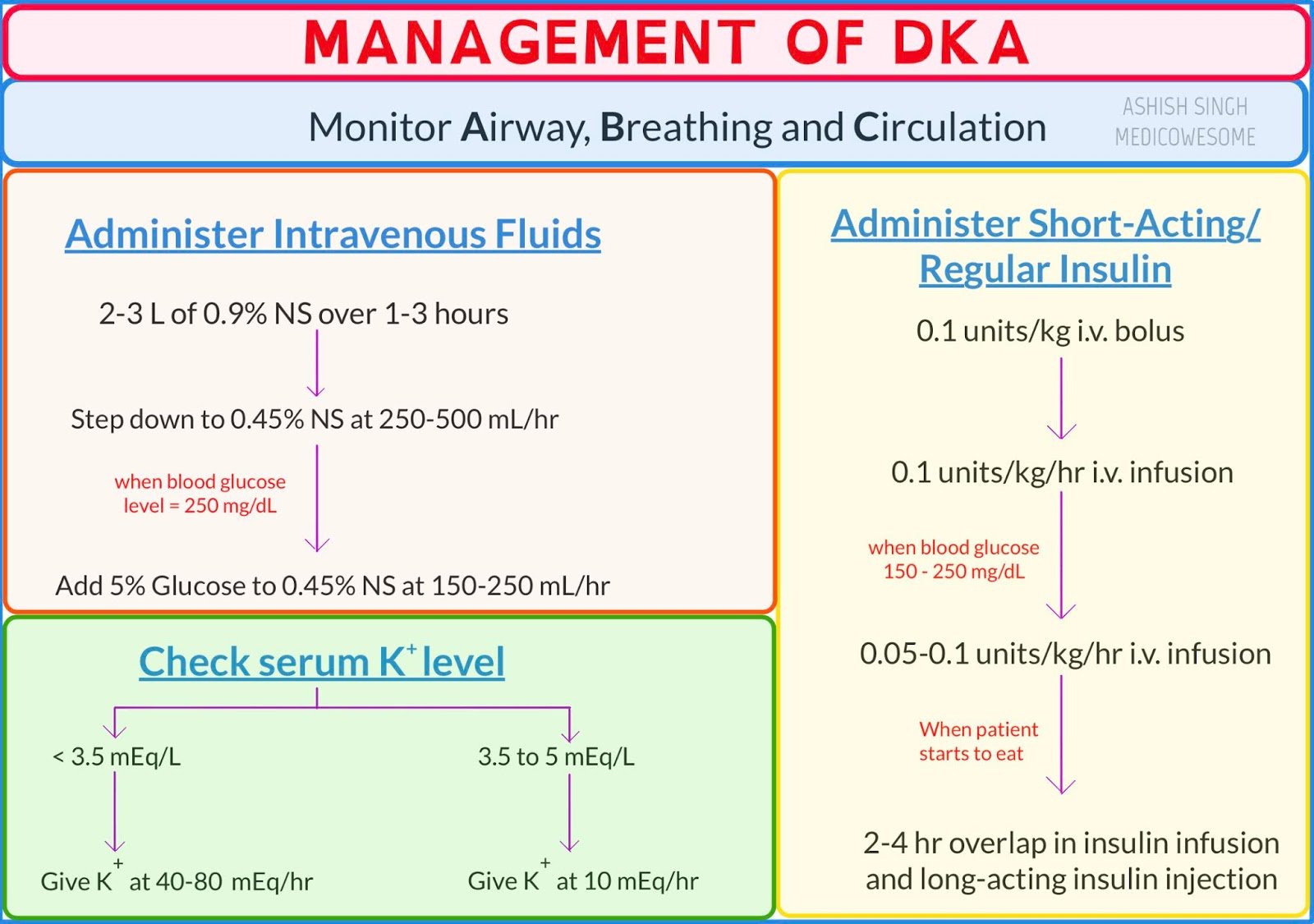
Except in rare circumstances, such as diabetic ketoacidosis or patients who are extremely catabolic or hyperosmolar or who are unable to hydrate themselves adequately , hospitalization is not required for initiation or adjustment of therapy. The patient is the key player in the diabetes care team and should be trained and empowered to adjust medications with the guidance of health care professionals to achieve glycemic goals and to prevent and treat hypoglycemia. Many patients may be managed effectively with monotherapy however, the progressive nature of the disease will require the use of combination therapy in many, if not most, patients over time, to achieve and maintain glycemia in the target range.
The levels of plasma or capillary glucose that should result in long-term glycemia in the nondiabetic target range, as measured by A1C, are fasting and preprandial levels between 3.9 and 7.2 mmol/l . If A1C levels remain above the desired target despite preprandial levels that are in range, postprandial levels, usually measured 90120 min after a meal, may be checked. They should be < 10 mmol/l to achieve A1C levels in the target range.
Recommended Reading: How Many People In The Us Have Type 1 Diabetes
Physical Activity For Patients With Type 1 Diabetes Mellitus
Exercise training in the form of resistance, endurance and combined training consisting of both, has been shown to improve glycaemic control and diabetes outcomes in patients with T1DM in a recent systematic review and meta-analysis. However, we need to keep in mind that there is substantial risk of hypoglycaemia during and after exercise. At times, post-exercise hyperglycaemia is encountered in patients with T1DM because of a surge of counter-regulatory hormones during and after exercise. The insulin treatment may need modification in patients who do only occasional unaccustomed physical activities to prevent these complications.
The benefits of exercise depend on factors such as frequency, duration, intensity, type of exercise, age of the patient and the adherence to the exercise programme. This is collectively termed as the FITT principle: Frequency , Intensity , Time and Type .
Different Methods Of Delivering Insulin
Not only is the variety of insulin preparations growing, so are the methods for administering insulin.
Pre-filled insulin pens
In the twentieth century, insulin was available only in an injectable form that required carrying syringes, needles, vials of insulin, and alcohol swabs. Clearly, patients found it difficult to take multiple shots each day as a result, good blood sugar control was often difficult. Many pharmaceutical companies now offer discreet and convenient methods for delivering insulin.
Many manufacturers offer pen delivery systems. Such systems resemble the ink cartridge in a fountain pen. A small, pen-sized device holds an insulin cartridge . Cartridges are available for the most widely used insulin formulations. The amount of insulin to be injected is dialed in, by turning the bottom of the pen until the required number of units is seen in the dose-viewing window. The tip of the pen consists of a needle that is replaced with each injection. A release mechanism allows the needle to penetrate just under the skin and deliver the required amount of insulin.
Insulin pumps
The most exciting innovation in pump technology has been the ability to combine the pump in tandem with newer glucose sensing technology. This is called sensor-augmented insulin pump therapy.
You May Like: Can You Eat After Taking Insulin
Combination Medications For Type 2 Diabetes
Glyburide/metformin , rosiglitazone/metformin , glipizide/metformin , pioglitazone/metformin , and metformin/sitagliptin are five examples of combination pills on the market to treat type 2 diabetes. There are many, many more combination pills available.
These combination drugs carry the benefit of taking fewer pills, which hopefully improves compliance. While they work well, most health-care professionals initiate individual medications to optimize dosing, before switching to a combination pill once the patient has been stable on individual medications for a while.
Management Of Coronary Heart Disease
There is contradictory epidemiologic evidence as to whether diabetes is in fact a CHD risk equivalent. For the present, however, that is the position adopted by most groups, such as the National Cholesterol Education Program and the ADA.
Although the risk for CHD is 2-4 times greater in patients with diabetes than it is in individuals without diabetes, control of conventional risk factors is probably more important in event reduction than is glycemic control. Control of hypertension, aspirin therapy, and lowering of LDL cholesterol levels are vitally important in reducing CHD risk.
Read Also: Does Insulin Cause Erectile Dysfunction
Drug Treatment Of Diabetes Mellitus
, MD, New York Medical College
. Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia. Early symptoms are related to hyperglycemia and include polydipsia… read more .)
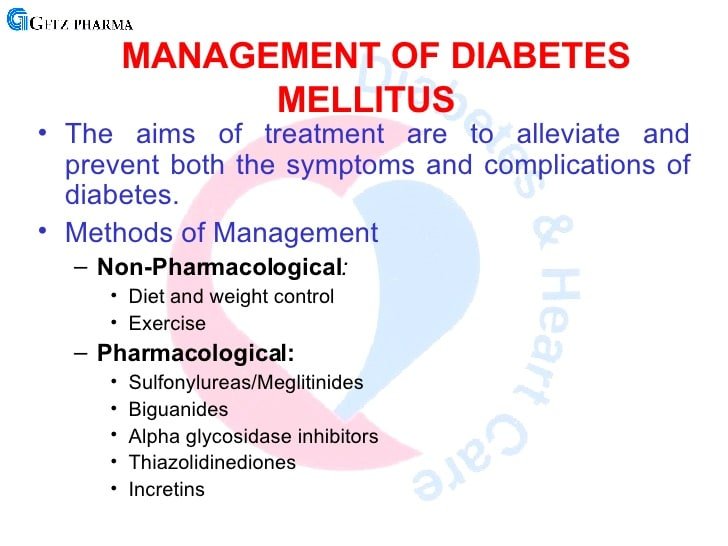
Patients with type 1 diabetes mellitus are treated with insulin as well as diet and exercise.
Patients with type 2 diabetes mellitus are often initially treated with diet and exercise. If those measures are not sufficient for glycemic control, patients may be prescribed oral antihyperglycemic drugs, injectable glucagon-like peptide-1 receptor agonists, insulin, or a combination of these drugs.
. Agents include renin-angiotensin-aldosterone system blockers , statins, and aspirin.
Can Prediabetes Type 2 Diabetes And Gestational Diabetes Be Prevented
Although diabetes risk factors like family history and race cant be changed, there are other risk factors that you do have some control over. Adopting some of the healthy lifestyle habits listed below can improve these modifiable risk factors and help to decrease your chances of getting diabetes:
- Eat a healthy diet, such as the Mediterranean or Dash diet. Keep a food diary and calorie count of everything you eat. Cutting 250 calories per day can help you lose ½ pound per week.
- Get physically active. Aim for 30 minutes a day at least five days a week. Start slow and work up to this amount or break up these minutes into more doable 10 minute segments. Walking is great exercise.
- Lose weight if you are overweight. Dont lose weight if you are pregnant, but check with your obstetrician about healthy weight gain during your pregnancy.
- Lower your stress. Learn relaxation techniques, deep breathing exercises, mindful meditation, yoga and other helpful strategies.
- Limit alcohol intake. Men should drink no more than two alcoholic beverages a day women should drink no more than one.
- Get an adequate amount of sleep .
- Take medications to manage existing risk factors for heart disease or to reduce the risk of developing Type 2 diabetes as directed by your healthcare provider.
- If you think you have symptoms of prediabetes, see your provider.
Don’t Miss: Treatment Of Type 1 Diabetes In Child
Initiation And Titration Of Therapy
All patients with type 1 DM require insulin therapy. There are 2 regimens available: basal-bolus and insulin-pump therapy. Patients with type 2 DM often require insulin, which can be combined with oral hypoglycemic agents. Regimens include basal insulin only, twice-daily premixed insulin, basal-bolus therapy, and insulin-pump therapy.
Complications Of Bariatric Surgery
Common complications following bariatric surgery are listed in Thirty-day mortality of bariatric surgical procedure is low , similar to that of laparoscopic cholecystectomy., Factors which influence the risk of complications include experience and volume of surgeries in the centre, complexity of the procedure, age and BMI of the patient, male sex, limited physical activity and associated problems such as hypertension, obstructive sleep apnoea and risk factors for pulmonary thromboembolism. Obesity surgery mortality risk score helps to predict surgical mortality risk after bariatric surgery. The variables considered are BMI > 50, male sex, hypertension, risk factors for pulmonary thromboembolism and age > 45 years. Obesity surgery mortality risk score assigns one point for each variable, so that the total score varies from 05. Higher scores are associated with increased mortality risk. The predicted mortality risks are: low-risk group A 0.2% intermediate group B 1.1% and high-risk group C 2.4%.
Recommended Reading: Number Of Grams Of Sugar Per Day For Diabetic
New Abridged Recommendations For Primary Care Providers
The American Diabetes Association has released condensed recommendations for Standards of Medical Care in Diabetes: Abridged for Primary Care Providers, highlighting recommendations most relevant to primary care. The abridged version focusses particularly on the following aspects:
-
Prediabetes
-
Diagnosis and treatment of vascular complications
-
Intensification of insulin therapy in type 2 diabetes
The recommendations can be accessed at American Diabetes Association DiabetesPro Professional Resources Online, Clinical Practice Recommendations 2015.
Type 2 diabetes care is best provided by a multidisciplinary team of health professionals with expertise in diabetes, working in collaboration with the patient and family. Management includes the following:
-
Appropriate goal setting
-
Appropriate self-monitoring of blood glucose
-
Regular monitoring for complications
-
Laboratory assessment
Ideally, blood glucose should be maintained at near-normal levels . However, focus on glucose alone does not provide adequate treatment for patients with diabetes mellitus. Treatment involves multiple goals .
Aggressive glucose lowering may not be the best strategy in all patients. Individual risk stratification is highly recommended. In patients with advanced type 2 diabetes who are at high risk for cardiovascular disease, lowering HbA1c to 6% or lower may increase the risk of cardiovascular events.
Planning A Diabetic Diet
In planning a diabetic diet, the following principles should be considered
Recommended Reading: Protein Shake For Diabetic Patients
Literature Search Strategy And Selection Criteria
The studies selected for this review were retrieved from the authorsâ personal files or identified by a computer search program using the PubMed, Scopus and Web of Science electronic databases, searching for scientific literature published in English up to July 2020. Combinations of the following search terms were applied: âcoronavirusâ, âCOVID-19â, âSARS-CoV2â, âdiabetes mellitusâ, âtype 1 diabetesâ, âtype 2 diabetesâ, âglycemic controlâ, âantidiabetic drugsâ and âcomorbiditiesâ. Additional references were retrieved from reviewing the references cited in the original articles. The final reference list was generated on the basis of relevance to the topics covered in this publication, with the aim of covering multiple aspects of the association between DM and COVID-19, and providing practical recommendations for the prevention of COVID-19 in patients with DM, and for the optimal management of hyperglycemia in patients with DM and COVID-19.
Challenges In Postpartum Management
Individuals with GDM are at increased risk of developing GDM in future pregnancies as well as an increased lifetime risk of cardiovascular disease57 and Type 2 diabetes mellitus, including by the time of the next pregnancy . In the HAPO follow-up study, 52.2% of females with GDM according to IADPSG criteria developed either a prediabetes state or Type 2 diabetes in the median 11.4 years of follow-up.58 For individuals with DIP, 59% are diagnosed with either a prediabetes state or Type 2 diabetes mellitus at the 6â8 week postpartum OGTT.59 Progression to Type 2 diabetes mellitus can be reduced by up to 50% among patients with prior GDM.60 In spite of this evidence, wide-scale systematic follow-up programmes remain underdeveloped. There are currently no evidence-based guidelines for the frequency of postpartum follow up of patients who have had GDM, though organisations such as ADIPS have released recommendations:9
- Postpartum 75 g OGTT at 6â8 weeks postpartum
- Annual 75 g OGTT if the individual is planning future pregnancy
- In those not planning pregnancy, screening via 75 g OGTT every 3 years, with increase in frequency based on clinical circumstances
- Where OGTT is not feasible, HbA1c can be used but has low sensitivity for impaired glucose tolerance
Don’t Miss: Development Of Type 2 Diabetes
Management Of Diabetes Mellitus In Hospitalized Patients
INTRODUCTION Patients with type 1 or type 2 diabetes mellitus are frequently admitted to a hospital, usually for treatment of conditions other than the diabetes . In one study, 25 percent of patients with type 1 diabetes and 30 percent with type 2 diabetes had a hospital admission during one year patients with higher values for glycated hemoglobin were at highest risk for admission . The prevalence of diabetes rises with increasing age, as does the prevalence of other diseases both factors increase the likelihood that an older person admitted to a hospital will have diabetes. The treatment of patients with diabetes who are admitted to the general medical wards of the hospital for a procedure or intercurrent illness is reviewed here. The treatment of hyperglycemia in critically ill patients, the perioperative management of diabetes, and the treatment of complications of the diabetes itself, such as diabetic ketoacidosis, are discussed separately. GOALS IN THE HOSPITAL SETTING The main goals in patients with diabetes needing hospitalization are to minimize disruption of the metabolic state, prevent adverse glycemic events , return the patient to a stable glycemic balance as quickly as possible, and ensure a smooth transition to outpatient care. These goals are not always easy to achieve. On the one hand, the stress of the acute illness tends to raise blood glucose concentrations. On the other hand, the anorexia that often aContinue reading > >
How Do I Check My Blood Glucose Level Why Is This Important
Checking your blood glucose level is important because the results help guide decisions about what to eat, your physical activity and any needed medication and insulin adjustments or additions.
The most common way to check your blood glucose level is with a blood glucose meter. With this test, you prick the side of your finger, apply the drop of blood to a test strip, insert the strip into the meter and the meter will show your glucose level at that moment in time. Your healthcare provider will tell you how often youll need to check your glucose level.
You May Like: Does Being Diabetic Make You Gain Weight
Current Management Of Type 2 Diabetes
The pharmacological management of type 2 diabetes is based on altering the effects of the ominous octet that lead to hyperglycaemia. The eight pathophysiological mechanisms include reduced insulin secretion from pancreatic cells, increased glucagon secretion from pancreatic cells, increased hepatic glucose production, neurotransmitter dysfunction and insulin resistance in the brain, increased lipolysis, increased renal glucose reabsorption, reduced incretin effect in the small intestine and reduced glucose uptake in peripheral tissues such as skeletal muscle, liver and adipose tissue. Currently available glucose-lowering therapies target one or more of these key components .
Antihyperglycaemic treatment of type 2 diabetes (based on the National Institute for Health and Care Excellence and the American Diabetes Association/European Association for the Study of Diabetes recommendation. DPP-IV, dipeptidyl-peptidase IV GLP-1, glucagon-like peptide-1 SGLT-2, sodium-glucose cotransporter-2.
Insulin formulations and delivery in the management of type 1 and type 2 diabetes