What Is Seattle Childrens Insulin Resistance Clinic
Our Insulin Resistance team works closely with children who have insulin resistance. This means the hormone insulin, which is made by the body, cannot keep a childs blood sugar levels normal after they eat or drink. With a healthy diet and exercise, it is possible to reverse insulin resistance and prevent type 2 diabetes.
- Why is insulin resistance a problem?
Insulin is made in the pancreas gland. Insulins job is to move sugar from the blood and turn it into energy. When insulin does not work right, the body tries to help by making more. This extra insulin keeps blood sugars normal for a while. But over time, the pancreas cannot make enough insulin. Blood sugar levels get too high, which can develop into type 2 diabetes.
- How do I know if my child has insulin resistance?
The signs and symptoms can vary, but some are easy to see. If your childs body makes too much insulin, they often develop patches of dry, darker skin on their neck, under the arms or in the groin area. This is called acanthosis nigricans. Some children have:
- Brain fogginess
- High blood sugar
- Higher blood pressure
Genotype And Phenotype Testing
Genetic testing is available through commercial laboratories for 4 of the 6 genes known to be associated with HI . In addition, acute insulin response tests are useful in phenotypic characterization: patients with diffuse KATP-HI display abnormal positive responses to calcium, abnormal negative response to the KATP-channel antagonist tolbutamide, and impaired responses to glucose . Focal and diffuse HI are clinically indistinguishable and AIR tests do not reliably differentiate between the two . Infants with GDH-HI demonstrate an increased response to leucine . For infants with prolonged stress-induced HI, AIR testing shows that, in general, the patterns of insulin response to calcium, tolbutamide, glucose, and leucine resemble those of normal controls .
What Is A High Insulin Level
Insulin is a hormone that is secreted by an abdominal organ called the pancreas. It controls the breakdown of carbohydrates, fats and proteins in the body. It also guides the liver and muscles to store glucose and fat that can be used during periods of increased energy requirements and fasting. Insulin is a key that unlocks the cell gates so that glucose from the blood enters the cells. The cells of the muscle and fat tissue are dependent solely on insulin for glucose uptake and use.
The lack of insulin in the body or inefficient insulin action at cellular levels causes blood sugar levels to spike . Hyperglycemia is the hallmark of diabetes mellitus. Insulin is the only hormone in the body that can prevent hyperglycemia.
Hyperinsulinemia: Some individuals require higher than normal amounts of insulin to maintain their blood sugar levels. This condition is called hyperinsulinemia. It is often found to co-exist with insulin resistance.
Insulin resistance is a state in which a given insulin concentration does not cause an expected dip in blood sugar levels. Insulin resistance may be caused by
- Antibodies to insulin or to the site in the cell where insulin binds .
- Suboptimal quality insulin as seen in people with certain genetic diseases.
- Genetic tendency to insulin resistance as seen in the people of Latino, African American, Native American or Asian-American heritage.
Read Also: Best Way For A Type 1 Diabetes To Lose Weight
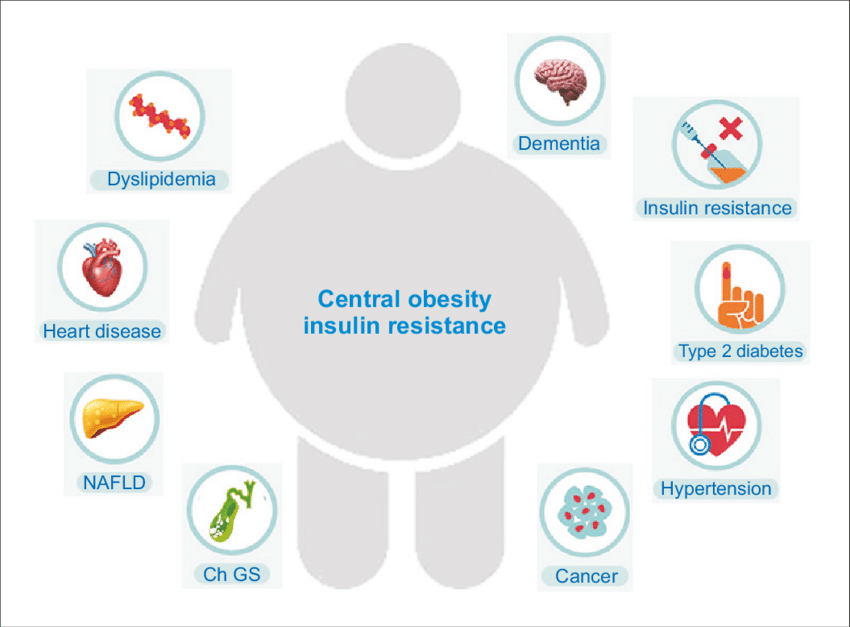
Insulin Resistance: Definition And Pathogenesis
Insulin resistance is a state in which a given amount of insulin produces a subnormal biological response . In particular, it is characterized by a decrease in the ability of insulin to stimulate the use of glucose by muscles and adipose tissue and to suppress hepatic glucose production and output . Furthermore, it accounts a resistance to insulin action on protein and lipid metabolism and on vascular endothelial function and genes expression .
Several defects in the insulin signalling cascade have been implicated in the pathogenesis of insulin resistance, such as reduced synthesis or increased degradation of components of the system, an increased inhibitory serine phosphorylation of the insulin receptor or the insulin receptor substrates, the interaction of components of the system with inhibitory proteins or an alteration of the ratio of the different proteins of the signalling cascade .
Insulin resistance is believed to have both genetic and environmental factors implicated in its aetiology . The genetic component seems to be polygenic in nature, and several genes have been suggested as potential candidates . However, several other factors can influence insulin sensitivity, such as obesity, ethnicity, gender, perinatal factors, puberty, sedentary lifestyle and diet .
Your Childs Correction Factor Will Look Like This:
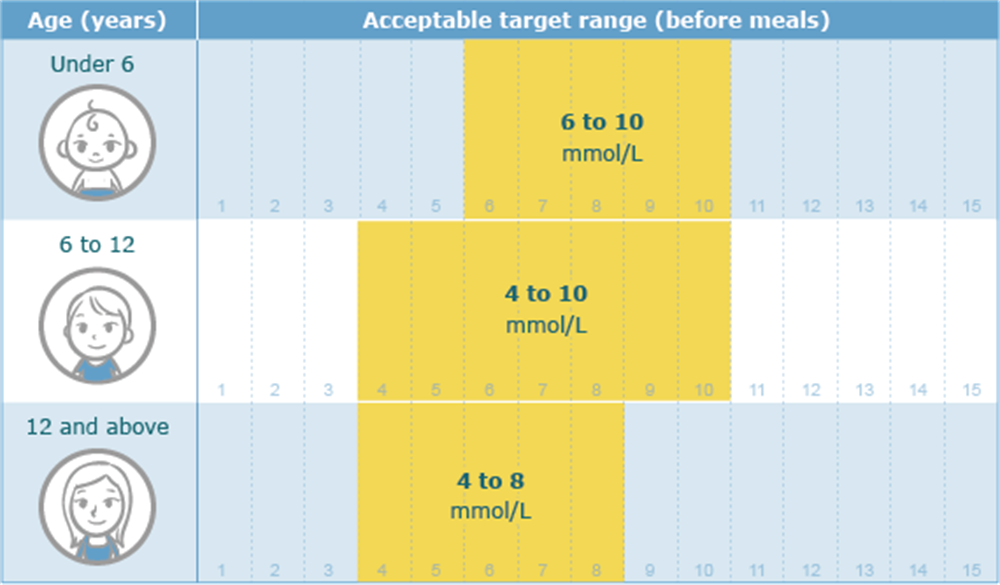
unit for every point that blood sugar is over
For example, a correction factor of 1:50> 150 means your child will take one unit of fast-acting insulin for every 50 points their blood sugar is over 150 .
To calculate this, take your childs current blood sugar and subtract their target blood sugar. Divide the result by 50, and multiply that result by the number of units.
Here is an example of a correction factor calculation:
If your childs correction factor is 1:50> 150 and their current blood sugar is 233:
- 233 minus 150 equals 83
- 83 divided by 50 equals 1.6
- 1.6 multiplied by 1 equals 1.6
This means your child needs to take 1.6 units of insulin to bring their elevated blood sugar down to their target blood sugar.
Also Check: How To Treat Sugar Diabetes
Ir As An Initiator Of Atherosclerosis
Studies of adults have shown that there is an association between IR and atherosclerosis, Increased thickness of the arterial carotid wall and an atherogenic dyslipidemic profile that includes hypertriglyceridemia, low serum HDL cholesterol concentrations, and atherogenic low density lipoprotein cholesterol particles compounded by low SHBG levels are factors for increased risk of atherosclerosis.
Importantly, hyperinsulinemia is an independent cardiovascular risk factor . The Muscatine Study linked childhood coronary risk factors to atherosclerosis in asymptomatic adults. The most predictive childhood risk factor was increased BMI. Coronary artery calcifications were also associated with increased blood pressure and decreased HDL cholesterol levels measured during childhood . Fatty streaks can be found in the aorta inchildren older than 3 yr of age and in coronary arteries by adolescence . The Bogalusa Heart Study confirmed that the same risk factors that are important for adults, such as elevated BMI, systolic blood pressure, serum TG, and LDL lipoproteins, convey greater atherosclerosis risk in the aorta and coronary arteries in children . The Pathobiological Determinants of Atherosclerosis in Youth study confirmed the origin of atherosclerosis in childhood, showed that progression toward clinically significant lesions may occur in young adulthood, and demonstrated that the progression of atherosclerosis is strongly influenced by CHD risk factors .
Treatment Of Obesity And Insulin Resistance
A balanced diet and increased physical activity are generally the cornerstone of the treatment of obesity and insulin resistance in children and adolescents. Decreases in body weight have been associated with a significant improvement in insulin sensitivity . A recent study has shown that in obese children, an 8-week exercise training programme increased insulin sensitivity and was associated with an improvement in cardiorespiratory fitness but was independent of measurable changes in body composition .
In children and adolescents, there is not a wide experience with weight loss medications or with insulin sensitizers. Metformin has been shown to improve insulin sensitivity and BMI in non-diabetic obese adolescents with fasting hyperinsulinemia and a family history of T2DM . A similar efficacy of metformin on insulin sensitivity and BMI has been found in two other small studies conducted in obese normoglycemic adolescents .
Sibutramine seems to have a good efficacy in reducing body weight in children and, in some studies, a positive effect on glucose and lipid metabolism has also been shown . However, this drug has been associated with an increase in blood pressure and heart rate, thereby posing limitations for its wide use in the paediatric population .
In adults thiazolidinediones have also been shown to have a good efficacy in improving insulin sensitivity however, their use in children has not been yet approved, based on the lack of relevant studies in this age group.
Don’t Miss: When Does Type 2 Diabetes Need Insulin
When To Call The Diabetes Team
You should always fix low blood sugars right away. Its also important to recognize when changes need to be made and adjust doses between clinic visits to reduce the chances of long term complications.
- Your childs blood sugars are worse after making a change in their insulin dose or if you make more than 3 changes in the dose since their last clinic visit
- Moderate or large ketones are present
Do you still have questions about when you should change your childs insulin doses? Contact the diabetes team at Childrens Diabetes Center, Childrens Hospital & Medical Center at for more information about insulin doses and pattern control.
How Is Insulin Resistance Treated
Insulin resistance is treated with positive lifestyle changes. Weight loss can bring big gains in blood sugar, lipids, and blood pressure. In kids who are still growing, slowing the rate of weight gain or keeping a healthy weight also will help.
Families can work with their health care provider, a dietitian, or a weight management program to build healthy habits. These might include:
- limiting junk food and sugary beverages
- eating more fruit and vegetables
- choosing whole grains
Also Check: How To Get Rid Of Diabetes Stomach Fat
Get Tested For Diabetes
If you’re experiencing symptoms of high blood sugar, speak with your doctor right away. He or she will likely want to test you for prediabetes or diabetes.
Diabetes is usually diagnosed with a blood test. It is also common to take an oral glucose tolerance test, according to the Mayo Clinic. This test is typically performed first thing in morning, because you’ll have to fast for at least eight hour in advance. The test includes consuming a very sugary drink and then having your blood glucose checked at regular intervals to see how your body is responding to the carbohydrates.
Here are the possible results: A normal fasting blood sugar level is less than 95 milligrams per deciliter . Two hours after drinking the glucose solution, a normal blood sugar level is less than 140 mg/dL. If your results show a blood sugar level between 140 and 199 mg/dL, you will be considered to have prediabetes. If, after two hours, your blood sugar is 200 mg/dL or higher, it indicates diabetes.
If you are diagnosed with prediabetes or diabetes, you will need to make lifestyle changes. This often includes dietary changes, increased exercise and possibly medications. If diabetes goes untreated, it can, over time, severely damage other parts of the body, including the eyes, liver and kidneys, per the National Institutes of Health.
Read more:Does Eating Cucumber Help Lower Blood Sugar for People With Diabetes
Who Gets Hyperglycemia In Infants
- Hyperglycemia in Infants is seen in both term and preterm infants. This form of hyperglycemia is seen in infants shortly after birth from birth to one month of age
- Both sexes are equally likely to develop Hyperglycemia. The gender of the baby has no effect on the development of this condition
- All racial and ethnic groups are generally affected
- In general, North America has the highest prevalence of diabetes , followed by the Middle East and North Africa. This corresponds to an increased risk of Hyperglycemia in Infants, because in areas with high prevalence of diabetes, the risk of the mother developing gestational diabetes mellitus and the infant developing hyperglycemia is higher
Recommended Reading: Diabetic Diet Plan To Lose Weight
What Are The Treatment Options
Treatment for hyperinsulinemia begins by treating whatever is causing it. This is particularly true if your condition is caused by insulinoma or nesidioblastosis.
Your treatment may also include a combination of medication, lifestyle changes, and possibly surgery. These lifestyle changes include diet and exercise.
Type 2 Diabetes Complications
Without treatment, type 2 diabetes appears to progress faster in young people than in adults.
Younger people also seem to have a higher risk of complications, such as kidney and eye disease, earlier in life.
There is also a greater risk of high blood pressure and high cholesterol levels, which increase a persons risk of blood vessel disease.
Type 2 diabetes in children often occurs with obesity, which may contribute to these higher risks. Obesity affects the bodys ability to use insulin, leading to abnormal blood sugar levels.
Because of this, early detection of type 2 diabetes and attention to managing overweight and obesity in younger people are crucial.
This may include encouraging children to follow a healthful diet and get plenty of exercise.
The National Institute for Health Care and Excellence recommend testing children for diabetes if they:
- have a strong family history of type 2 diabetes
- have obesity
- are of Black or Asian family origin
- show evidence of insulin resistance, such as acanthosis nigricans
The outcomes for children with type 1 or type 2 diabetes improve greatly with early detection.
It is not currently possible to prevent type 1 diabetes, but type 2 diabetes is largely preventable.
The following steps can help prevent type 2 diabetes in childhood:
- Maintain a moderate weight: Overweight increases the risk of developing type 2 diabetes, as it increases the chance of
Don’t Miss: Insulin Syringes 31 Gauge 8mm
Pediatric Hyperinsulinemia Treatment In Novi Mi
Hyperinsulinemia is not diabetes, but it means that there is a higher-than-normal amount of insulin in a persons blood. The condition is often associated with type 2 diabetes. It can be caused by insulin resistance, in which the pancreas makes more insulin to compensate for the bodys resistance to its effects.
If your child is overweight or obese and you are concerned that they might be insulin resistant or at risk for type 2 diabetes, contact Endocrine Kids to learn more about our weight management pathway. Call our Novi, Michigan office at for an appointment, or you can use our secure online appointment request form.
Natural History Of The Clinical Irs
The natural history of IRS begins in childhood, from the interplay of genetic and environmental factors . Although it is generally unclear whether a primarily genetically encoded state of IR and/or satiety disorder appears first, IR results in hyperinsulinism and precocious development of atherosclerosis and type 2 diabetes . A contemporary diet from early childhood replete with large amounts of saturated fats and excess carbohydrates is probably important to the development of hyperinsulinemia and obesity. The epidemic of obesity and diabetes follows U.S. commercially driven drink and food sources, with consumption of large amounts of sodas and fruit juices, and foods with a high glycemic index. Dietary carbohydrates induce hyperinsulinism, a reduction in fatty acid oxidation, and hypertryglyceridemia. Diets rich in saturated FAs add a strong insulinotropic effect. In children, obesity and IR precede the development of hyperinsulinism. The hyperinsulinemia can thus be seen a compensatory mechanism for the preexisting, genetically programmed IR, which represents a mechanism for protection against the development of IGT and diabetes.
Natural history of developing diabetes type 2.
You May Like: What Should My Sugar Level Be With Type 2 Diabetes
Fatty Liver Or Hepatic Steatosis
Hepatic steatosis is another complication of IR that may progress over years with inflammation and fibrosis . At least 20% of such individuals eventually develop cirrhosis, liver failure, or hepatocellular carcinoma. Fatty liver affects 2.6% of children , and 22.552.8% of obese children and 1025% of adolescents . In adult patients with diabetes and obesity, 100% have mild steatosis, 50% have steatohepatitis, and 19% have cirrhosis . The disease is usually silent over many years. Serum levels of alanine aminotransferase , aspartate aminotransferase, alkaline phosphatase, and -glutamyltransferase are elevated and have been proposed as surrogate markers of hepatic fat accumulation . The ratio of aspartate aminotransferase to ALT is usually less than 1, but this ratio increases as fibrosis advances.
Assessment Of Nutritional Status
Height, weight, waist circumference and hip circumference were measured in all participants using a standard protocol . Body mass index /height 2), waist hip ration /HC ) and waist to height ratio /Ht ) were calculated. Nutritional status of children was assessed based on IOTF and categorized as obese, overweight and lean. Cutoff values for %FM used was 28.6% for boys and 33.7% for girls . All assessments were done by trained research assistants who were medical graduates.
Recommended Reading: How Long Does Insulin Take To Work
Diagnosis Of Diabetes In Children
Diagnosis of diabetes and prediabetes is similar to that in adults, typically using fasting or random plasma glucose levels and/or HbA1c levels, and depends on the presence or absence of symptoms . Diabetes may be diagnosed with the presence of classic symptoms of diabetes and blood glucose measurements. Measurements are random plasma glucose 200 mg/dL or fasting plasma glucose 126 mg/dL fasting is defined as no caloric intake for 8 hours.
An oral glucose tolerance test is not required and should not be done if diabetes can be diagnosed by other criteria. When needed, the test should be done using 1.75 g/kg glucose dissolved in water. The test may be helpful in children without symptoms or with mild or atypical symptoms and may be helpful in suspected cases of type 2 or monogenic diabetes. The HbA1c criterion is typically more useful to diagnose type 2 diabetes, and hyperglycemia should be confirmed.
Congenital Defects Of Insulin Function
In presence of children with severe phenotypes, an inherited alteration of the action of insulin should be suspected and fasting serum insulin should be measured. If insulin is elevated with normal or high blood glucose, additional studies should be directed to look for insulin receptor mutations, circulating anti-insulin receptor antibodies, or other disorders.
Inherited lipodystrophies are rare disorders in which selective loss of adipose tissue and a predisposition to insulin resistance are typical . Among them, some manifest at birth, such as congenital generalized lipodystrophy and neonatal progeroid syndrome, while others have a later onset, such as familial partial lipodystrophies and mandibulosacral dysplasia manifest later in life. The higher is the extent of body fat loss in these patients, the more severe is the metabolic syndrome by which they are affected. Table 1 lists all subtypes of genetic lipodystrophies classifying them according to their possible inheritance patterns or their possibility to be caused by a de novo heterozygous mutation. The two most prevalent variations are CGL and FPLD. For its complex clinical presentation and severe metabolic complications we will focus on CGL, which has an estimated prevalence of 1 in 10 million.
Table 1. Genetic lipodystrophies listed according to their possible inheritance patterns.
Read Also: Type 2 Adult Onset Diabetes