What Is Type 2 Diabetes
Type 2 diabetes, the most common type of diabetes, is a disease that occurs when your blood glucose, also called blood sugar, is too high. Blood glucose is your main source of energy and comes mainly from the food you eat. Insulin, a hormone made by the pancreas, helps glucose get into your cells to be used for energy. In type 2 diabetes, your body doesnt make enough insulin or doesnt use insulin well. Too much glucose then stays in your blood, and not enough reaches your cells.
The good news is that you can take steps to prevent or delay the development of type 2 diabetes.
How Does The Possible New Implication Affect Current Day Treatment
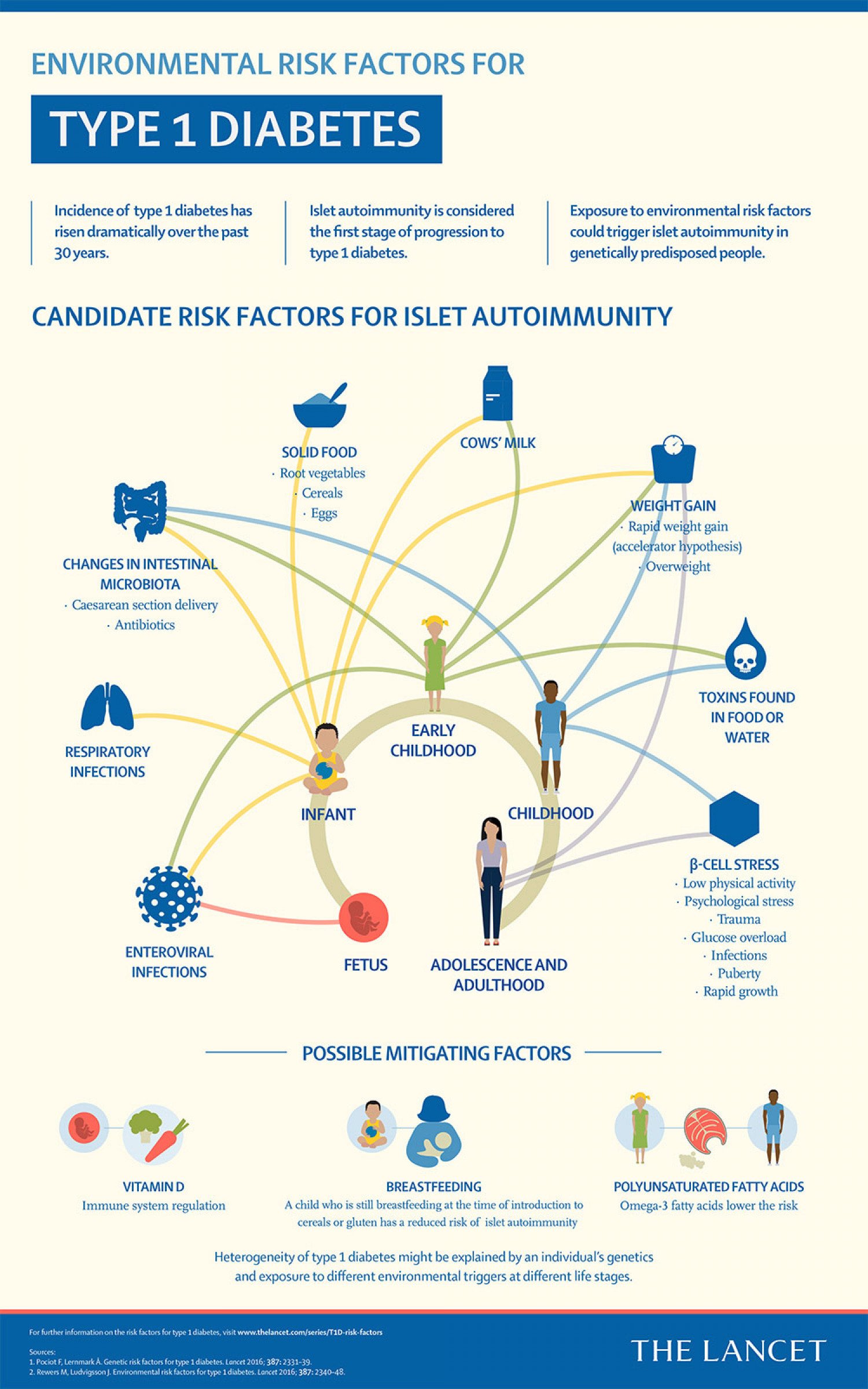
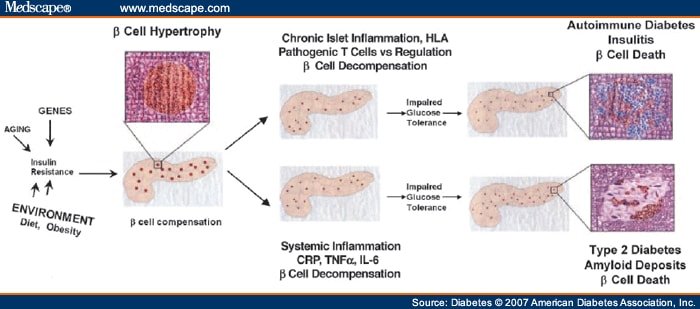
Generally, type 2 diabetes has been considered a metabolic condition that could degenerate into worse complications like fatty liver disease caused by too many fatty acids, heart disease, kidney failure, and stroke. However, considering what research now shows, its possibly more than that and could also result from autoimmunity.
The studies show that type 2 diabetes could develop from low-grade chronic inflammation following an attack on immune systems cells. This new revelation means that diabetes treatments may need to undergo significant changes to handle the new type 2 diabetes better. Its believed that these changes could finally help treatment focus on type 2 diabetes control more effectively.
Currently, the two major ways doctors treat diabetes are through lifestyle adjustments and medications. The former comprises healthy living, dieting, and keeping fit a strategy whose overall goal is to achieve consistent blood sugar control and weight management. Since obesity is linked with the condition, doctors usually recommend lifestyle adjustments as the healthiest and most natural way to tackle diabetes and blood sugar.
The other form of controlling type 2 diabetes is through medication. Some of the more common treatments are GLP-1 RAs and insulin injection. These medications are targeted to decrease blood sugar levels and improve insulin sensitivity.
What Are The Symptoms
The symptoms of autoimmune disease vary between types, but the common indicators are fatigue, fever, general malaise , joint pain and skin rash. Symptoms worsen during flare-ups and reduce during remission.
The common and most noticeable signs of type 1 diabetes are:
- Increased thirst
- Extreme tiredness
- Sudden or unexplained weight loss
These signs are often referred to as the 4Ts of type 1 diabetes Toilet, Thirsty, Tired and Thinner to help make them easier to remember.
Don’t Miss: How Much Is Insulin Out Of Pocket
Is Diabetes An Autoimmunedisease
Based on 2011 reports, scientists have redefined type 2 diabetes. Rather than just being a metabolic condition, it could also be an autoimmune illness. If thats true, then preventive tactics and new treatments can help manage the condition.
According to Daniel A. Winer, one of the study leaders, these findings could inspire new diabetes treatments that target the immune system instead of just managing the blood sugar.
Scientists estimate that insulin resistance happens because the immune cells and B cells are attacking their own bodies tissues. With this study, endocrine pathologists are in the process of revamping the most widespread illness in America as an autoimmune disease.
If successful, the study can change peoples perceptions about obesity and diabetes. It will most likely affect future diabetes treatment. To really understand where this is coming from, it is important to look at both type 2 and type 1 diabetes individually.
Adaptive Immune Responses In Islets

In addition to VAT inflammation, the pancreas is an organ found to be infiltrated with adaptive immune cells during obesity-linked inflammation and type 2 diabetes . Patients with type 2 diabetes display heightened pancreatic islet inflammation, initially characterized by increased expression of inflammatory cytokines derived from innate immune cells, such as TNF-, IL-1, and IL-12 , as well as deposition of islet amyloid polypeptide . These observations initially led researchers to propose that islet inflammation in type 2 diabetes is distinct from that in type 1 diabetes and is predominantly mediated by innate cells . Our understanding of the nature of islet inflammation in type 2 diabetes, however, is only starting to emerge. Studies found an increased prevalence of islet-associated antigen-specific antibodies and T-cell responses in patients with type 2 diabetes, targeting autoantigens, such as glial fibrillary acidic protein , GAD65, IA2, and proinsulin. Furthermore, a recent report documented an increased proportion of B cells within the islets of patients with type 2 diabetes compared with healthy control subjects . These studies provide evidence for a potential islet-specific adaptive immune process in type 2 diabetes.
Recommended Reading: Financial Help With Diabetic Supplies
Metabolic Control And Diabetes Complications
In the field of diabetes complications, at 10 years of diabetes duration, we report a significant higher frequency of microvascular complications in LADA, especially due to diabetic nephropathy. The slow progression of disease in LADA may be associated with asymptomatic hyperglycaemia before diagnosis, which together with other metabolic risk factors, leads to a continuous micro and macrovascular damage . There are reports in the literature of LADA patients with established micro and macrovascular complications in the first year after diabetes diagnosis . In our study, patients in the LADA group showed a trend to have higher weight, HbA1c and blood pressure values, and this may have contributed to the increased frequency of nephropathy in this group.
What Are The Most Common Autoimmune Diseases
Of the 80-plus autoimmune disorders, the most common ones include:
- Addisons disease immune system attacks the adrenal gland, disrupting production of steroid hormones aldosterone and cortisol.
- Coeliac disease autoimmune attack on substances found inside gluten damages the surface of the small bowel, disrupting the bodys ability to take in essential nutrients from food
- Hashimotos thyroiditis or Hashimotos disease similar to Graves disease, but this time damage to the thyroid gland lead to an underactive thyroid gland
- Multiple sclerosis myelin sheaths which protect the nerve fibres carrying messages to and from the brain are targeted by the immune system, causing behind scarring .
- Reactive arthritis immune system is tricked into thinking a previous infection is still present and attacks healthy tissue, causing it to become inflamed.
- Rheumatoid arthritis cells that line your joints are targeted by the autoimmune reaction, causing joints and surrounding tissues to become swollen, stiff and painful.
- Systemic lupus erythematosus immune system targets healthy tissue, causing inflammation of the skin and joints, and can affect internal organs
- Type 1 diabetes immune system destroys cells within the pancreas that produce the blood sugar-regulating hormone insulin.
Read Also: Can Probiotics Help With Diabetes
Why You May Need More Medication Over Time
After your initial diagnoses of type 2 diabetes, you may notice that its harder to reach your diabetes treatment targets even though your medication, exercise routine, diet, or other things you do to manage your diabetes hasnt changedand thats normal. Every so often, your routine to manage your diabetes will likely need to be adjusted. You might start managing your diabetes with diet and exercise alone, but, over time, will have to progress to medication, and further down the line you might need to take a combination of medications, including insulin.
Switching from taking an medications other than insulin, like metformin, to insulin can make you feel like you havent been doing enough to manage your diabetes. But this isnt true. Your body changes as it ages and diabetes is a progressive disease, so your need for different medications and treatments also changes.
While you may have to adjust your treatment plan and medications as your body changes and your diabetes progresses, it to helps prevent complications and helps you stay as healthy as possible.
How To Prevent Diabetes
In the above section, we considered some of the major risk factors that cause type 2 diabetes. Currently, the established diabetes risk factors are the only major cause of the condition since its autoimmunity hasnt been globally recognized.
Here, we outline some of the natural means that people can use to control high blood sugar, live more healthily and prevent the risk of autoimmunity as much as possible.
Read Also: How I Reversed My Diabetes
Clinical Aspects Of Autoimmunity In T2d
Since accumulating evidence show an etiopathological role of LGI in the development of T2D, clinical trials and observational studies have been designed to explore the effect of anti-inflammatory drugs on glucose parameters . On the other side, also glucose-lowering drugs can have anti-inflammatory effects. The description of the pleiotropic, beneficial, anti-inflammatory effects of selected anti-diabetic medications is beyond the scope of this manuscript and it has been largely reviewed elsewhere .
The first discovery linking LGI and T2D found an increased expression of TNF in the AT of obese subjects . A number of observational studies and small-pilot trials have tested the effect of anti-TNF biologicals on glucose parameters, showing improved insulin sensitivity in subjects without diabetes and with chronic inflammatory diseases, such as rheumatoid arthritis . While the use of TNF- antagonism is associated with an improved endothelial function in a wide range of patients , however, it has not demonstrated a tangible benefit in patients with T2D .
Strengths And Limitations On This Study
This is a retrospective study with the limitations related to this kind of design: the unavailability of all data in patients files and the non-uniform diagnostic and therapeutic strategies. The non-matching of patients in what concerns to disease duration in the groups may lead to some difficulties in interpreting the results. Nonetheless, the patients included in the study represent a real-world sample of diabetic patients followed on a tertiary care centre. To the best of our knowledge, few studies compared T1DM and LADA patients, especially with long duration of disease.
Read Also: Mens Low Cut Diabetic Socks
Eat Food High In Fiber
Eating food with fiber is essential for weight management and gut health. It could also prevent or reduce your risk of diabetes. Research on prediabetic people and old women with weight issues suggests that fiber helps lower insulin and blood sugar levels.
Fiber can be grouped into categories of soluble and insoluble. Soluble fiber absorbs water while insoluble doesnt. Water and insoluble fiber create a gel in the digestive tract that causes a decline in food absorption resulting in a slow rise in your blood sugar. So, eating foods with soluble fiber can reduce insulin and fasting blood sugar levels.
Research has also linked insoluble fiber to lowering blood sugar. Many studies on diabetes and fiber focused on supplements, but foods high in fiber are likely to be more beneficial in preventing diabetes.
Latent Autoimmune Diabetes Of The Adult
The presence of circulating autoantibodies in non-insulin-dependent diabetes mellitus was first identified more than 40 years ago . Nowadays, the presence of these autoantibodies characterizes a condition referred to as latent autoimmune diabetes of the adults . Autoantibodies against glutamic acid decarboxylase , islet cytoplasm , insulinoma-associated protein , and zinc transporter are commonly found in these patients.
At diagnosis, LADA patients do not usually need exogenous insulin and they appear to be clinically affected by T2D, but a large percentage will need it within a few years, showing a much faster decline of cell function compared to T2D patients, possibly caused by the ongoing immune-mediated cell destruction. Notably, Turner et al. showed that 94% of patients with ICA and 84% of those with GADA required insulin therapy by 6 years, compared with 14% of those without the antibodies . A small study has directly correlated the presence of islet autoantibodies with significantly lower acute insulin response when compared to that of the autoantibody-negative group, but observed similar peripheral IR, providing compelling evidence that the profound impairment of insulin secretion is plausibly determined by the immune-mediated injury of pancreatic cells .
You May Like: Can You Go Blind From Diabetic Retinopathy
How Can I Manage My Type 2 Diabetes
Managing your blood glucose, blood pressure, and cholesterol, and quitting smoking if you smoke, are important ways to manage your type 2 diabetes. Lifestyle changes that include planning healthy meals, limiting calories if you are overweight, and being physically active are also part of managing your diabetes. So is taking any prescribed medicines. Work with your health care team to create a diabetes care plan that works for you.
Insulin Resistance And Severe Insulin Resistance
Insulin resistance occurs when the cells of the body do not respond properly to insulin. This means the insulin produced by the pancreas cannot be used effectively. People with IR may need a much larger amount of insulin or other insulin sensitising medications to reach and stay within their blood glucose targets.
Don’t Miss: How To Care For Someone With Diabetes
Additional Information On Children And Teens
While children have been less affected by COVID-19 compared with adults, children can be infected with the virus that causes COVID-19, and some children develop severe illness. Children with underlying medical conditions are at increased risk for severe illness compared to children without underlying medical conditions.
Current evidence suggests that children with medical complexity, with genetic, neurologic, or metabolic conditions, or with congenital heart disease can be at increased risk for severe illness from COVID-19. Similar to adults, children with obesity, diabetes, asthma or chronic lung disease, sickle cell disease, or immunosuppression can also be at increased risk for severe illness from COVID-19. One way to protect the health of children not currently eligible for vaccination is to ensure that everyone who is eligible in a household is fully vaccinated against COVID-19.
What You Need To Know
- People of any age with the conditions listed below are more likely to get severely ill from COVID-19.
- COVID-19 vaccines and preventive measures for COVID-19 are important, especially if you are older or have multiple or severe health conditions including those on this list.
- Approved and authorized COVID-19 vaccines are safe and effective and should be administered to people at higher risk including people with underlying medical conditions. Learn more about COVID-19 vaccines for people with underlying medical conditions.
- Some immunocompromised people may be eligible for a COVID-19 additional primary dose.
- This list does not include all possible conditions that place you at higher risk of severe illness from COVID-19. If you have a condition not included here, talk to your doctor about how best to manage your condition and protect yourself from COVID-19.
Don’t Miss: Type 2 Diabetes Nerve Damage
Continue Medications And Preventive Care
- Continue your medicines and do not change your treatment plan without talking to your healthcare provider.
- Have at least a 30-day supply of prescription and non-prescription medicines. Talk to a healthcare provider, insurer, or pharmacist about getting an extra supply of prescription medicines, if possible, to reduce your trips to the pharmacy.
- Follow your current treatment plan to keep your medical condition under control.
- When possible, keep preventive care and other routine healthcare appointments with your provider. Check with your provider about safety precautions for office visits and ask about telemedicine or remote healthcare visit options.
- Learn about stress and coping. You may feel increased stress during this pandemic. Fear and anxiety can be overwhelming and cause strong emotions.
What The Experts Say: A New Outlook
Although there are considerations that push the ideology of diabetes being an autoimmune disease, health institutions havent formally confirmed this line of thought. However, this doesnt imply that the condition isnt connected to improper functioning of the immune system targeting diabetes-preventing cells.
Several studies indicate that type 2 diabetes could be an autoimmune condition just like type 1 diabetes, as pathogenic IgG antibodies were used to treat some of the immune cells that are believed to play a major role in triggering diabetes. The majority of these studies on type 2 diabetes showed that while other factors cause the condition, the possibility of the immune system targeting other healthy cells and tissues is also an eligible factor.
The Nature Medicine journal published one of the most reputable studies on diabetes being an autoimmune disease. The institution focused its research on finding treatments for type 2 diabetes by targeting the immune system instead of the traditional move of controlling blood sugar.
The study suggested that the B cells, a major part of the immune system, are among the causes of type 2 diabetes. The researchers who performed the study on mice used the anti-CD20 antibody to eliminate mature B cells in some samples, and the result showed that those with lesser B cells were less prone to the progression of type 2 diabetes.
Recommended Reading: Type 1 Diabetes Blurred Vision
Is Diabetes An Autoimmune Disease Breaking It Down
Diabetes is a metabolic disease, implying that its a condition that develops following a negative alteration of the bodys metabolism. While there are many classifications of the condition, type 2 diabetes comes to mind following general consideration, possibly due to its widespread nature and impact on general health. Type 2 diabetes has long been considered a problem related to blood sugar levels rise caused by obesity-related insulin resistance and other risk factors.
The second most popular type of diabetes is type 1 diabetes, established as an autoimmune disease. However, since it doesnt account for most diabetes cases globally, its barely regarded as diabetes. Below is a complete definition of the different types of diabetes that people experience:
Whats The Difference Between Type 1 And Type 2 Diabetes
Type 1 diabetes is an autoimmune disease that impacts 1.25 million American children and adults. For type 1, the immune system destroys the cells that release insulin, eventually leading to the complete inability to produce insulin in the body. Type 1 generally manifests at a young age and lasts a lifetime.
Type 2 diabetes has multiple contributing factors including genetics and lifestyle factors such as obesity and inactivity. The disease generally arises during adulthood and oftentimes can be reversed or controlled through diet and exercise. 90-95% of those diagnosed with diabetes have type 2.
You May Like: Pain Medicine For Diabetic Neuropathy