Diagnosing A Diabetic Ulcer
An accurate diagnosis of a diabetic ulcer must be given by a medical health professional. Most doctors will first provide a physical examination of the patients foot. Should further tests be required, a doctor may recommend an X-ray or an MRI scan.
An X-ray can show any changes in foot alignment through a system of imaging. An X-ray image can show loss of bone mass and hormonal imbalances that can potentially relate to the diagnosis of diabetes.
MRI scans use three-dimensional images of the bodys soft tissue. If the extent of damage needs to be assessed, an MRI scan can use magnetic radio waves to reveal possible inflammation. This test can expose any significant infections in the foot.
One of the simplest tests a physician can use to diagnose an infectious diabetic ulcer is the blood test. This test is usually done by drawing blood at a doctors office so that the results can be sent to a lab for further information.
What If A Leg Ulcer Does Not Heal Properly
If you have a wound or sore that is not healing properly, schedule an appointment with your primary care physician as it may develop into or be the start of a leg ulcer. You may be scheduled to see a nurse rather than a doctor, since nurses are often responsible for the care of patients with leg issues.
How Do Diabetic Foot Ulcers Form
Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation , and trauma, as well as duration of diabetes. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by elevated blood glucose levels over time. The nerve damage often can occur without pain and one may not even be aware of the problem. Your podiatric physician can test feet for neuropathy with a simple and painless tool called a monofilament.
Vascular disease can complicate a foot ulcer, reducing the bodys ability to heal and increasing the risk for an infection. Elevations in blood glucose can reduce the bodys ability to fight off a potential infection and also retard healing.
Recommended Reading: I Need Help With My Diabetes
Risk Of Bias Within Studies
The quality assessment scores obtained ranged between four and six, indicating moderate methodological quality of included studies. As it is not possible to blind both the participant and treating therapist, studies in this review were not able to achieve a score greater than eight out of ten on the PEDro scale. The PEDro scale scoring of the included studies is shown in Fig. .
Fig. 2
How Can I Prevent Diabetic Foot Ulcers
Diabetic foot ulcers are the most common reason for hospital stays among people with diabetes.
Whats the reason? People with diabetes, not only do they not heal non-diabetics, but in addition to that, they develop a disease called diabetic neuropathy, where they lose feeling in their feet, says Arti Masturzo MD, medical director at the Bethesda North Wound Care Center.
However, with the proper precautions, Dr. Masturzo says diabetic foot ulcers can be avoided.
Read Also: Pain Medicine For Diabetic Neuropathy
Nonsurgical Treatment For Diabetic Foot Ulcers
To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
Difference #: Scientifically Proven To Work
EMUAID® First Aid Ointment is proven to have 99% efficacy approval rating.
EMUAID® First Aid Ointment is recommended both by physicians and customers worldwide. Additionally, EMUAID® First Aid Ointment is non-steroidal, has NO reported side effects, and does not conflict with other medications.
In a Time Kill Study conducted by a third party, independent laboratory, test results proved that EMUAID® kills Bacteria, Yeast and Mold on contact and eliminates 99.99% of bacteria in less than 1 minute.1
Read Also: How Close Are We To Curing Diabetes
Preventing & Curing Diabetic Ulcers With Wellstar Wound Care
When someone is diabetic, a small wound can escalate into a major health issue and, in many cases, lead to an amputation. However, with proper and accelerated healing with , Wellstar patients are partnering with providers to treat wounds like diabetic foot ulcers.
Diabetic foot ulcers can develop if is not well-managed, and some causes of ulcers include poor circulation and high blood sugar. Ulcers may go unnoticed at first because many people with diabetes are also affected by and do not have feeling in their feet, said , Medical Director of the Wound Care and Hyperbaric Medicine Department at .
Also, if a diabetic person gets a wound, it may not heal as quickly, as people with diabetes are more likely to also experience poor circulation, immune system deficiencies and elevated blood sugar levels.
When you combine the lack of sensation in the foot with the lack of healing, that leads to even more damage, Dr. Duran said.
Foot ulcers should be taken seriously when a diabetic person has an open wound, their five-year mortality rate increases by about 32%, according to Dr. Duran.
When You Need More Treatment
If your wound doesnât heal in about a month or becomes an infection that spreads to the bone, you may need other treatments. These can include surgery and hyperbolic oxygen therapy, which involves breathing pure oxygen in a special room in order to help your body heal.
If your ulcer develops gangrene and your tissue dies, your doctor may have to amputate that area of your body.
Also Check: How Do You Know Have Diabetes
What Causes Diabetic Sores
Diabetic sores are open wounds that often affect the feet and legs but can also form in other areas such as the hands or folds of the skin on the abdomen.
One of the main causes of diabetic sores is high blood sugar levels, which can damage the nerves and blood vessels over time and restrict blood flow, especially to the limbs. This makes it harder for wounds to heal.
Diabetes makes a person more likely to develop ulcers or sores because of the following:
- Neuropathy: Nerve damage reduces the sensation in the feet, making them insensitive to minor cuts or injuries.
- Poor blood circulation: Poor blood flow makes it harder for even minor wounds to heal. Diabetes is also linked to a condition called peripheral arterial disease, which reduces blood flow to the legs and feet.
- Reduced immune function: The immune system is responsible for fighting off and stopping infections, but in people with diabetes, the immune system is less effective.
Even minor wounds or small cuts can turn into serious foot ulcers if not treated properly.
What Causes Diabetic Foot Ulcer
People with diabetes have an increased chance of developing foot ulcers because you are more likely than other people to damage the skin on your feet. This is because diabetes can cause nerve damage, so you donât notice if your foot is injured or sore. Diabetes also causes blood vessel damage so your skin canât heal easily.
You May Like: Sample Meal Plan For Ulcerative Colitis
Recommended Reading: Is Sardines Good For Diabetics
New Treatment Using Pure Oxygen Therapy That Is Applied At Home Appears Effective In Speeding Up Healing Of Diabetic
with Robert G. Frykberg, DPM, David Armstrong, DPM, MD, PhD, and Mike Griffiths, DProf
If you have diabetes, developing a foot ulcer can be seriousdeadly serious. These open sores occur in about 15 percent of those with diabetes, and most often appear on the bottom of the foot. About half of all people who experience a foot ulcer will land in the hospital due to either an infection or another complication related to the foot ulcer.1
Of course, this open, slow-to-heal wound is likely to restrict your mobility and make life pretty unbearable and depressing, especially if, as is common, an infection sets in, or is worsened by poor circulation. And, the standard treatments, ranging from compression stockings to are not sufficiently effective.
Now, there may be a home-based method of oxygen therapy that is reported to helpboth to heal the ulcers faster than usual care and to help keep them from recurring.2.
“This approach delivers pure oxygen directly to the surface of the wound,” says Robert G. Frykberg, DPM, the study’s lead author and an adjunct professor at Midwestern University in Glendale, Arizona. The best aspect of this new treatment is that it can be done by the patient at home, which is a huge bonus, he tells EndocrineWeb.
Insurance Coverage For Pure Oxygen Treatment Is Limited But Expanding

The Food and Drug Administration considers the oxygen delivery product, a class II medical device, to which it granted premarketing clearance in 2009.
The therapy is available now in limited areas of the country but the company is working to gain broader availability, says Mike Griffiths, DProf, CEO and medical director of AOTI Inc. based in Oceanside, California, and Galway, Ireland.
This therapy is now prescribed in Veterans Administration facilities, he says, and ”we have approval for New York State Medicaid reimbursement.” He declined to provide the cost to a patient who doesnt have insurance coverage, but he says the new study results is expected to help the company get broader healthcare coverage from Medicare and other insurers soon.
Read Also: Grams Of Sugar Per Day For Diabetic
Treatment Still Requires Regular And Ongoing Foot Self
The best treatment for a foot ulcer, according to the American Podiatric Medical Association, ”is to prevent its development in the first place.” To prevent diabetes-related foot wounds from occurrng, you should have your feet checked at least annually, and more often if you have poor circulation or other symptoms.
Besides seeing your endocrinologist or a podiatrist regularly, you can reduce your risk by assessing your time-in-range and making adjusting to improve your blood sugar control, quiting if you are still smoking, and taking the necessary steps to achieve good blood cholesterol levels.
Ask your podiatrist about the best shoes to wear and how best to inspect your feet to spot problems early.
Dr. Armstrong has no relevant disclosures. Dr. Frykberg received AOTI research funds to conduct the study and has received speaking honoraria. The study was sponsored by AOTI, Inc. which makes the device.
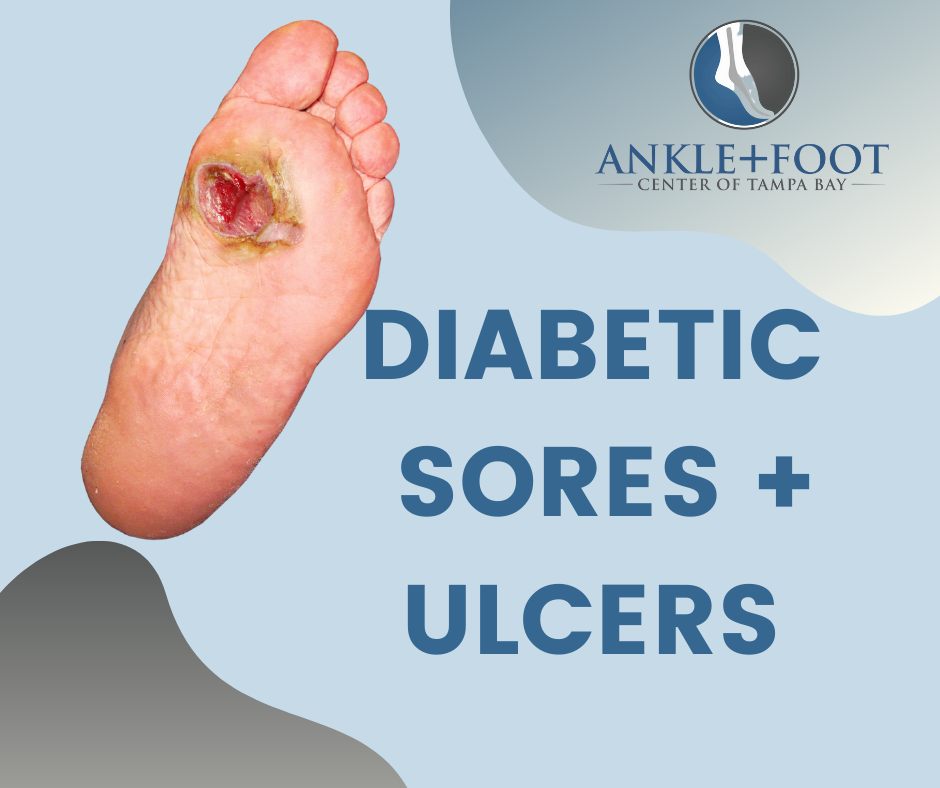
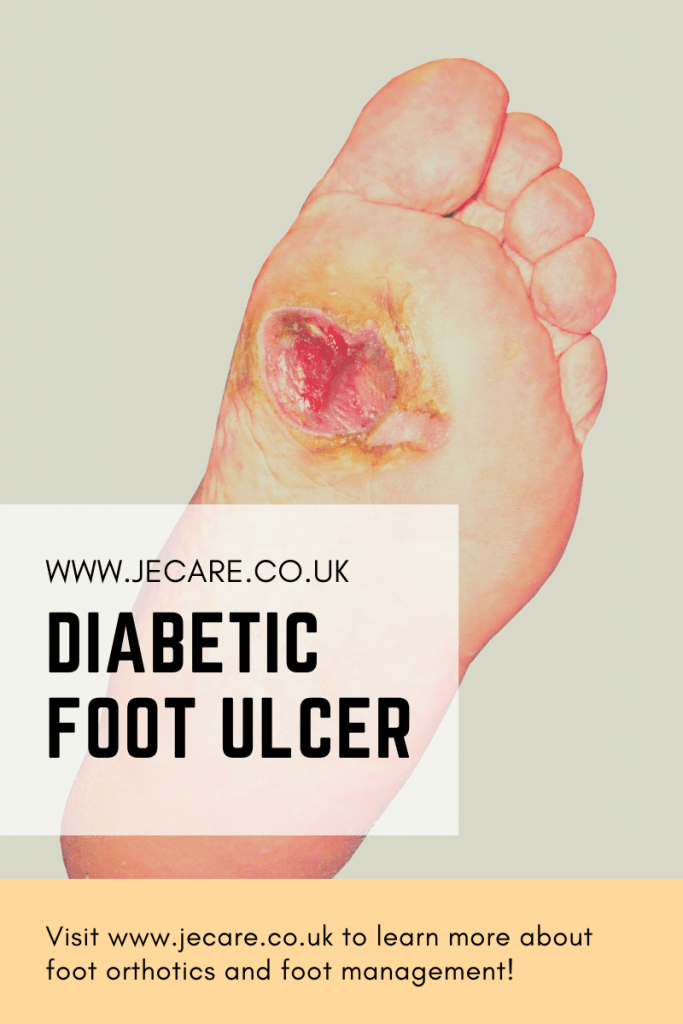
What Is A Diabetic Ulcer
A neurogenic ulcer is also known as a diabetic ulcer. Diabetic ulcers are generally found on the bottom of the foot and can occur on either or both feet. Other areas that can be affected include the legs, hands, and even in the folds of skin, around or on the stomach. Diabetic ulcers can be painful. Many people feel embarrassed by their appearance, in addition to the physical pain they experience.
A typical diabetic ulcer on the foot looks like a red sore that manifests in the surface of the skin and can form in a variety of areas. However, sores can occur deeper in the skin. A deep foot ulcer can extend to the tendons and bones of the feet and must be treated quickly. If the condition worsens, the diabetic ulcer will likely become infected.
Read Also: Diabetes High And Low Symptoms
What Does A Fungal Infection In The Groin Look Like
What are the signs of a fungal infection of the groin? Typically, the groin area gets itchier and somewhat painful, particularly in the crease between the top of the leg and the genitals. It is more prevalent in males, and the scrotum may be itchy as well. In the groin, a red, somewhat scaly skin forms, generally with a distinct edge or boundary.
How Emuaid Works To Eliminate Your Diabetic Ulcer Symptoms
You May Like: How Much Sugar Can A Diabetic Have In One Day
Bread And Baking Soda
I have a new leg uler which developed after a bleed. It is on my interior ankle. Extremely painful. Can feel the swelling where the damage was done. I was told of a method using bread, bicarbonate of soda on the bread and water which makes the paste bubble. Does anyone know of this method. Surelly there is some native bush remedy out there. Indigenous people have cures for all their needs which they have used for years. Modern wound clinics just put on a bandage and say see you nexst week. One year later you are still doing the same thing.
Some years ago I was given a radical idea to try. At the time I didn’t take any notes etc but it worked! I had 5 cellulitis ulcers on one leg and I was told to drink 1/4 cup of Colloidal Silver every 5 hours and spray my leg frequently with same. To do it over a 24 hour period. I did it and within 10 days I had only had the original ulcer left. Which hasn’t been oozy for years.
So in that time frame, I lost 4 ulcers that have never returned. In 2017, one of my 2 specialists told me to use potassium permanganate to wash my legs daily and use the amount of crystals that would barely fit on the edge of a matchstick… He told me it kills sepsis and pseudomonas. Other Dr was delighted and told me that before the arrival of penicillin, doctors used Condy’s Crystals as a wash for ulcers.
HoneyHoney
What Is The Finest Cream For Leg Ulcers
Additionally, creams containing urea may be beneficial, since urea is a good moisturizer. Around a leg ulcer, the skin may get macerated and damaged, particularly if the lesion is actively oozing. A barrier film, such as Cavilon barrier film or LBF , protects and assists in the healing of the peri-wound skin.
Don’t Miss: Type 2 Diabetes Nerve Damage
Management Of Systemic And Local Factors
Treatment of diabetic foot ulcers requires management of a number of systemic and local factors.
Precise diabetic control is, of course, vital, not only in achieving resolution of the current wound, but also in minimizing the risk of recurrence. Management of contributing systemic factors, such as hypertension, hyperlipidemia, atherosclerotic heart disease, obesity, or renal insufficiency, is crucial. Management of arterial insufficiency, treatment of infection with appropriate antibiotics, offloading the area of the ulcer, and wound care are also essential.
References
Amin N, Doupis J. Diabetic foot disease: From the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016 Apr 10. 7 :153-64. . .
Naves CC. The Diabetic Foot: A Historical Overview and Gaps in Current Treatment. Adv Wound Care . 2016 May 1. 5 :191-197. . .
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for Medicare and private insurers. Diabetes Care. 2014. 37 :651-8. .
Gentile AT, Berman SS, Reinke KR, Demas CP, Ihnat DH, Hughes JD, et al. A regional pedal ischemia scoring system for decision analysis in patients with heel ulceration. Am J Surg. 1998 Aug. 176:109-14. .
Mills JL Sr, Conte MS, Armstrong DG, et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection . J Vasc Surg. 2014 Jan. 59 :220-34.e1-2. . .
What Type Of Healthcare Provider Helps With Ulcers How Do They Diagnose An Ulcer
Your healthcare provider can tell what type of ulcer you have based on four observations:
- Appearance of the ulcer.
- Appearance of the borders.
- Appearance of the surrounding skin.
Your primary healthcare provider can diagnose an ulcer, but they may send you to a specialist for treatment. You may see a podiatrist, a provider who works with feet, or a wound specialist. To find out how deep the ulcer goes, and to see if it caused an infection in a nearby bone, they may order an X-ray, MRI or CT scan.
For more complicated cases that require surgery, you may also see a plastic surgeon, anesthesiologist, orthopedic surgeon and/or vascular surgeon.
You May Like: Sourdough Bread Good For Diabetics
The Closest Choice To Native Amniotic Membrane
Never dehydrated or frozen, Affinity uses a gentle hypothermic* storage method called AlloFresh that preserves the product in its fresh state. In analytical testing, Affinity has been shown to retain its native tissue characteristics1,2:
Viable cellsincluding epithelial cells and fibroblasts1,3
Growth factors/cytokinesanalytical testing has shown that the level of these factors is similar to unprocessed amniotic membrane1,4
Native extracellular matrix structurewith multiple ECM proteins that are important for scaffolding, including collagen types I, III, V, VI, and hyaluronic acid1,3,5
The spongy layeran abundant source of proteoglycans, glycoproteins, and hyaluronic acid1,6
*Affinity should be maintained at refrigerated temperature .
How To Prevent Diabetic Foot Ulcers
The first line of defense in preventing diabetic wounds is to follow the guidelines recommended to keep the disease itself under control:
- Maintain healthy blood sugar levels through a healthy diet and by taking medications as instructed by your doctor.
- Keep your blood pressure within a healthy range.
- Avoid alcohol and tobacco.
You should also take measures to avoid causing sores or wounds on the feet:
- Never walk barefoot.
- Wear shoes that fit properly and dont rub the skin.
- Wash your feet daily with mild soap and lukewarm water to prevent the buildup of bacteria on the skin, which can cause infection even in the tiniest skin breaks.
Because a loss of sensation in the feet may mean theres no pain felt even when an ulcer is present, its also extremely important for those with diabetes to regularly check for any foot sores or skin irritation. This way, the ulcer can be properly treated as early as possible.
Don’t Miss: Are Ketones Safe For Diabetics