Youre Eating Healthy Foods But Youre Eating Too Much
Portion control is vital to managing your A1C, Gallagher says. Watching the amount you eat helps you maintain a healthy weight, but it also helps you manage your intake of carbohydrates and maintain healthy blood sugar levels, according to the Centers for Disease Control and Prevention . The agency offers a guide for estimating portion sizes. They also recommend taking steps to control your food intake, such as measuring out portions of snacks, rather than eating straight from the bag or box, and having your server wrap half of your meal if youre eating out, so you can enjoy it later. A registered dietitian or certified diabetes care and education specialist can help you develop a meal plan to help keep your blood sugar under control.
Aspects Of Insulin Resistance
Hayashi et al. followed 407 Japanese Americans not receiving diabetes treatment over 1011 years, finding that computed tomography -scan measurement of intra-abdominal fat area showed significant correlation with subsequent insulin resistance based on homeostasis model assessment reported greater association of CT volumetric measures of visceral than subcutaneous adipose tissue with diabetes risk and significant effect of visceral adiposity after adjusting for BMI and waist circumference in women but not in men among 1,189 participants from the Framingham Offspring cohort. Of course, a great deal more than total fat measures may be gleaned from imaging studies, with Matsuda et al. finding that pancreatic CT density was 43% lower among 69 type 2 diabetic individuals receiving insulin than among 63 diet onlytreated patients, suggesting pancreatic fat accumulation contributing to -cell damage.
Treatment Thats No Longer Effective
Type 2 diabetes can progress or change, which means sometimes a different treatment approach might be necessary to manage your A1C level.
If your treatment is no longer effective and is impacting your blood sugar levels, talk with your doctor about making an adjustment. You may need to:
- start taking medication if youre currently managing with diet and exercise
- change the dosage of your current medication
- switch to a new medication
- switch from oral diabetes medications to insulin
Your blood sugar naturally fluctuates throughout the day. Many things can impact your blood sugar, such as:
- the amount of carbohydrates you eat
- your physical activity level
- quality of sleep
- stress
Fluctuating blood sugar can affect your A1C readings, which is the average of your blood sugar over a few months.
Testing your blood sugar regularly can help you see how certain factors affect your blood sugar and help you stay in your target range.
Read Also: Travel Insurance For Type 1 Diabetes
New Type 2 Diabetes Treatment Approaches
Bile acid sequestrants may lower glucose as well as LDL cholesterol levels, in individuals with diabetes. Kalin et al. , Schwarz et al. , and Zieve et al. administered 3.75 g colesevelam daily versus placebo to 59 type 2 diabetic individuals, finding a placebo-adjusted reduction in fasting glucose of 23 and 18 mg/dl at 4 and 8 weeks, respectively. At 12 weeks, fasting glucose had fallen from 170 to 165 mg/dl, and the glucose level 1 h following a sucrose-containing meal decreased from 269 to 251 mg/dl with colesevelam, while with placebo fasting glucose increased from 188 to 190 mg/dl and postprandial glucose increased from 285 to 288 mg/dl. There was a 0.2% reduction in A1C versus a 0.3% increase among individuals receiving placebo from the 8% baseline. LDL cholesterol fell from 123 to 108 mg/dl with colesevelam, whereas it increased from 120 to 122 with placebo. Kawabata et al. administered the similar anion-exchange resin colestimide, 3 g daily, to 27 type 2 diabetic individuals, finding a decrease in A1C from 7.7 to 6.8%, in fasting glucose from 164 to 152 mg/dl, and LDL cholesterol from 130 to 103 mg/dl.
Discussion In Support Of The Acp Guidelines
The first guidance statement concurs with the existing guidelines, all of which recommend personalizing treatment.
The second guidance statement reflects the observation that, collectively, all of the trials upon which these guidelines were based showed that treating to targets of < 7% versus around 8% did not reduce mortality or macrovascular morbidity from over 5 to 10 years of treatment but did lead to substantial harms. Of course, this need not apply to patients who are able to achieve an HbA1c of 6.5% through diet, exercise and lifestyle modifications alone, observed Dr. Ende.
According to David W. Lam, MD, Assistant Professor of Medicine in the Division of Endocrinology, Diabetes and Bone Diseases at the Icahn School of Medicine at Mount Sinai , the key takeaway from this updated guideline is the personalization of care by considering multiple comorbidities of the patient, life expectancy, and ultimately considering the risk/benefit ratio of intensifying glycemic control.
A major change in the paradigm of diabetes treatment comes from guidance statements 3 and 4, more specifically the de-escalation of medical therapy with HbA1c less than 6.5% and the shift from a focus on an HbA1c target to focusing on the avoidance of symptoms from hyperglycemia.
Also Check: How To Heal Diabetic Ulcers
When Goals Are Not Met In Diabetes Care
The American Journal of Accountable Care
A presentation at the fall live meeting of the ACO & Emerging Healthcare Delivery Coalition® focused on the clinical and economic consequences of not meeting glycemic goals in patients with type 2 diabetes.
Clinical and economic burdens are placed on the US healthcare system when target goals are not met in diabetes care. In 2012, total costs associated with diabetes in the United States were $245 billion dollars.1 In a presentation at the 2017 Fall ACO & Emerging Healthcare Delivery Coalition®, hosted by The American Journal of Managed Care®on October 26th, 2017, Kari Uusinarkaus, MD, discussed the economic impact of type 2 diabetes . This presentation focused on the prevalence, costs, and consequences of not meeting glycemic goals in patients with T2D.
Approximately 16.5 million people in the United States have T2D.2 The majority of adult patients with diabetes have T2D.1 Risk factors associated with the occurrence of T2DM include ethnicity , male gender, older age, obesity, family history, gestational diabetes, impaired glucose metabolism, and physical inactivity.
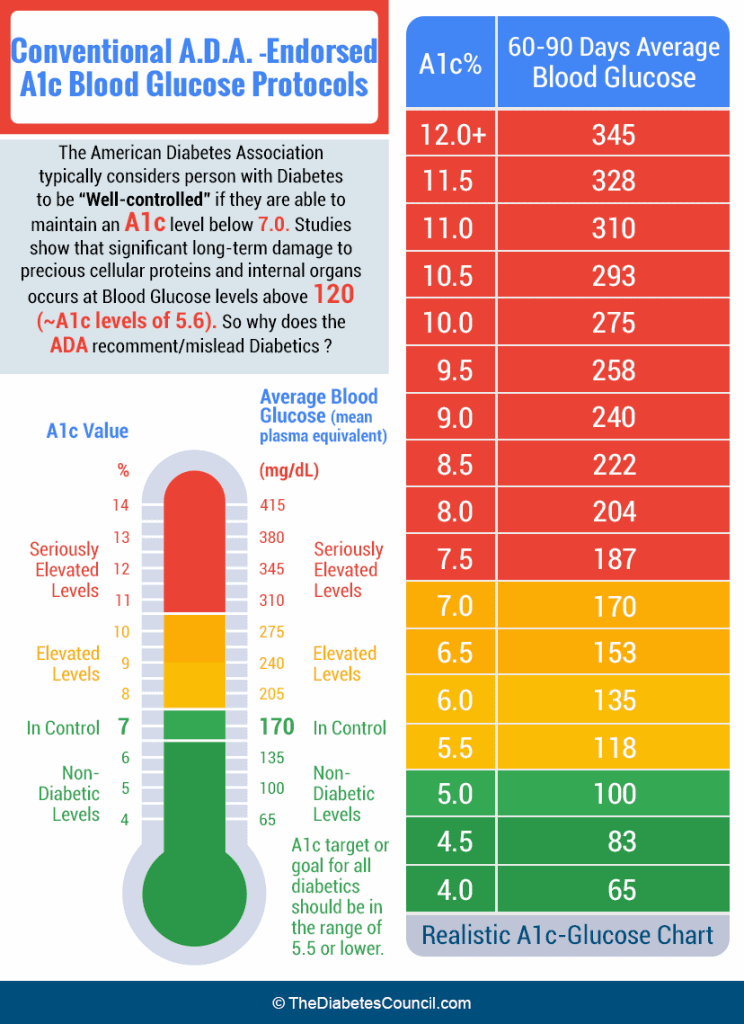
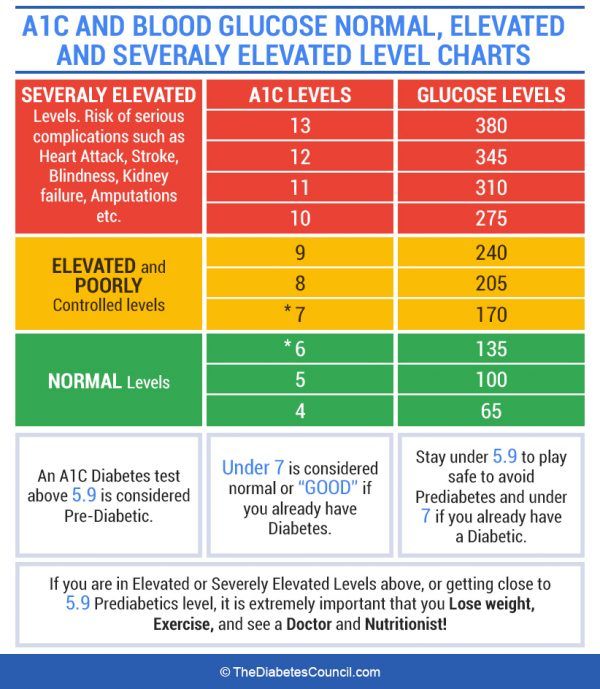
Both the American Diabetes Association and the American Association of Clinical Endocrinologists/American College of Endocrinology have established target goals to decrease cardiovascular comorbidities associated with T2D.6,7 These recommended targets are described in Table 1.
- 27% reduction in all-cause mortality after 10 years of& thinsp follow-up.
We Dont Even Need To Follow The A1c For Some Patients
Elderly patients, and those with serious medical conditions, will benefit from simply controlling the symptoms they have from high blood sugars, like frequent urination and incontinence, rather than aiming for any particular A1c level. Who would be included in this group? People with a life expectancy of less than 10 years, or those who have advanced forms of dementia, emphysema, or cancer or end-stage kidney, liver, or heart failure. There is little to no evidence for any meaningful benefit of intervening to achieve a target A1c in these populations there is plenty of evidence for harm. In particular, diabetes medications can cause low blood sugars, leading to weakness, dizziness, and falls. There is the added consideration that elderly and sick patients often end up on a long list of medications that can interact, causing even more side effects.
Recommended Reading: Can You Control Diabetes With Diet And Exercise
A1c And Microvascular Complications
Hyperglycemia defines diabetes, and glycemic control is fundamental to diabetes management. The Diabetes Control and Complications Trial , a prospective randomized controlled trial of intensive versus standard glycemic control in patients with type 1 diabetes, showed definitively that better glycemic control is associated with 5076% reductions in rates of development and progression of microvascular complications. Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications study demonstrated persistence of these microvascular benefits over two decades despite the fact that the glycemic separation between the treatment groups diminished and disappeared during follow-up.
The Kumamoto Study and UK Prospective Diabetes Study confirmed that intensive glycemic control significantly decreased rates of microvascular complications in patients with short-duration type 2 diabetes. Long-term follow-up of the UKPDS cohorts showed enduring effects of early glycemic control on most microvascular complications .
Three landmark trials were conducted to test the effects of near normalization of blood glucose on cardiovascular outcomes in individuals with long-standing type 2 diabetes and either known cardiovascular disease or high cardiovascular risk. These trials showed that lower A1C levels were associated with reduced onset or progression of some microvascular complications .
Navigating The Targets For Hba1c
With more than 100 million U.S. adults living with diabetes and prediabetes,¹ the value of education and treatment for this condition cannot be overstated. The health and economic costs of managing, rather than improving, the complications associated with diabetes necessitate a careful look at the treatment options that are available for this disease.
Summary of Recommendations from the ACP Guidance Statement:âµ
- Clinicians should personalize goals for glycemic control
- Aim to achieve HbA1c 7â8% in most patients
- De-intensify pharmacologic therapy when HbA1c < 6.5%
- Avoid targeting HbA1c level in certain patient populations
The ACP determined that the risks associated with intensive medication therapy aimed at achieving tight HbA1c control were greater than the benefits, asserting that the evidence did not support enough of an improvement in outcomes for patients with an HbA1c of less than 7% versus 7â8%. The statement cited concerns with intensive pharmacologic treatment as it relates to adverse events, medication costs and patient burden, as well as the risk-benefit analysis based upon a patientâs health status.âµ According to the ACP, their guidance statement is consistent with the recommendations of the Institute for Clinical Systems Improvement guideline from 2014 wherein a recommendation for > 7% â < 8% was provided in order to manage the potential complications of intensive medication therapy.â¶
Recommended Reading: Signs Your Kid Has Diabetes
High Risk For Hypoglycemia Or Presence Of Hypoglycemia Unawareness
Noninsulin-dependent medications such as metformin, SGLT2 inhibitors, GLP-1 receptor agonists, or DPP-4 inhibitors are preferred for patients who are prone to hypoglycemia or have hypoglycemia unawareness. Insulin secretagogues should be avoided. If insulin is needed, levemir and degludec have a lower incidence of hypoglycemia than glargine or NPH .
Know Your Family History
Did your mother, grandfather, or other close relative have a stroke or heart attack? Check out your family tree to get clues about your medical future. Having family members with heart disease makes you more likely to follow the same path. And if one or more relatives had a heart attack before age 50, your chances of heart disease could be even higher. Learning your family history can give you incentives to take care of your health.
Recommended Reading: How To Administer Insulin And D50 For Hyperkalemia
What Does The A1c Test Measure
When sugar enters your bloodstream, it attaches to hemoglobin, a protein in your red blood cells. Everybody has some sugar attached to their hemoglobin, but people with higher blood sugar levels have more. The A1C test measures the percentage of your red blood cells that have sugar-coated hemoglobin.
A1c Differences In Ethnic Populations And Children
In the ADAG study, there were no significant differences among racial and ethnic groups in the regression lines between A1C and mean glucose, although the study was underpowered to detect a difference and there was a trend toward a difference between the African and African American and the non-Hispanic White cohorts, with higher A1C values observed in Africans and African Americans compared with non-Hispanic Whites for a given mean glucose. Other studies have also demonstrated higher A1C levels in African Americans than in Whites at a given mean glucose concentration .
A1C assays are available that do not demonstrate a statistically significant difference in individuals with hemoglobin variants. Other assays have statistically significant interference, but the difference is not clinically significant. Use of an assay with such statistically significant interference may explain a report that for any level of mean glycemia, African Americans heterozygous for the common hemoglobin variant HbS had lower A1C by about 0.3 percentage points when compared with those without the trait . Another genetic variant, X-linked glucose-6-phosphate dehydrogenase G202A, carried by 11% of African Americans, was associated with a decrease in A1C of about 0.8% in hemizygous men and 0.7% in homozygous women compared with those without the trait .
You May Like: Type Of Exercise For Diabetes
Achieving Glycemic Goals In Type 2 Diabetes
Zachary T. Bloomgarden Achieving Glycemic Goals in Type 2 Diabetes. Diabetes Care 1 January 2007 30 : 174180.
This is the fourth in a series of articles on presentations at the American Diabetes Associations 66th Scientific Sessions, Washington, DC, 913 June 2006, addressing aspects of the treatment of type 2 diabetes.
A pilot project is underway to offer the Perspectives on the News commentaries as a monthly Web-based CME activity. Please access www.diabetes.procampus.net to view our initial efforts. We look forward to your comments.
What Are The Blood Sugar Targets For Diabetes
The ADA recommendations are general guidelines and may be modified according to individual situations. Discuss with your medical provider what treatment goals are best for you. For example, if you are not taking any medications or your diabetes treatment doesnt increase the risk of low blood sugars your provider may recommend that you keep your blood sugar in the normal range or closer to the normal range. Pregnant women or women thinking about getting pregnant also have lower blood glucose targets.
When you have diabetes and are treated with insulin replacement therapy or medications that increase insulin release from your pancreas, the insulin levels in your blood stream are imperfectly matched to how much insulin you actually need and there is always a risk of having too much insulin effect. Too much insulin effect can cause a low blood sugar or hypoglycemia. To minimize this risk, your provider may recommend that you target higher blood sugars such as a pre-meal blood sugar of 90-130 mg/dl and post meal blood sugar of less than 180 mg/dl.
American Diabetes Association Recommendations
| After Meal Glucose Level | < 180 mg/dl |
*Hemoglobin is a measure of your average blood glucose control over the previous 3 months. Think of the A1c as a long-term blood glucose measure that changes very gradually.
Read Also: Best Vitamin C Supplement For Diabetics
What Should Be My Hba1c Level
The clinical studies, as well as Dr. Richard K. Bernstein experience, confirms an A1C target of 4 to 4.6% is the best. This goal helps to avoid diabetes complications and provide the longest life expectancy.
Non-diabetic A1C is usually between 4.0 to 5.0%. For diabetics, both type 1 & 2, A1C target should be < 5.0%. A1C levels above 5.0% increase your risk towards diabetes complications.
People with diabetes should lower the HbA1c level. However, the hypoglycemia risk is high, if you try achieving A1C below 4.6%.
How damaging or dangerous is a hemoglobin A1C of over 8?
An A1C of over 8% is surely not okay. At the same time, it does not mean you are going into ketoacidosis, coma, or die! However, you should take it seriously as a danger alarm.
A1C of 8% does not mean your kidneys are going to fail, heart stop working, or you are going to blind tomorrow. However, it might happen if it stays there for years.
Many have an A1C close to or even more than 8% when first diagnosed as diabetic. It is possible to bring under 7% in just three months then below 5% if you put consistent effort. You should strive to take it below 7% at your earliest. High level for months are dangerous still, you have time to turn around.
Bp Control And Its Optimal Value
Optimal value was only detected for SBP in the models fitting for macrovascular complication. Lower SBP was correlated to lower risk of microvascular complication. To minimize the risk of macrovascular complication, optimal SBP was found at 131mmHg. Lower SBP may increase the risk of macrovascular complication in our study. BP of 143/82mmHg was estimated with lowest risk of vascular events. However, the population used in this study was not patients with T2DM. A retrospective study found that an optimal SBP of 128mmHg was associated with best outcome of diabetic nephropathy. Considering the risk of macrovascular complication, we found that higher SBP might be the best SBP value for the general population with T2DM.
Also Check: Best Insulin For Type 2 Diabetes
Setting And Modifying A1c Goals
Numerous factors must be considered when setting glycemic targets. The ADA proposes general targets appropriate for many patients but emphasizes the importance of individualization based on key patient characteristics. Glycemic targets must be individualized in the context of shared decision making to address the needs and preferences of each patient and the individual characteristics that influence risks and benefits of therapy for each patient.
The factors to consider in individualizing goals are depicted in . is not designed to be applied rigidly but to be used as a broad construct to guide clinical decision making in both type 1 and type 2 diabetes. More stringent control may be recommended if it can be achieved safely and with acceptable burden of therapy and if life expectancy is sufficient to reap benefits of tight control. Less stringent control may be recommended if the life expectancy of the patient is such that the benefits of an intensive goal may not be realized, or if the risks and burdens outweigh the potential benefits. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals.
Does Insurance Cover A Type 2 Diabetes Care Plan
Some insurance providers may cover type 2 diabetes care plans within the context of DSM training.
For example, Medicare covers DSM training to prepare individuals to cope with and manage their condition. A care plan could also be part of this.
People with Medicare pay 20% of the Medicare-approved amount after the yearly deductible.
Many states require that insurers cover DSM training. This means that state-mandated insurers, such as Medicaid, are also likely to provide coverage.
However, individuals should check their policy documents to find details of coverage for their specific policy.
Don’t Miss: Diabetes How To Control Blood Sugar