Good Insulin Pump Habits
It may take several months to get comfortable with the insulin pump. During those first months is the time to adopt some good habits. Here are some tips to help you adjust:
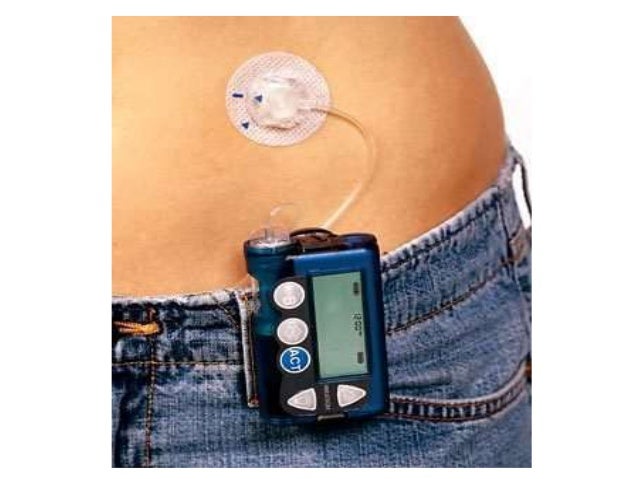
Places to wear the insulin pump
Some people are comfortable with wearing the insulin pump on their belt. The pump may come with a leather carry case or clip, which holds the device and gives the appearance of a pager or small mobile phone.
Others simply carry the pump in a pocket. Some women prefer to wear the pump in their bra or attached to a garter on the leg. Each of the pump suppliers has accessories and there are now also many websites selling pump accessories.
The cannula, which is inserted under the skin, is often placed in the abdominal area but can also be placed in the upper buttock, upper and outer thigh, hip or upper arm.
Swimming
Swimming is a very healthy activity for people with diabetes including those using a pump. Some pumps are waterproof and tested to an international standard while others are watertight. This means it is possible to swim, shower and surf without taking your pump off if you so choose. If you participate regularly in water sports it is advisable to check the individual product specifications regarding waterproof status before choosing your pump.
Sleeping
One of the questions most commonly asked about pump therapy is Where do I put the pump when I go to sleep?
Some common places people leave their pumps are:
Exercise
Pregnancy
Sick days
School
Travel
Managing Patients With Type 1 Diabetes On An Insulin Pump
This section is meant to provide general information and guidelines on the management of patients using insulin pumps and should not replace care from or consultation with diabetes care providers who are experts in insulin pump therapy. Ideally, the patient is managed by a diabetes care team and is seen regularly by members of that team.
Upon initiation of insulin pump therapy, it is recommended that patients have face-to-face follow-up with their diabetes care providers within the first 3-14 days after starting.
As with patients on MDI, insulin doses for patients on insulin pumps should be adjusted regularly. Adjustments are made whenever BG patterns indicate a need. Typically, a pattern is established over a period of several days before changes are made, thus minimizing the potential for chasing BG levels. Once a change is made, the effectiveness of this change should be determined over several more days. The need for constant adjustments to meet the needs of the growing child and adolescent is the hallmark of insulin treatment in pediatrics.
Adjusting Basal Rates
Adjusting Meal Boluses
-
Test the 2-hour postprandial BG level to eval/uate effectiveness of meal bolus
-
2 hours after meal target of < 160-180 mg/dL
Consider accuracy in carb counting as one cause for bolus ineffectiveness
Increase ratio to decrease amount of insulin given with bolus
Adjustments typically made in 10%-20% increments
Adjusting Correction Boluses
Managing Hypoglycemia
Causes
Treatment
Causes
Pump Site Failures Stress Me Out
I find it really stressful how quickly you can develop moderate ketones or simply blood sugars over 300 mg/dL just because a pump site failed or theres a kink in the cannula.
Using long-acting insulin for my background/basal insulin needs means I never have to worry about thisever. Sure, there are other reasons, like a terrible stomach virus or extreme stress, that can lead to ketones or an huge unexpected spike in my blood sugar, but those are rare.
With an insulin pump, site failures are par for the course. Theyre expected. Theyre one of the things you simply have to deal with in order to get other benefits of pumping.
As a mother of two, I also find it extremely stressful to be worrying about a 300 mg/dL because the insulin isnt getting through a new infusion site properly than simply taking my insulin via MDI and knowing without a doubt that Im getting what I need.
I dont want to deal with site failures. Id take the stressors of MDI over pump site failures any day, all day.
Recommended Reading: Diabetes Type 1 Treatment Without Insulin
Diabetes Insulin Pump Features To Consider
Calculating insulin
Insulin pumps calculate the amount of insulin required to cover the carbohydrate eaten . Insulin pumps also calculate the insulin dose required to correct any high blood glucose level that you enter in the insulin pump that is outside your target range.
Tracking active insulin
Insulin pumps have a feature that prevents you from stacking or giving too much insulin. When you enter your blood glucose level and carbohydrate intake, the pump will calculate the dose required after considering the insulin still active or on board from a previous bolus. This may assist with avoiding hypos.
Bolus types
Insulin pumps can be programmed to deliver a meal bolus in different ways. A meal bolus may be delivered, for example, over a period of two hours rather than all at once. These different bolus types can make eating a variety of foods and eating out much easier.
Insulin delivery
Pumps vary in the increments of the basal rate and bolus dose that can be delivered. If you have a very small total daily dose of insulin or are very insulin sensitive then small delivery doses will be important.
Insulin reservoir/cartridge size
The reservoir/cartridge size varies between pumps, so depending on your daily dose of insulin some pumps will be more suitable than others.
Infusion sets
Insertion devices
Computer software
Food database
Water resistance
Continuous glucose monitoring systems
Insulin pump cost
Who pays?
Reasons People Ditch The Pump

Integrated Diabetes Services provides detailed advice and coaching on diabetes management from certified diabetes educators and dieticians. Insulin Nation hosts a regular Q& A column from IDS that answers questions submitted from the Type 1 diabetes community.
Q I see studies show that people with Type 1 do better on insulin pump therapy, but I sometimes hear of people stopping pump therapy to return to multiple daily injections. Can you tell me why it might be better for some people to stop using a pump?
A There are many more choices for insulin pumps than in the past, and many of these new pumps come with new and powerful technological options to help you with blood sugar management. Many clinicians promote pump use as the best way to achieve optimal control.
But is it really the end-all-be-all of diabetes management? As with everything in life, it comes down to personal choice and what works for you. Its best to do your homework to evaluate if a pump is best for your lifestyle and blood sugar management needs.
There are plenty of articles discussing the pros of pump therapy, but few that discuss the cons. To offer some balance, here are some downsides to pump use that have caused people to switch back to multiple daily injections:
Thanks for reading this Insulin Nation article. Want more Type 1 news? .
Have Type 2 diabetes or know someone who does? TryType 2 Nation, our sister publication.
Don’t Miss: Best Essential Oils For Diabetes
Potential Benefits Of Pump Therapy
The expected benefits of insulin pump therapy are summarized in . Insulin pump use provides a near-physiologic basal-bolus insulin delivery method that, in theory, mimics normal pancreatic function better than injections . Precise insulin dosages can be programmed and administered, giving the patient increased flexibility in daily living with regard to mealtimes, travel, work schedule, etc. . Observational studies, meta-analyses, and randomized clinical trials have demonstrated improvements in long-term glycemic control when compared with daily multiple-dose insulin injections . Evidence from clinical studies suggests that pump therapy is associated with a decreased risk of severe hypoglycemia and the need for emergent medical care . The latter translates into reduction in the cost of care and utilization of health care resources . Quality of life measures have shown improvement with pump therapy compared with MDII .
Disadvantages Of Using A Pump With Type 2 Diabetes
People with Type 2 diabetes often prefer insulin pumps because of the flexibility that the treatment provides and the freedom from injections. We cant forget that every person with diabetes has specific requirements and that is why its important to choose, along with healthcare professionals, the best possible treatment plan for each individual.
You May Like: Diabetic Coma Is A Condition That Occurs When
Who Should Use A Pump
Insulin pumps have been used successfully across the age spectrum. Whether or not to use a pump is a personal decision. You can manage your diabetes equally well with pumps or multiple injections, so it comes down to your preference.
Choosing one method over the other is not a lifelong commitment. Some people go on and off their pumps . Remember that a pump is just a toolyou can reach blood glucose goals with a pump or injections. But here are some things to consider
Travelling With An Insulin Pump
While travelling, an accompanying letter on practice letterhead should be provided stating the medical history of the patient, including the diagnosis of type 1 diabetes, and that management is via an insulin pump. A list of current drugs, with generic names and doses, should be included. The letter should stress that it is important that the patients drugs accompany them, and that the insulin pump should not be disconnected. In particular, the pump should not be put through airport X-ray machines.
Prescriptions should be obtained for insulin and other drugs before travel. In case of pump failure both rapid-acting and long-acting insulin should be obtained along with injecting devices and needles. Sufficient equipment for glucose testing should be packed in the hand luggage. In addition to drugs and glucose-testing equipment adequate quantities of consumables should be packed. As a rule, pack twice as many sets as potentially required for the planned period away from home. An adequate supply of consumables should be included in the hand luggage while flying.
Recommended Reading: Diabetes And Metabolism Patient Portal
Changing Infusion Sites And Refilling The Pump
Once set up, changing infusion sites and refilling the pump with insulin are two common tasks you will regularly need to perform to keep yourself pumping.
Infusion sites need to be changed every few days to allow consistent delivery of insulin. Changing of infusion sites means taking out old infusion set and replacing it with a new infusion set.
A change of infusion site can take a few minutes and a bit of space to get organised but as you only need change the site every 2 to 3 days, it is usually easy enough to find a convenient time and place to do this.
When the pump begins running out of insulin, new insulin will need to be loaded into the pump, either by cartridge or by refilling the reservoir from an insulin vial .
What Happens While Using An Insulin Pump
An insulin pump delivers insulin in one of two ways:
- Small, continuous insulin doses .
- Surges of insulin near mealtimes .
While using an insulin pump, you still need to check your blood sugar levels. Most people check blood sugar at least four times a day. Or you may use a continuous glucose monitor.
The pump uses information you enter about your food intake and blood sugar levels to calculate how much bolus insulin you need. The pump then recommends a bolus dose to you and waits for your approval before delivering. In addition, some pumps automatically adjust basal doses based on glucose levels from a continuous glucose monitor.
Also Check: Who Do You Know If You Have Diabetes
Case 6benefits Of The Insulin Pump In Patients With Type 2 Diabetes And Insulin Resistance
RW is a 47-year-old Hispanic male who has had type 2 diabetes for 16 years. He is morbidly obese with a body-mass index of 43. Both of his parents and two of his three siblings suffer from diabetes. He is taking metformin and multiple-dose insulin injections. He has tried incretin-based therapies in the past for their glucose-lowering and weight-stabilizing benefits but could not tolerate the gastrointestinal side-effects. The patients daily insulin dose has been progressively increased to a regimen of glargine 115 units twice a day and aspart 4560 units prior to each meal. He prefers to use disposable insulin pens for convenience however, individual pens only hold 300 units and do not last more than two days each. Efforts at lifestyle changes aimed at weight loss have been marginally successful. His A1c level varies between 7.9% and 8.6%. He is motivated to improve his health and checks his fingerstick glucose readings several times a day.
Question:
Considering his high insulin requirements and burden of multiple daily insulin injections, what management options could be presented to him?
The Diabetes Gear Load
Speaking of airports, you cant travel light with diabetes. All insulin-using PWDs should be carrying gear for checking or monitoring blood sugar, some fast-acting glucose, a glucagon kit, and a medical alert of some sort. But, as youll see, pumpers need to carry more.
While shot-wielding PWDs can get away with limiting their load to either extra syringes or pen needles, and perhaps a cooling system for the insulin itself, pumpers need spare infusion sets, spare cartridges, spare batteries or a charging cord, and perhaps skin prep products to sterilize the skin and help the sets to stick.
As a pumper, you wont feel quite like a Marine will a full combat pack hitting the beach, but its close.
Recommended Reading: What Is A Good Morning Blood Sugar For A Diabetic
Why Use An Insulin Pump For Diabetes
Some health care providers prefer the insulin pump for diabetes because its slow release of insulin mimics how a normally working pancreas would release insulin. Research studies have shown that the insulin pump is a safe and valuable treatment option for those with poorly controlled blood sugar.
Another advantage of the insulin pump is that it frees you from having to measure insulin into a syringe.
Show Sources
How Insulin Pumps Work
Insulin pumps are worn externally and deliver a continuous amount of fast-acting insulin 24 hours a day.
There are three main components to insulin pump therapy:
- a pump , which pumps the insulin into your body
- a reservoir or a cartridge, where insulin is held
- an infusion set, which includes a thin tube that runs from the reservoir in the pump to the infusion site on your body, and a short cannula that is inserted under your skin
The main steps to using the pump include placing the insulin-filled reservoir inside the pump, and inserting the cannula under your skin using a needle. The cannula is held in place with an adhesive patch for 24 to 72 hours, after which time it should be replaced. A tube connects the cannula to the reservoir in the pump and delivers a set amount of insulin into your body.
Two types of insulin doses are delivered to your body by the pump:
- Basal insulin doses are delivered continuously over 24 hours and keep your blood sugar levels stable between meals and overnight.
- Bolus insulin doses are delivered when you push a button on the pump – you can use them when you eat to correct high blood sugar levels.
The pump can be worn in many places on your body. It can be attached to your waistband, pocket, bra, armband, or underwear. When you sleep, you can lay it next to you on your bed or nightstand. You can disconnect the pump for activities such as swimming or showering. Insulin pumps that are not waterproof should not be exposed to water.
Also Check: What Is An Insulin Pump
How To Get An Insulin Pump
To get a pump for free, youll have to meet certain criteria set by the National Institute for Health and Care Excellence .
If you live in England and Wales, youre over 12 years old and have type 1 diabetes, you need to meet one or more of the following criteria:
- You cant get to your target HbA1c without severe hypos.
- Your HbA1c remains high despite carefully trying to manage your diabetes.
If you live in Scotland or Northern Ireland, the criteria is different. Your healthcare team will give you advice on whether you meet your local criteria for getting a pump and what the next steps are.
If youre thinking about an insulin pump for your child, the criteria is different. Pumps are recommended for children under 12 when multiple daily insulin injections arent practical or appropriate. Make sure you speak to your diabetes specialist about if this is the best option for your child.
We understand that trying to get an insulin pump can be very frustrating, and you might feel disappointed if you cant get one. If you have any questions at all, or you just need someone to talk to, call our helpline.
Pumps are currently not available for people with Type 2 on prescription. You can self-fund, but make sure you have a discussion with your healthcare professional if youre thinking of trying one.