How Do You Administer Iv Insulin
Mix 250 units of regular human insulin in 250 mL of normal saline . Flush approximately 30 mL through the line prior to administration. Do not use a filter or filtered set with insulin. Piggyback the insulin drip into intravenous fluid using an intravenous infusion pump with a capability of 0.1 mL/hr.
Errors When Treating Hyperkalemia
When treating hyperkalemia, the potential for errors and patient harm is significant due to the urgency of the treatment, the difficulty in measuring and administering bolus doses of IV insulin, and the risk of treatment-induced hypoglycemia. A 2017 analysis of almost 200 adverse events associated with hyperkalemia treatment showed that delayed treatment and administration of insulin by the wrong route or the wrong dose were the most common types of errors.1 The analysis also showed that, despite the administration of dextrose, hypoglycemia was still a relatively common occurrence often linked to the variability in dextrose and insulin dosing, the type of insulin used, duration of the dextrose and insulin infusion, the sequence of administering the dextrose and insulin, and patient factors such as renal dysfunction. Some episodes of hypoglycemia have also been caused by administering only the insulin portion of the treatment and not the glucose component.2
What About Using Dextrose Only
Theoretically, administering dextrose should stimulate insulin release and thereby lower serum potassium concentrations. Early reports recommend against this technique for 2 reasons.9
On the flip side, a randomized, crossover study was conducted in 10 chronic hemodialysis patients who were prone to hyperkalemia.10 Administration of 10 units of insulin with 100 mL of 50% glucose was compared with the administration of 100 mL of 50% glucose only. Infusion of a glucose-only bolus caused a clinically significant decrease in serum potassium by 0.5 mEq/L without any episodes of hypoglycemia. The insulin/glucose group saw a drop in potassium of 0.83 mEq/L at 60 minutes.
Bottom Line: Based on conflicting data, and considering that many patients have ESRD plus diabetes, this approach has potential but may not be ready for mainstream use. Also, hyperglycemia may be undesirable in some patients.
You May Like: How To Get Fasting Numbers Under 90 For Gestational Diabetes
Can Lactulose Be Used For Hyperkalemia
4.4/5Lactulosehyperkalemialactuloseused
Diarrhea may occur if the dose of lactulose is too high. Problems associated with diarrhea are fluid and potassium loss in the diarrheal stool leading to dehydration and low blood levels of potassium .
Also Know, does calcium bind to potassium? Calcium is given intravenously to protect the heart, but calcium does not lower the potassium level. Then insulin and glucose are given, which move potassium from blood into cells, thus lowering the potassium level in blood. Albuterol may be given to help lower the potassium level.
Moreover, how does albuterol work in hyperkalemia?
Albuterol is an adrenergic agonist that has an additive effect with insulin and glucose, which may in turn help shift potassium into the intracellular space. This agent lowers the serum potassium level by 0.5-1.5 mEq/L. It can be very beneficial in patients with renal failure when fluid overload is concern.
What is the emergency treatment for hyperkalemia?
Drugs used in the treatment of hyperkalemia include the following: Calcium : Reduces the risk of ventricular fibrillation caused by hyperkalemia. Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.
Study Selection And Outcomes
We considered articles to be eligible for inclusion if they reported on using insulin in the management of hyperkalemia. We included all study designs that used a standardized protocol except for case reports. We also excluded articles from further review if they fulfilled one or more of the following criteria: patients less than 18 years of age hyperkalemia that occurred in an operative setting and articles in which there were co-interventions for the management hyperkalemia .
Our primary outcome was the mean change in serum K+ concentration at 60 minutes after starting the administration of insulin.
You May Like: What Is A Good Score For Diabetes
Causes Of Hyperkalemia In Acutely Ill Patients
Factors associated with the development of hyperkalemia can be classified into three categories, and include altered renal clearance of potassium , release from the intracellular space and altered transfer to the intracellular space . Hyperkalemia in the patient with normal renal function is unusual and should prompt evaluation for pseudo-hyperkalemia if no ECG abnormalities consistent with hyperkalemia are identified . While concomitant medications are often a contributor to hyperkalemia, in our experience they are rarely the only cause in acute settings.
Table 1 Mechanisms contributing to the development of hyperkalemia
A special warning should be made with regards to the use of succinylcholine, classically used to induce paralysis in acutely ill patients for rapid sequence intubation. Succinylcholine induces skeletal muscle cell depolarization with an efflux of intracellular potassium by nicotinic receptor activation. In a population of critically ill patients, succinylcholine increased serum potassium on average 0.4 mmol/L . It should be avoided in patients with hyperkalemia and in patients with up-regulation of nicotinic receptors, as they are at risk of greater potassium elevation. This includes those with anatomical denervation, prolonged administration of neuromuscular blocking drugs, burn injury, and prolonged immobilization . Alternative to succinylcholine are available in patients at risk of hyperkalemia .
Insulin Mechanism Of Action In Hyperkalemia1415
Insulin causes an intracellular shift of potassium by stimulating Na+-H+antiporters, promoting sodium influx. Increased intracellular sodium concentrations trigger the activation of the Na+-K+ATPase transporter, which exchanges intracellular sodium for extracellular potassium. A dose of 10 units IV insulin regular has been estimated to lower serum potassium levels by 0.6 to 1.2 mEq/L in 1hour.16
Read Also: How To Cure Diabetes 2
When Do You Recheck Potassium After Hyperkalemia Treatment
After initial interventions, potassium should be rechecked within one to two hours, to ensure effectiveness of the intervention, following which the frequency of monitoring could be reduced. Subsequent monitoring depends on the potassium level and the potential reversibility of the underlying cause.
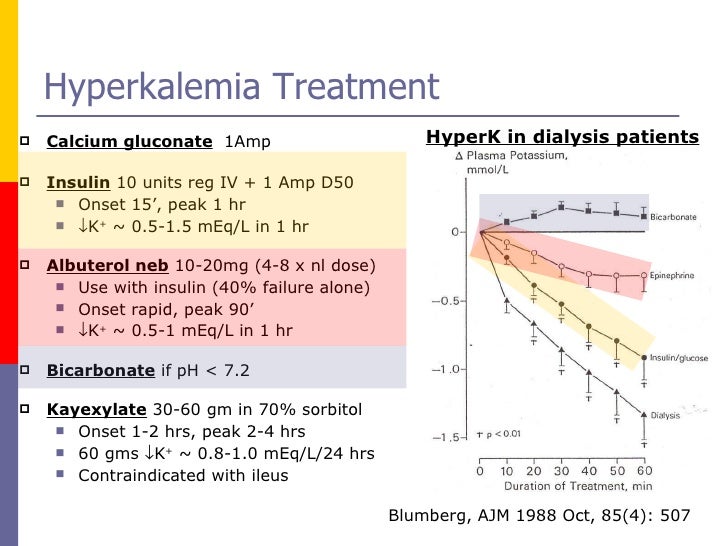
Medications In The Emergency Management Of Hyperkalemia
Three main principles
There are specific treatments geared at targeting each of these three main principles, which we will discuss below. Unfortunately, there is no clear evidence to guide exactly when to initiate specific treatments for hyperkalemia. Our experts recommend using two factors to guide your management:
with the following indications for immediate treatment of hyperkalemia in the ED:
Principle 1: Stabilize the cardiac membrane
There is no good literature to help guide whether calcium gluconate or calcium chloride is better for stabilizing the cardiac membrane in hyperkalemia. The most important difference to remember is that calcium chloride has 3 times more elemental calcium than calcium gluconate and has greater bioavailability. However, calcium gluconate has less risk of local tissue necrosis at the IV site. Therefore, if you decide to give calcium gluconate, ensure you are giving sufficient doses of calcium since one amp may not be enough. Three amps of calcium gluconate are often required to start to see the ECG changes of hyperkalemia resolve. Remember that calcium does not lower the potassium level.
Our experts recommend using calcium chloride through a large well-flowing peripheral IV or central line in the arrest or peri-arrest patient. Calcium gluconate is recommended for all other patients given its lower risk for local tissue necrosis.
Monitor glucose q30 minutes
Read Also: Type 2 Diabetes When To Take Insulin
Cautions With Iv Insulin
Hypoglycemia: One of the obvious labs that you must monitor very closely when administering IV insulin is the patient’s glucose. You would not want the patient to become hypoglycemic because too much insulin was administered. Patients may start getting sweaty, confused, feeling nauseous, begin shaking, or experiencing decreased level of consciousness when their blood sugar becomes too low.
Hypokalemia: A large cause of death in treatment of DKA patients is hypokalemia. There is an elevated serum potassium initially when patients are in a state of DKA. This quickly comes down as insulin is administered and the potassium shifts back into the cells. Hypokalemia can cause cardiac arrhythmias and death if left untreated.
Cerebral edema: Dropping a patient’s blood sugar too quickly can result in the development of cerebral edema. In a publication by Bohn & Daneman, they stated that “the osmolar gradient caused by the high blood glucose results in water shift from the intracelluar fluid to the extracellular fluid space and contraction of cell volume. Correction with insulin and intravenous fluids can result in a rapid reduction in effective osmolarity, reversal of the fluid shift and the development of cerebral edema.”
Other relevant articles include:
What Medications Are Used To Treat Hyperkalemia
treatmenthyperkalemiadrugtreatmenthyperkalemia
Drugs used in the treatment of hyperkalemia include the following:
- Calcium : Reduces the risk of ventricular fibrillation caused by hyperkalemia.
- Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.
Furthermore, how do you treat hyperkalemia?
Similarly one may ask, what are the drugs that reduce potassium?
- Diuretics. Diuretics like furosemide, bumetanide, hydrochlorothiazide, and chlorthalidone are the main medication-related cause of low potassium levels.
- Albuterol.
- Risperdal and Seroquel.
What potassium level necessitates urgent treatment for hyperkalemia?
A Hyperkalemia Emergency, which we define as a serum potassium> 6.0 meq/L or a sudden increase in serum potassium 1.0 meq/L above 4.5 meq/L within 24 hours associated with cardiopulmonary arrest, evolving critical illness, AMI, or signs and symptoms of neuromuscular weakness, should be treated with agents that
Read Also: Short Term Health Insurance For Diabetics
Severity & Risk Stratification
The first step of treatment requires determining whether hyperkalemia is life-threatening . No evidence-based definition for severe hyperkalemia exists. Clinical judgement is needed, with attention to the following factors:
- Potassium level: above 6.5-7 mM is more worrisome.
- Chronicity:
- Chronic hyperkalemia is better tolerated .
- Acute hyperkalemia is more dangerous.
Below is a consensus definition of severe hyperkalemia from a KDIGO conference. The European Resuscitation Council has similarly defined severe hyperkalemia as > 6.5 mM.
A Nurse’s Guide To Administering Iv Insulin
You have a patient that comes up to your unit with a blood sugar of 952. The labs are sent off and the patient is found to be in severe diabetic ketoacidosis .
The doctor puts in the orders for serial lab work, fluid boluses, electrolyte replacements, and an insulin drip. As a newer nurse, you are familiar with labs, boluses, your replacement protocols, but have never administered insulin through an IV. What nursing interventions do you need to perform to safely care for this patient?
Don’t Miss: How Can I Get Checked For Diabetes
How Does Insulin Work
Insulin is a hormone created by the pancreas. It allows your body to use glucose to provide the body’s cells with the necessary energy they need. Insulin production from the pancreas is based off of your blood sugar levels. If you are getting hyperglycemic, the pancreas is signaled and insulin is released into the bloodstream. Insulin then signals different cells to absorb the glucose and use it as energy or store it for later use.
When insulin facilitates glucose being pulled into a cell, a potassium cation is also pulled from extracellular fluid into the intracellular fluid. How does this affect our patients? Initially, patients in DKA have an increased extracellular potassium level due to the hyperglycemia and acidosis they are experiencing. This potassium level is quickly decreased as blood glucose is pulled into the cells.
Insulin Dosing Evaluation In Hyperkalemia
Several studies have compared insulin dosing strategies in hyperkalemia.8-10,13,18 These studies compared patients receiving 10 units to lower doses, such as 5 units or 0.1 unit/kg, and assessed for potassium-lowering ability and incidence of hypoglycemia.8-10,13,18 Hypoglycemia was generally defined as blood glucose less than 70 mg/dL however, there were varying definitions of severe hypoglycemia and duration of monitoring for hypoglycemia after insulin administration.8-10,13,18
Also Check: How To Prevent Yourself From Getting Diabetes
High Serum Potassium Levels
High serum potassium levels can be life-threatening and requires immediate therapy. There are several conditions which can significantly affect serum potassium levels and cause them to rise.
The amount of potassium in the blood determines the excitability of nerve and muscle cells, including the heart muscle or myocardium. When potassium levels in the blood rise, this reduces the electrical potential and can lead to potentially fatal abnormal heart rhythms.
What Are Dosages Of Dextrose
Dosages of Dextrose :
Dosage Considerations Should be Given as Follows:
Acute Alcohol Intoxication
- 25-50 g administer with thiamine to prevent Wernicke’s encephalitis
Sulfonylurea Overdose
- 10-25 g IV may require repeated boluses
Insulin Overdose
- 400-600 mg of glucose/kg/hour needed for most insulin overdoses
- Alternatively, administer 25-50 g IV may repeat doses in severe cases determine glucose levels before injecting dose in emergencies, may administer promptly before obtaining glucose results
Hyperkalemia
- 25-50 g plus 10 units regular insulin IV over 30-60 min
Insulin Induced Hypoglycemia
- Children under 6 months: 250-500 mg/kg/dose
- Children over 6 months: 0.5-1g/kg/dose
Recommended Reading: Why Does Diabetes Affect Feet
Risk Factors For Developing Hypoglycemia
The study by Apel et al identified 3 factors associated with a higher risk of developing hypoglycemia:
Renal dysfunction, in and of itself, may also be a risk factor for developing hypoglycemia. Some evidence suggests that insulin is metabolized by the kidneys to some extent. Furthermore, patients with acute kidney injury have clinically relevant changes in insulin metabolism, as evidenced by increased hypoglycemic events and lower insulin requirements upon developing AKI.6
A higher insulin dose caused more hypoglycemia .7
The 2018 study by Scott et al, identified that lower glucose prior to insulin , higher doses of insulin , and lower doses of D50 were independently associated with hypoglycemia in the multivariate analysis.5 Age, history of diabetes, and history of renal failure were not independently associated.
Emdocs Cases: Updates In Management Of Hyperkalemia
Authors: Brit Long, MD and Justin R. Warix, DO, FAAEM // Edited by: Alex Koyfman, MD Welcome back to emDocs Cases! Today we have case-based discussion on a core EM topic, with a look at some controversy and cutting edge treatments. – A 62-year-old female with history of renal disease on dialysis, hypertension, and CAD presents with nausea and weakness. She missed todays dialysis session. Her VS are normal, and her exam is also normal. Whats your first test you obtain? The ECG! You see large, peaked T waves with absence of P waves. The VBG returns with potassium of 7.3 mmol/L, with sodium 140 mmol/L and normal lactate. You ask for your standard hyperkalemia regimen, or C BIG K DROP see more from This regimen classically consists of Calcium , Beta agonist and/or Bicarbonate , Insulin , Kayexalate , Diuretics , and Renal unit for dialysis Of Patient. Whats the literature behind this regimen? Is there anything better? Before we start, lets cover some basics. Most potassium is intracellular , with 75% found in skeletal muscle. A significant gradient between the intracellular and extracellular environment plays a vital role in generation of cellular action potentials.1-5 The renal system plays the most important role in regulation of potassium . Normal levels are 3.5-5.0 mEq/L or mmol/L.1,2 Changes iContinue reading > >
- Managed Care Updates: Medicare and CGM, Omada Health Hires, Council for Diabetes Prevention Officers
You May Like: Type 2 Diabetes Is Caused By
Patients Without Risk Factors For Hypoglycemia After Insulin
If patients do not have any risk factors for hypoglycemia after insulin, no modification to traditional practice is needed. Some sources recommend holding dextrose if pre-treatment blood glucose is greater than 250 mg/dL.7 However, monitoring blood glucose every hour for 4 to 6 hours after insulin is still recommended regardless of the number of risk factors the patient has for hypoglycemia.
Role Of The Pharmacist
Pharmacists can play a vital role in the management of hyperkalemia. They should be aware of newly approved treatment options and can assist with dosing of the various medications used, as well as assess for drug-inducing hyperkalemia agents. Since management options for hyperkalemia have remained consistent for many years prior to the approval of patiromer, the only comparator of the newly approved agent was SPS. Although the data regarding efficacy were limited for SPS, it became a mainstay treatment option due to lack of alternatives. The 2015 approval of patiromer now adds another option for management of hyperkalemia in the outpatient setting. Neither patiromer nor ZS-9 replace current treatment approaches for hyperkalemia. ZS-9 may be beneficial as suppressive or preventive treatment in those with CKD.
Read Also: Does Water And Baking Soda Help Diabetes
Hyperkalemia Is The Great Ecg Imitator
These ECG findings are not specific to hyperkalemia alone. Given the broad differential for these ECG changes, hyperkalemia has been dubbed the Great ECG Imitator. It is important to consider the patients presentation, clinical complaints and trends on the ECG.
PEARL: Hyperkalemia has been known to cause almost any dysrhythmia. Pay special attention to patients in slow VT and wide-complex bradycardia and consider treating them empirically as hyperkalemia.
Medication Errors During Insulin Administration For Patients With Hyperkalemia
Hyperkalemia is a serious, potentially lethal electrolyte disturbance that requires medical treatment without delay if it is severe enough to cause disturbances in cardiac conduction. Although hyperkalemia treatment guidelines in the literature vary,1 many organizations begin treatment with the administration of one or more intravenous bolus doses of 50% dextrose and an IV bolus dose of 10 units of insulin. Some organizations use a rapid-acting insulin rather than short-acting insulin because it may decrease the incidence of hypoglycemia, given its shorter half-life.1
Don’t Miss: Is Type Two Diabetes Hereditary