Diagnosis And Ancillary Testing/differential Diagnosis
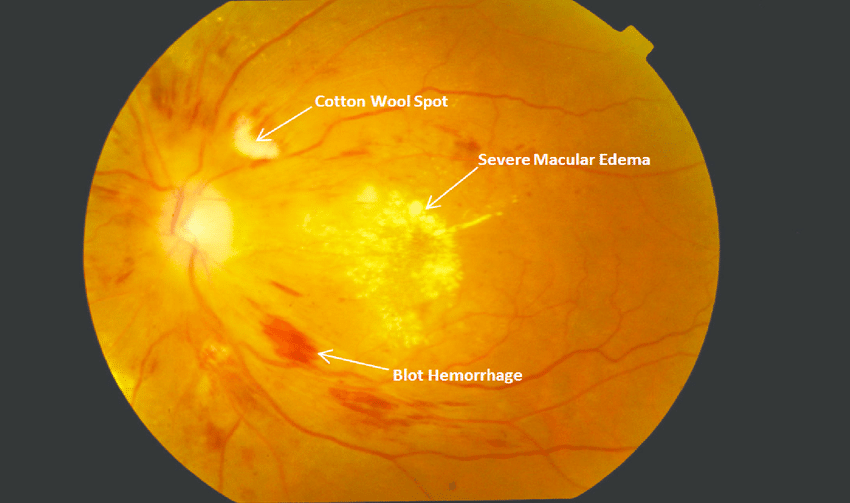
DR is diagnosed clinically on the basis of visible hemorrhages, microaneurysms, cotton wool spots, lipid exudates, and neovascularization. Fundus photography and fluorescein angiography have greater sensitivity than ophthalmoscopy because of superior optics, the enhanced contrast of fluorescein angiography, confirmation of vascular leakage, and the ability of the observer to review magnified images without the interference of patients moving or blinking.
How Is Diabetic Eye Disease Diagnosed
If youve ever had a comprehensive eye exam, youll find that many of the same tests are used for diabetic eye disease, plus some amazing new technology that has significantly advanced diagnosis and treatment protocols. If you dont have a regular eye doctor, ask your primary care provider or endocrinologist to recommend one who regularly treats diabetic eye disease. A doctor of optometry is like a primary care physician for your eyesthey can examine, diagnosis and treat a variety of common vision issues. An ophthalmologist, however, is a medical doctor who specializes in the eye, performs eye surgery, and treats more serious eye diseases. An ophthalmologist especially one who is a retina specialist and therefore highly trained in treating diabetic eye diseasewill have the most experience with treatments and more sophisticated diagnostic tests that allow them to monitor the changes in the retina over time. Heres what to expect:
Related Conditions And Causes Of Diabetic Macular Edema
Some conditions closely related to diabetic macular edema include:
The NIHs National Eye Institute provides detailed educational materials for different types of eye diseases and conditions. From fact sheets to webinars, their resources can help you learn more about diabetic eye diseases and how to lower your risk of vision loss.
The ADAs mission is to prevent and cure diabetes and improve the lives of all people affected by the disease. Their site offers useful information about diseases that affect vision as well as stories from patients who are living with diabetes-related eye conditions.
Prevent Blindness is an organization with a mission that echoes its name: to prevent blindness and preserve sight. We especially like their Resources for Low Vision page, which provides links to financial assistance sites, doctor searches, assistive technology products, and more.
Don’t Miss: How To Count Carbs For Type 1 Diabetes
Causes & Risk Factors
Diabetic retinopathy results from the damage diabetes causes to the small blood vessels located in the retina. These damaged blood vessels can cause vision loss:
- Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
- In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
Diabetic retinopathy is classified into two types.
How Will My Eye Doctor Check For Diabetic Retinopathy

Eye doctors can check for diabetic retinopathy as part of a dilated eye exam. The exam is simple and painless your doctor will give you some eye drops to dilate your pupil and then check your eyes for diabetic retinopathy and other eye problems.
If you have diabetes, its very important to get regular eye exams. If you do develop diabetic retinopathy, early treatment can stop the damage and prevent blindness.
If your eye doctor thinks you may have severe diabetic retinopathy or DME, they may do a test called a fluorescein angiogram. This test lets the doctor see pictures of the blood vessels in your retina.
Recommended Reading: How Long Does Thc Stay In A Diabetics System
What Are Diabetic Retinopathy And Diabetic Macular Edema
Nearly 8 million Americans are affected by DR, which may result in problems with vision. DME is related to DR and also causes vision problems.
-
DR and DME damage the retina , the lightsensitive part in the back of your eye that gathers images
-
DME occurs when DR affects the macula . The macula is a small indent on the retina that helps you see fine details
- If you have uncontrolled high blood sugar from diabetes, it is important to pay careful attention to your sugar levels and any problems with vision you may experience
- In DR and DME, uncontrolled high blood sugar may damage the parts of the eye that allow you to see, leading to problems with vision
Progression And Regression Of Dr
A large number of cohort studies have investigated progression and regression of DR . Disease severity was most often classified by the Early Treatment Diabetic Retinopathy Study classification for DR severity . The cohort with the longest follow-up time was the WESDR cohort, which reported 25-year progression of DR in patients with type 1 diabetes . In this study, DR severity was assigned a level by concatenating the severity grade in both eyes, with the worse eye given greater weight. This created a 15-step scale, and progression was defined as increase in severity of 2 steps or more. Some other studies assigned DR severity based on the severity grade in the worse eye alone. The findings on DR progression and regression from the various cohort studies are summarized in Table . Four to six-year cumulative incidence of 2-step progression among the studies ranged from 24.1 to 38.9 %, which increased to 64.1 and 83.1 % in studies with 16-year or 25-year follow-up.
Read Also: Does Viagra Work For Diabetics
Other Types Of Diabetic Eye Disease
Diabetic retinopathy is the most common cause of vision loss for people with diabetes. But diabetes can also make you more likely to develop several other eye conditions:
- Cataracts. Having diabetes makes you 2 to 5 times more likely to develop cataracts. It also makes you more likely to get them at a younger age. Learn more about cataracts.
- Open-angle glaucoma. Having diabetes nearly doubles your risk of developing a type of glaucoma called open-angle glaucoma. Learn more about glaucoma.
Prevention Of Diabetic Macular Edema
- Maintaining good blood sugar control
- Keeping blood pressure and cholesterol levels in check
- Receiving a comprehensive eye exam at least once a year
- Following a healthy lifestyle that includes regular exercise and a nutritious diet
Regular eye exams and screenings are extremely important for people at risk for diabetic macular edema because symptoms dont always show up.
Recommended Reading: Does Medicare Cover Diabetic Testing Supplies
What Can I Do To Prevent Diabetic Retinopathy
Managing your diabetes is the best way to lower your risk of diabetic retinopathy. That means keeping your blood sugar levels in a healthy range. You can do this by getting regular physical activity, eating healthy, and carefully following your doctors instructions for your insulin or other diabetes medicines.
To make sure your diabetes treatment plan is working, youll need a special lab test called an A1C test. This test shows your average blood sugar level over the past 3 months. You can work with your doctor to set a personal A1C goal. Meeting your A1C goal can help prevent or manage diabetic retinopathy.
Having high blood pressure or high cholesterol along with diabetes increases your risk for diabetic retinopathy. So controlling your blood pressure and cholesterol can also help lower your risk for vision loss.
What Causes Diabetic Macular Edema
Diabetes is a leading cause of blindness and nearly 10% of diabetics may experience DME.3 DME can develop in people with type 1 or type 2 diabetes. The condition can progress slowly and generally makes it difficult to focus.
There are multiple contributing factors for developing DME. People with diabetes having one or more of the following are at increased risk for developing DME2,3:
- Living with diabetes for 20+ years
- Poor glucose control
Recommended Reading: Advanced Diabetes Supply Freestyle Libre
Risk Factors For The Occurrence And Progression Of Diabetic Retinopathy
The type of diabetes influences the occurrence and progression of diabetic retinopathy. In persons with inadequately controlled type 1 diabetes, proliferative retinopathy can arise as early as 10 years after diagnosis. In type 2 diabetes, the risk of macular edema is somewhat higher. In the prospective CALDIRET study, 635 persons with type 2 diabetes and mild, non-proliferative diabetic retinopathy were enrolled after a follow-up interval of up to five years, proliferation was present in only three eyes , but clinically significant macular edema was present in 155.
The sex of the patient also plays a role. The overall risk of blindness is nearly twice as high in women, and women are also more likely than men to have diabetes. Thus, according to the statistics of the statutory health carriers in the German state of Hesse for the year 2004, 55% of all diabetics covered by statutory health insurance were women. A study carried out by the Marburg University Department of Ophthalmology revealed that, in 1997 and 1998, 446 women and 233 men with diabetes in the state of Hesse were blind or severely visually impaired . Pregnancy can lead to progression of diabetic retinopathy.
Sex-specific risk
Women are twice as likely to go blind from diabetic retinopathy. Pregnancy can lead to progression of diabetic retinopathy.
Risk factors
-
Poor glycemic control
-
Arterial hypertension
Cataract surgery as a risk factor
All About Diabetic Macular Edema

Diabetic macular edema is extremely common in people with diabetic retinopathy. These two eye conditions are the leading cause of blindness in developed countries across the globe.
DME often goes hand-in-hand with retinopathy. In the later stages of retinopathy, DME is almost always present, but research has found it may start developing much sooner but goes undetected in these earlier stages.
Recommended Reading: My Husband Has Diabetes Erectile Dysfunction
What Causes Diabetic Eye Disease In The First Place
To understand how diabetic retinopathy and DME develop, lets take a peek into the anatomy of the eye. At the front of your eye is the clear dome-shaped portion known as the cornea, which covers your iris and the pupil . Directly behind the pupil is the lens. Light enters the eye through the cornea and travels to the lens, which focuses the light to the back of the eye and the nerve-packed retina. The retina then sends messages via the optic nerve to the visual cortex of the brain. Within the retina is a specialized area known as the macula, which helps you see fine detail.
Diabetic retinopathy occurs when the tiny blood vessels in the eye become damaged by the high sugar levels hanging out in them and begin to leak fluid, blood, or lipid deposits into the retina. In turn the retina swells, preventing the cells from sending accurate images to the brain. DME is when the leaking and swelling also occurs in the macula, furthering impairing vision . Think of it this way: The blood vessels in the eye are normally like a strong impermeable piece of PVC pipe, but when theyre constantly filled with sugar, the pipe begins to rust and corrode, springing leaks like a soaker hose in a garden.
What Is Diabetic Retinopathy With Macular Edema
What is diabetic retinopathy with macular edemaDiabetic retinopathy is an eye disease caused by diabetes.Diabetes can affect your eye care, making it especially important to get a regular eye exam.Damaged blood vessels and abnormal new ones can cause vision loss. In this article:
These conditions include diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma. Over time, diabetes can cause damage to your eyes that can lead to poor vision or even blindness. But you can take steps to prevent diabetic eye disease, or keep it from getting worse, by taking care of your diabetes.
Work with your diabetes doctor to determine if there are ways to improve your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can usually slow the progression. Advanced diabetic retinopathy. If you have proliferative diabetic retinopathy or macular edema, youll need prompt treatment.
Short description: Type 2 diabetes w unsp diabetic retinopathy w macular edema The 2022 edition of ICD-10-CM E11.311 became effective on October 1, 2021. This is the American ICD-10-CM version of E11.311 other international versions of.
Group ETDRSR. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema: Early Treatment Diabetic Retinopathy Study report number 2. Ophthalmology 94, 761774 .
Recommended Reading: I Need Help With My Diabetes
What Is The Best Treatment For Diabetic Macular Edema
Argon laser photocoagulation has been the mainstay of treatment for macular edema since the publication of the results of the Early Treatment Diabetic Retinopathy Study, which showed an approximate 50% reduction in the rate of moderate vision loss at 3 years following laser photocoagulation compared to no treatment.
Whats The Treatment For Diabetic Retinopathy And Dme
In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months.
In later stages, its important to start treatment right away especially if you have changes in your vision. While it wont undo any damage to your vision, treatment can stop your vision from getting worse. Its also important to take steps to control your diabetes, blood pressure, and cholesterol.
Injections. Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help.
You May Like: Long Acting Insulin Side Effects
Progression Of Diabetic Macular Edema
DME can happen at any stage of diabetic retinopathy. Itâs possible to have mild diabetic retinopathy and severe DME. Thereâs no timeframe for how long it might take for DME to become serious or a scale to measure its progression. In general, your doctor will watch out for two things during eye exams: the level of swelling and where itâs located.
Treatment Of Diabetic Retinopathy And Macular Edema
Diabetic retinopathy is damage to the light-sensitive retina in the back of the eye caused by type 1 or type 2 diabetes.
Chronic high blood sugar levels from the disease damage tiny blood vessels in the retina, causing them to leak fluid or blood into the retinal tissues. Damages to retinal blood vessels also causes bleeding into the posterior chamber of the eye that contains the normally clear vitreous gel.
Eventually, these changes cause irreparable damage to the retina and leads to vision problems that cannot be corrected with eyeglasses or contact lenses.
Diabetic retinopathy is associated with the proliferation of a protein called vascular endothelial growth factor in the retina.
VEGF stimulates the production of new blood vessels in the retina to bring more oxygen to the tissue because retinal blood circulation is inadequate due to diabetes.
Unfortunately, these tiny new blood vessels that form in the retina in response to VEGF are fragile and increase in number, leading to additional fluid leakage, bleeding and scarring in the retina and progressive vision loss.
Blood vessel leakage from diabetic retinopathy can cause fluid to accumulate in the macula, which is the most sensitive part of the retina that is responsible for central vision and color vision.
This condition called diabetic macular edema is the primary cause of vision loss associated with diabetic retinopathy.
Read Also: Where Is The Best Place To Inject Insulin
Top Suggestions For What Is Diabetic Retinopathy With Macular Edema
The American Journal of Ophthalmology is a peer-reviewed, scientific publication that welcomes the submission of original, previously unpublished manuscripts directed to ophthalmologists and visual science specialists describing clinical investigations, clinical observations, and clinically relevant laboratory investigations. More
How Is Diabetic Retinopathy Treated
Treatment for diabetic retinopathy will depend on your symptoms, age and general health. It will also depend on how severe the condition is.
People with advanced retinopathy have a good chance of keeping their vision if they are treated before the retina becomes severely damaged. Treatment for diabetic retinopathy may include one or a combination of the following:
- Laser surgery. This is often used to treat proliferative retinopathy and sometimes macular edema. It involves shrinking the abnormal blood vessels, or sealing the leaking ones.
- Vitrectomy. Vitrectomy is a procedure that involves removing the jelly-like substance that fills the center of the eye. The vitreous is replaced with a balanced saline solution.
- Injections. Certain medications can be injected into the eye to slow the growth of the abnormal vessels of the retina and to treat macular edema.
Also Check: Walmart 70 30 Insulin Pen
Injections To Treat Diabetic Retinopathy And Diabetic Macular Edema
If you have diabetic macular edema or an advanced case of diabetic retinopathy, your doctor may use injections as part of your treatment plan. You may need other treatments, like laser treatments or surgery, in addition to injections.
When you get injections in your eye, your eye doctor will:
- Put numbing medicine on your eye to make you more comfortable during the injection
- Clean your eye to help prevent infections
- Put the medicine in your eye with a very small needle
After the treatment, you may need to use antibiotic eye drops to keep your eyes from getting an infection. The treatment doesnt change your vision right away. Most people can go back to their normal activities right after the treatment.
Can You Have Diabetic Macular Edema Without Diabetic Retinopathy
No. DME is a complication of diabetic retinopathy, so youll have both if you have DME. You can have diabetic retinopathy without DME, though.
That said, diabetic retinopathy isnt the only cause of macular edema. Even people without diabetes can get macular edema from:
- complications of eye surgery for cataracts, glaucoma, or retina diseases
- age-related macular degeneration
Don’t Miss: Best Type 2 Diabetes App
What Are The Symptoms Of Diabetic Retinopathy
The early stages of diabetic retinopathy usually dont have any symptoms. Some people notice changes in their vision, like trouble reading or seeing faraway objects. These changes may come and go.
In later stages of the disease, blood vessels in the retina start to bleed into the vitreous . If this happens, you may see dark, floating spots or streaks that look like cobwebs. Sometimes, the spots clear up on their own but its important to get treatment right away. Without treatment, the bleeding can happen again, get worse, or cause scarring.
Treatment For Diabetic Macular Edema
The treatment plan for DME will depend on the severity of the condition, but there are two things everyone with DME can work on immediately after their diagnosis:
- Work with your healthcare team to bring your blood sugar levels and A1c into a safer range.
- Work with your healthcare team to lower your blood pressure levels.
Then, youll discuss the following treatment options with your eyecare team.
Read Also: How To Lower High Blood Sugar Without Insulin