Making Lifestyle Changes Together
Nursing Interventions For Lack Of Knowledge With Rationales
| Nursing Interventions | Rationales |
| Educate the patient on the importance of not skipping a meal | Eating 3 meals a day at regular times is the best way to utilize administered insulin. Skipping a meal, especially after the administration of insulin, can lead to an unsafe drop in blood sugar level |
| Educate the patient on the components of a diabetic diet | Ideally, a diabetic diet should be low in sugar and fat, with plenty of whole grains, fruits, and vegetables |
| Assess alcohol consumption | Alcohol consumption without food can cause hypoglycemia due to a lack of glycogen release from the liver |
| Educate patient on wearing a medical alert bracelet | In case of future hypoglycemia or unconsciousness, bystanders or medical personnel should be made aware of diabetes diagnosis |
| Familiarize patient with symptoms of hypoglycemia | Knowledge and awareness of symptoms of hypoglycemia can alert the patient to impending hypoglycemia in the future |
To conclude, hypoglycemia is a common problem among diabetic patients. As a nurse, you must quickly identify and treat appropriately for hypoglycemia.
Here weve created a hypothetical case scenario for hypoglycemia and formulated a comprehensive sample nursing care plan, including nursing assessment, NANDA nursing diagnosis, desired goal, and nursing interventions with rationales.
Reference
Ackley, B., Ladwig, G., Makic, M., Martinez-Kratz, M., & Zanotti, M. . Nursing Diagnoses Handbook: An Evidence-based Guide to Planning Care . Elsevier.
Focus 1 Important Past Health Information
Just to remind you of the complexity of diabetes, hence the importance of keeping a record of your past diabetes information, lets touch on to some diabetes background.
What is diabetes?
Diabetes is a medical condition known to be chronic in other words lasting for years, if not a lifetime. In this disease, the blood sugar level increases to a higher level.
Don’t Miss: How Does Diabetes Cause Immunosuppression
Storage Conditions For Pre
In relation to the storage, stability and sterility of pre-loaded insulin syringes in the home, studies have shown these can remain stable and sterile at refrigerator temperatures for up to 28 days .
Pre-loaded insulin syringes should be stored in the main part of the refrigerator at between 2ºC and 8ºC, and should not be placed in the freezer or at the back of the refrigerator. The needle should point upwards in mixtures containing isophane insulin to prevent blockage by suspended substances in the insulin .
Lantus or Abasglar are unsuitable for use in pre-loaded syringes as it will become turbid . Tresiba and Toujeo are also not suitable and should not be drawn from the cartridge or the pre-filled pen into a syringe as it is available in different doses and can overdose the patient.
Syringes should be stored in a sealable container, and both syringes and container should be clearly labelled. If the patient is required to administer insulin more than once per day there should be a separate container for each administration time even if the doses that are utilised are the same.
Focus 3 Results Of The Objective Examinations And Test Results
If you or your loved ones diagnosed with diabetes, it is likely him/her to undergo regular checkups to monitor for common complications of diabetes closely.
Eye health
High blood glucose will result in issues like a vision that will be foggy. Then the below three problems can even occur.
- Cataracts, and
- Glaucoma.
You must conceive regular ophthalmologist visits after you have a polygenic disease . Polygenic disease diabetes is the primary reason behind vision defects in adults ages 20 to 70.
Integumentary system
Skin is prone to extreme damages by diabetes if it wasnt managed well. When dehydrated, the high blood sugar lacks the skin to be dry.
Tip: Drain your feet or use a jelly, cream, or moisturizer. Dont let the skin be on hold on with moist as it will cause fungal bacteria. Mostly they are to present in between fingers, toes, armpits, and corners of the mouth.
Tip: Skin ulcers and wounds are common among people with diabetes. Pressure-relieving heel protectors, best wound dressingsincluding negative-pressure wound therapy, all can help to speed up wound healing.
Bone and muscle function
Bone disease is a severe complexity to diabetes. Due to diabetes, the patient suffers the risk of fracture . Some factors that increase the risk of fractures include sex, body mass index, and blood glucose and diabetes medications.
Neurological function
Heart and vessel function
Heart diseases and stroke are common complications of diabetes.
Actions
You May Like: Type 2 Diabetes Can It Be Reversed
Nursing Care Plan For Diabetes Mellitus
Nursing care plan for diabetes requires the nurses to be knowledgeable and skillful.
The plan includes positive treatment for normalizing the blood glucose and lowering the complications with the help of insulin replacement, a well-planned diet, and exercise.
Further, the nurses should educate their patients about the importance of treatment and the necessity to follow the prescribed plan.
Moreover, as a nurse, you should make your patients understand the poor effect of abnormal blood glucose on their health and well-being.
The most common nursing care plans for diabetes mellitus are as follows:
- The risk for abnormal blood glucose
- Proper knowledge about the types of diabetes and their treatment
- Risk of infection
See also:Nursing Care Plan for CVA
When Should Nurses Chart Their Notes
Ideally, you make quick notations during your visit and add more depth immediately after you leave the patientâs room, when the information is fresh and top-of-mind. American Nurse Today says making brief notes while assessing the patient will help you chart faster and give more accurate nursesâ notes right after your visit. This helps you move efficiently between each patient you need to see. Visit, chart, repeat.
Read Also: Best Pills For Type 2 Diabetes
Older People With Diabetes
Some older persons with diabetes may experience poor nutritional status with physical, social and psychological factors affecting intake. Education should continue to be offered to older persons, including dietary intervention age should not restrict access. Dietetic input is key to assess nutritional status and formulate individualised care plans which take into account the changes in nutrients that are required as the body ages. Guidelines and care planning should be further adapted for those living with dementia with a focus on maintaining nutritional intake and preventing malnutrition.
Nursing Care For Diabetic Toe Ulcers: A Case Series Report And Literature Review
Volume 3, Issue 3 , September 2016, Pages 332-336 Nursing care for diabetic toe ulcers: A case series report and literature review Author links open overlay panel LiJia Jiao-jiaoBaia Open Access funded by Chinese Nursing Association This paper reports the treatment of eight cases with toe ulcers. The eight patients received nursing treatments, including debridement, dressings, decompression, anti-fungal management, and education from specialist nurses. The patients were also given drugs to control glucose, nourish the nerve, and improve blood circulation of the lower extremities. The toe ulcers of the eight diabetic patients healed after 42168 days . Thus far, few studies have focused on diabetic toe ulcers. Timely identification of risk factors and regular toe care could decrease the prevalence of toe ulcers and shorten the recovery time in patients with diabetic mellitus. Hence, these patients must be diagnosis and treated early. Results suggest that feet, particularly toes, should be inspected and cared for regularly in diabetic patients.Continue reading > >
You May Like: What Sodas Can Diabetics Drink
Nursing Interventions For Hypoglycemia With Rationales
| Nursing Interventions | |
| Educate the patient on the long-term consequences of hypoglycemia | Long-term side effects of hypoglycemia include coma, seizures, paralysis, and death |
| Educate the patient on carrying glucose tablets | Glucose tablets are a portable solution to have on hand in case of hypoglycemic emergencies |
| Perform a fall risk evaluation and enact the proper safety interventions | Dizziness and disorientation are high fall-risk factors. Interventions such as bed alarms, non-skid footwear, adequate lighting, and hourly checks, are helpful to prevent falls |
| Perform repeat neurological checks until baseline neurological status is reached | Hypoglycemia can cause severe neurological symptoms which can be permanent or fatal if blood sugar is not corrected |
Focus 8 Skin Management
On any persons skin being challenged, if body damages, it can be witnessed quite easily as diabetes progresses their cause as well.
Diabetes causes skin problems to get bad at times but can also be prevented with just a little attention. Diabetes in the past few years has commonly struck to adults, youngsters including teenagers and children. There is much medication to treat through insulin injections, non-insulin injectable, and oral drugs.
Here are the causes of fragile and vulnerable skin in diabetes.
Cause to poor skin
Symptoms of a fragile and vulnerable skin are below.
Symptoms of damaged skin
Most diabetic patients encounter complex skin conditions and disease resulting in skin wounds and ulcers.
Tip: Did you know that Hyperbaric Oxygenis proven to heal slow-healing diabetes wounds and ulcers.
Over time, your skin vulnerability can be worse in the following form.
- Wounds or cut forming on your skin
- Getting a lot of time to be healed
- Severe Irritation to the skin
- Remarkable forming change on the skin
There is a major challenge when you have skin vulnerability and unhealthy skin. That is what you will be prone to skin infections. Commonly, those infections are caused due to bacteria or fungus.
Bacterial infections
Recurrent bacterial infections are some of the serious complications that can be encountered in Type 2 Diabetes disease. These conditions cause a
redness, and
swelling.
Common types of bacterial skin infections are below.
Fungal infections
Treatments
Don’t Miss: Insulin Syringes 31 Gauge 8mm
Having A Quality Conversation About Emotional Health And Diabetes
Its important to ask people about their emotional health at every appointment. Just because everything may seem okay the first time you ask, this can change over time. Dont think of this as an added extra. If someone is struggling emotionally, theyre going to find looking after their diabetes much more difficult
When To Seek Help
Hypoglycemia is the most common emergency requiring the nurse to intervene and consult healthcare team members. If, upon assessment, the nurse finds a patient with diabetes who has signs and symptoms of hypoglycemia , the nurse should assess for additional clinical manifestations of hypoglycemia such as cool, clammy skin and perform blood glucose testing. Most in-patient clinical facilities provide automatically generated treatment protocols for hypoglycemia. These protocols might include providing orange juice for conscious patients with the ability to swallow. Otherwise, if the patient is lethargic and providing oral intake would pose an aspiration risk, the protocol might include intravenous administration of dextrose 50% or a glucagon injection followed by retesting the blood glucose in 10 to 15 minutes and notifying the healthcare provider so that the patients medication regimen can be adjusted appropriately. Another emergency in patients with diabetes is extreme hyperglycemia. If the patient with diabetes is experiencing tachypnea and extreme hyperglycemia , the nurse should notify the healthcare provider immediately. Anticipated orders might include transferring the patient to an intensive care unit, administering insulin intravenously, administering potassium intravenously, and infusing intravenous fluids. Additionally, the nurse should seek help from the respiratory therapist who might obtain blood sampling for arterial blood gases.
Also Check: Type 2 Diabetes After Kidney Transplant
When How And Who
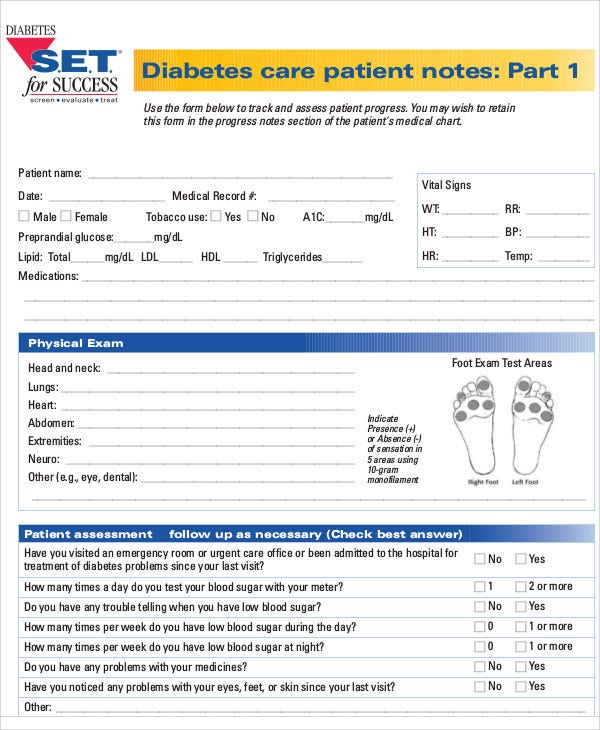
Patients with diabetes frequently attend their healthcare practitioners, either specifically for diabetes-related issues, for complications of their chronic illness, or for unrelated problems. They may see their GP, practice nurse, hospital diabetologist, diabetes specialist nurse, dietician and many others, from time to time. Each visit can be viewed as an opportunity to assess and improve the patient’s understanding of their illness, and their ability to control the disease.
This article provides a summary of the areas of assessment relevant to type 1 diabetes and type 2 diabetes, which will need to be adapted, depending on an individual patient’s type of diabetes.
The Fundamentals Of Nursing Care Plan For Type 2 Diabetes The Checklist
This Nursing Care Plan is based on 10 key focus areas when managing type 2 diabetes from home.
They are:
Focus 1 Important Past Health Information
Focus 2 Your Lifestyle
Focus 3 Results of the Objective Examinations and Test Results
Focus 4 Diabetes Monitoring
Focus 6 Your Endurance
Focus 7 Symptoms and Complications Management
Focus 8 Skin Management
Focus 9 Healthy Immunity for Infection Control
Focus 10 Positive Health Beliefs and Psychology
Lets explore each focus area of the Care Plan to understand them better, especially the key actions under each.
Also Check: How Do Diabetics Check Their Blood Sugar
How To Write Nursing Notes
A nursing note is a medical or health record that is made by a nurse that shows accurate documentation of nursing assessments, changes in patients conditions, care provided, and related information to support the clinical team to deliver excellent care.
Keeping a detailed and accurate note is essential for having efficient communication between the medical staff and nurses. The nursing note serves as a proof of record between the medical staff and nurses to show the progress achieved in a patient and guide whoever takes off after the previous working staff of a day. Apart from record purposes, the legal team uses the note or chart in case of any lawsuit or malpractice to show what was last noticed in the patient and what was the last action taken to treat him or her.
Nursing notes would help a nurse recall the nature of the events and care provided and the doctors involved if she is called as a witness or sued.
Risk For Unstable Blood Glucose Levels
If a womans insulin production is insufficient, glucose cannot be used by the body cells. The cells register the need for glucose, and the liver quickly converts stored glycogen to glucose to increase the serum glucose level. However, because insulin is unavailable, the body cells still cannot use the glucose, so the serum glucose levels rise.
Nursing Diagnosis
- Risk for Unstable Blood Glucose Levels
Risk factors may include
- Increased resistance of cells to insulin
- Increased insulin breakdown
- A risk diagnosis is not evidenced by signs and symptoms. Interventions are directed at prevention.
Desired Outcomes
- Within 4 hours of nursing intervention, the patient will verbalize understanding of the individual treatment regiment and the need for regular glucose self-monitoring.
- Within 8 hours of nursing action, the patient will maintain fasting serum blood glucose levels between 60-100 mg/dl and 1-hour postprandial of no higher than 140 mg/dl and will be free of signs and symptoms of diabetic ketoacidosis .
Nursing Assessment and Rationales
2. Note signs of hyperglycemia or hypoglycemia .Observing these signs may alert the nurse to developing hyperglycemia or hypoglycemia. If the woman cannot increase her insulin production, she will have periods of hyperglycemia as glucose accumulates in the blood. Because the fetus continuously draws glucose from the mother, maternal hypoglycemia can occur between meals and night.
Nursing Interventions and Rationales
You May Like: Foam Dressing For Diabetic Foot Ulcer
Risk For Unstable Blood Glucose Level Nursing Care Plan
Use this nursing diagnosis guide to help you create a Risk for Unstable Blood Glucose Level nursing care plan.
There are different kinds of sugars. Glucose is what our body utilizes most. Other sugars we eat, like fructose from fruit or lactose from milk, are converted into glucose in our bodies and use them for energy. Our bodies also break down starches, which are sugars stuck together, into glucose. Serum glucose is transported from the intestines or liver to body cells via the bloodstream and is made available for cell absorption via the hormone insulin, produced by the body primarily in the pancreas. Insulin is secreted by the beta cells of the islets of Langerhans in the pancreas in response to elevated level of blood glucose. This pancreatic hormone facilitates the movement of glucose across the cell membranes to be used for metabolic activity. The alpha cells of the islets of Langerhans secrete glucagon when blood glucose levels are low.
Hyperglycemia or elevated blood glucose levels may occur in a variety of clinical situations. Diabetes mellitus is the most common disorder associated with elevated blood glucose levels. Certain drugs have hyperglycemia as a side effect.
An important part of managing blood glucose levels, as well as the overall health of a person, is maintaining a healthy weight through a healthy diet and exercise plan.
| Excessive alcohol consumption, without food intake, blocks release of glycogen from the liver, causing hypoglycemia. |