What To Tell Patients On The Day They Start Insulin
Although everyone has different information needs, comprehensive information given when starting insulin may confuse many patients. They may not remember the more important messages and some may even be scared away from insulin treatment altogether. Our practice is to concentrate on teaching patients how to inject the insulin subcutaneously into the abdomen, using devices such as the FlexPen or InnoLet which are extremely user-friendly and can be taught in a matter of minutes.
The day patients start insulin is also not an ideal time for detailed dietary advice. We only emphasise the need to have regular meals and snacks containing carbohydrates.
At this stage of diabetes, most patients would be familiar with glucose monitoring and should be asked to perform this. As adjustment of insulin dosage in this regimen is primarily dependent on the morning fasting blood glucose concentrations, testing at this time point is the first priority and should be included every day. For some patients who cannot test their blood glucose for various reasons, it may be necessary to commence insulin without such monitoring and rely on blood glucose monitoring at the doctor’s office and HbA1c concentration to make dose adjustments.
> > > Discover The 1 Green Veggie That Worsens Diabetes Type 2 Symptoms
Diabetes can be managed through oral medications. In addition to insulin, metformin, which is a sugar-reducing agent, is also a common treatment for diabetes. It is considered a first-line therapy for diabetes treatment and is often added to insulin. It is important to know the risks of taking diabetes medications. Some drugs can be addictive, so you must consult your doctor before taking any medication. Your physician can prescribe you an appropriate treatment plan based on your medical history.
Your doctor will prescribe medication and check your blood glucose levels on a regular basis. Your A1c level will be checked every six months and your cholesterol levels will be tested regularly. Your doctor will also look for any signs of retinopathy, which is damage to the nerves in the eye caused by diabetes. You will also be examined for any foot problems. It is important to see a foot specialist regularly. Your feet should be thoroughly inspected for damage to the nerves.
While the first two types of insulin are the most common treatments, diabetes can be treated in a variety of ways. Your doctor may prescribe medications to control high blood pressure, which can protect the kidneys. Other types of medication include aspirin and other types of anti-platelet drugs. If your doctor is concerned about your blood sugar level, you may need to try a different medication. Some medications can cause side effects. Your treatment will depend on what type of insulin you need.
Titration And Timing Of Basal Insulin
After the recent unexpected finding of increased mortality in the intensive glucose-lowering therapy group of the ACCORD study, which might be partly related to the rate of the reduction in A1C , clinicians may now be more reserved to lower glucose levels promptly. However, we still feel that in addition to timely initiation, rapid titration of the dose is indispensable for successful insulin therapy. The ACCORD study solely included patients at high risk for cardiovascular disease, in whom low A1C levels were reached by using up to four or five different classes of glucose-lowering drugs. In contrast, in less selected patients treated with stable doses of one or two oral agents, simple titration algorithms targeting fasting plasma glucose 100 mg/dl can safely achieve A1C of 7.0% . A patient-driven algorithm, with patients increasing their insulin dose by 2 or 3 units every 3 days, as long as their fasting plasma glucose remains above target, constitutes a practical approach that has been shown to be equally or more effective than physician-led titration .
Recommended Reading: Cold Medicine For Diabetics With High Blood Pressure
Making The Switch To Insulin
Making the transition is much easier than it used to be because most patients are started on a long-acting insulin that does not need to be matched with food intake.
Insulin pens that are preloaded are replacing insulin that needs to be drawn up into a syringe. Patients may still be worried about giving themselves injections, but because the needle is so tiny the adjustment is often quick.
Toujeo and Lantus are long-acting forms of insulin that are available in a prefilled injectable pen.
There’s also a type of rapid-acting insulin, Afrezza, that can be inhaled through the mouth via an inhaler.
And a new class of medication called sodium-glucose cotransporter 2 inhibitors is also available now, according to Mazhari. “It works via a different pathway that’s not pancreas-dependent, offering another medical therapy option for patients with type 2 diabetes.”
The key to an easy transition to insulin is education.
“Patients need to know how to take their insulin properly since there are many formulations on the market, including short- and long-acting insulin and premixed,” Mazhari said. “Most can be started on a long-acting insulin once a day, though for some patients short-acting or mealtime insulin may be necessary as well. Insulin doses need to be further adjusted depending on blood sugar readings.”
Do Tell Friends And Family That Youre Taking Insulin

Its a good idea to teach your friends, colleagues, and family members about insulin and its potential side effects. If you do end up taking too much insulin and having a hypoglycemic episode, they should know how to help.
If you become unconscious, a friend or family member can give you a shot of glucagon. Talk to your doctor about keeping a supply of glucagon on hand and learning when and how to use it.
Recommended Reading: When You Have Type 2 Diabetes
Other Options For The Initiation Of Insulin Therapy
The recent Treating to Target in type 2 Diabetes study compared the introduction of basal insulin at bedtime to insulin initiation with either biphasic insulin twice daily or prandial insulin before meals . The biphasic and prandial insulin regimens provided better glycemic control than once-daily basal insulin but at the expense of increased risks of hypoglycemia and weight gain. Although biphasic insulin reduced A1C levels to the same extent as prandial insulin, the latter regimen was associated with the most hypoglycemic episodes and the highest weight gain . Therefore, and considering that to date there is no clinical trial evidence supporting the specific lowering of postprandial glucose levels when aiming to lower cardiovascular risk in type 2 diabetes, initiation with prandial insulin is generally not a first-choice approach when starting insulin in type 2 diabetic patients. This was confirmed by a recently reported direct comparison of once-daily insulin glargine versus thrice-daily insulin lispro in insulin-naive patients . Finally, also regarding feasibility in clinical practice and patients’ acceptance, three injections per day is the least attractive option for initiation of insulin therapy.
Common Questions About Type 2 Diabetes:
- Can type 2 diabetes go away?
- Will I need to take insulin?
- Do I have to take it forever?
How do you treat type 2 diabetes?
When you have type 2 diabetes, you first need to eat a healthy diet, stay physically active and lose any extra weight. If these lifestyle changes cannot control your blood sugar, you also may need to take pills and other injected medication, including insulin.
Eating a healthy diet, being physically active, and losing any extra weight is the first line of therapy. Diet and exercise is the foundation of all diabetes management because it makes your bodys cells respond better to insulin and lowers blood sugar levels.
If you cannot normalize or control the blood sugars with diet, weight loss and exercise, the next treatment phase is taking medicine either orally or by injection.
Diabetes pills work in different ways some lower insulin resistance, others slow the digestion of food or increase insulin levels in the blood stream. The non-insulin injected medications for type 2 diabetes have a complicated action but basically lower blood glucose after eating. Insulin therapy simply increases insulin in the circulation.
Many people with type 2 diabetes have elevated blood fats and blood pressure, so you may be given medications for these problems as well.
Can type 2 diabetes go away? And if my blood sugar becomes normal, do I still have diabetes?
Will I need to take insulin if I have type 2 diabetes?
Read Also: Whats A Good A1c For A Type 2 Diabetes
What Is Insulin Made Of
Insulin is made in different ways. You and your healthcare team will discuss which insulin you can take.
- Human insulin this is synthetic and made in a laboratory to be like insulin made in the body.
- Analogue insulin the insulin molecule is like a string of beads. Scientists have managed to alter the position of some of these beads to create genetically engineered insulin known as analogues.
- Animal insulin This isnt used much anymore, but some people find that insulin from animals works best for them. It is usually from a cow or pig.
Insulin Treatment In Type 2 Diabetes
The decision to take insulin is never an easy one. For many patients, it comes after years of having type 2 diabetes and trying multiple weight-loss regimens, diets, and oral medications. For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control with other drugs.
The good news is that insulin almost always works. Daily injections, however inconvenient or painful at first, can be very effective at controlling blood glucose. Anxious about giving injections? Help is available. If your health care provider prescribes insulin, a trained diabetes educator or pharmacist can teach you how to measure out the proper dose and administer your daily injections.
Why should I use insulin?
With type 2 diabetes, over time, the pancreas is often unable to produce insulin on its own. When that happens, your blood glucose levels will become very difficult to control without daily injections of insulin. Injectable insulin is identical to the insulin made by the body, but can be categorized into two main types: basal insulin keeps your blood glucose stable all day long, even when not eating, while bolus insulin helps your body respond to the quick rise in blood glucose after meals.
Also Check: Free Stuff For Type 1 Diabetes
When Should Insulin Therapy Be Initiated
Type 2 diabetes is a progressive disease, and thus, ultimately this question will arise for many of our patients. Unfortunately, there is no unequivocal answer, which was nicely illustrated by a recent interactive case vignette. The polling results demonstrated once again that the management of patients with type 2 diabetes uncontrolled by two oral glucose-lowering agents is controversial. Furthermore, the preferred treatment option was found to be related to the respondents’ locations and self-reported specialties .
Too Much Insulin Or Not Enough
High morning blood sugar levels before breakfast can be a puzzle. If you haven’t eaten, why did your blood sugar level go up? There are two common reasons for high before-breakfast blood sugar levels. One relates to hormones that are released in the early part of sleep . The other is from taking too little insulin in the evening. To see which one is the cause, set your alarm to self-monitor around 2 or 3 a.m. for several nights and discuss the results with your health care provider.
Also Check: What Happens When You Take Insulin
How Much Insulin And At What Time
For practical purposes, the patient can always be commenced on 10 units of intermediate-acting insulin, given just before bedtime and as late as possible. This timing allows the insulin to exert its maximum action just before dawn rather than at 2-3 a.m. when it is most likely to cause hypoglycaemia. If the patient is very nervous or reluctant and it is imperative to minimise the risk of hypoglycaemia, however small, then a slightly lower dosage can be used to get the process underway and to gain the patient’s confidence. Patients who have symptoms of hyperglycaemia can start at a higher dose of insulin, but this would rarely need to exceed 20-25 units.
The bedtime dose of insulin is best given as isophane insulin. Currently in Australia, there is only one brand of human isophane insulin available. When it becomes generally available, insulin glargine will probably become the basal insulin of choice as its ‘flatter’ and longer action make it more suitable for this purpose.3
Insulin For People With Type 2 Diabetes
Insulin is a hormone produced by your pancreas. Often referred to as the most powerful hormone in the human body, we all need insulin to live. Without enough insulin, your body cannot use the sugar in your bloodstream for fuel. Without enough insulin, your the amount of sugar in your bloodstream can rise to above-normal levels that threaten your short-term and long-term health.
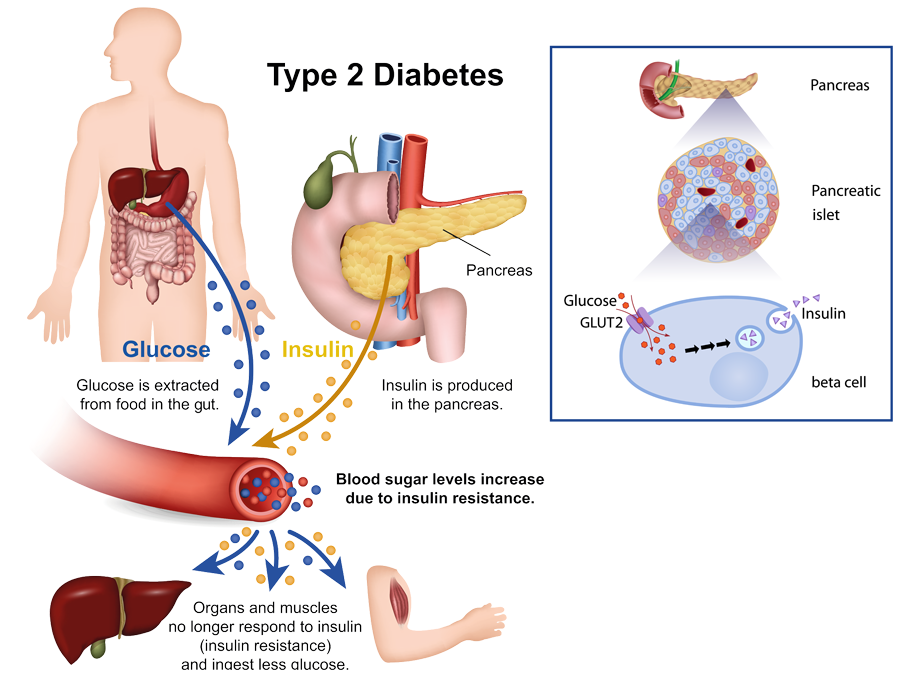
In people with Type 2 diabetes, your body is struggling with two things that can lead to high blood sugar levels:
- Insulin resistance: This is when your body isnt responding to normal amounts of insulin and isnt able to use that insulin effectively to manage your blood sugar levels. Some insulin resistance can be improved through lifestyle changes . For some people, insulin resistance is a deeper issue that cannot always be easily changed. This means you may need support from diabetes medications or insulin to help you manage healthy blood sugar levels.
- Beta-cell dysfunction: This is when your body struggles to produce normal amounts of insulin. Beta-cells are produced by the pancreas, then those cells produce insulin. In many people with Type 2 diabetes, your body struggles to produce normally functioning beta-cells which means you dont produce enough insulin. This can worsen over time, and your body is able to produce less and less insulin over time. This means youll need more support from diabetes medications or insulin to help you manage healthy blood sugar levels.
Don’t Miss: How To Control Pre Diabetic Condition
How To Titrate Insulin Dosage And Monitor Progress
A major feature of this regimen is that insulin is added to existing treatment. Glycaemic control should therefore improve immediately and for practical purposes, should not deteriorate. This means that the dose of insulin can be increased relatively slowly, minimising the risk of hypoglycaemia. As described originally, the regimen2 increased the insulin dosage by 4 units a day if the fasting blood glucose exceeded 8 mmol/L on three consecutive days and by 2 units a day if it exceeded 6 mmol/L. We tend to do it slightly slower and adjust insulin dosage according to these glucose thresholds every 1-2 weeks. The slower pace helps to gain the patient’s confidence and reduces the risk of hypoglycaemia. This titration regimen is of course not ‘cast in stone’ and there are ongoing trials that are exploring the best options.
After 2-3 months, the patient is likely to be on about 30 units of insulin each day and maximum oral drug therapy. Measuring the HbA1c concentration after this interval helps to quantify the new level of glycaemic control and further increases in insulin dosage can be made accordingly. There is generally a reduction in HbA1c of about 2% and an increase in body weight of several kilograms. If these changes are not evident, one should consider the possibility that the patient has not been taking the insulin regularly or someone unfamiliar with the regimen has reduced or stopped one or more of the oral hypoglycaemic drugs.
How To Reverse Insulin Resistance
If you have insulin resistance, you want to become the oppositemore insulin sensitive .
Physical activity makes you more sensitive to insulin, one reason why its a cornerstone of diabetes management . Dont wait until youre diagnosed with diabetes to start moving more. The earlier you take action , the better off youll be.
Weight loss is important too, as is avoiding high blood sugar, reducing stress, and getting enough sleep .
These lifestyle changes really work. Talk with your health care provider about how to get started.
Read Also: Can I Buy A Diabetes Test Kit
How Is Insulin Used
Most people use insulin as an injection, or shot. It is given into the fatty tissue just under the skin. Learning how to give yourself insulin may take some time. You’ll also need to pay more attention to your blood sugar levels than you may be used to. But with practice, monitoring your levels and using insulin correctly can become a routine part of your day.
The Future Of Insulin
More insulin advances are percolating. There will be new insulins that act even faster. Improvements will be made in the open-loop pumps currently on the market, and efforts continue to develop the so-called artificial pancreas, or closed-loop system that promises, with several different models, to control blood sugar without the person having to do all the thinking.
Work also progresses on alternate ways to take insulin. The second generation of inhaled insulin is on the way with the FDA’s approval of Afrezza in 2014. Investigation is ongoing for delivering insulin buccally — via the tongue, throat, and cheeks — or through a skin patch.
While the progress on new insulin products and delivery systems is encouraging, don’t delay starting insulin if your health care provider and your diabetes health status indicate you need it now. The insulin available today is safe and relatively easy to take, and injections are nearly painless. Plus, starting to take insulin sooner rather than later may improve your health quickly and make your life better for many years to come.
Recommended Reading: Can You Control Type 2 Diabetes
Type 2s: Time For Insulin
Type 2s: Time For Insulin?
Another effective option would be to use an insulin PUMP. Insulin pumps are beeper-sized and battery-operated. They deliver tiny pulses of rapid acting insulin throughout the day and night, which effectively serves as the & ldquo basal& rdquo insulin. The user programs a larger dose, called a & ldquo bolus& rdquo dose, to be delivered at meal and snack times. The insulin is delivered from the pump into a small plastic tube that sits just below the skin.In order to cut down on the number of injections required with MDI or the complexity of using an insulin pump, some people opt to use PREMIXED insulin. Premixed insulin usually consists of intermediate insulin known as NPH combined with rapid insulin. Taken at breakfast and dinner, premixed insulin provides some basal insulin throughout the day and night and rapid insulin to offset breakfast and dinner.