What Else Can I Do To Manage My Blood Glucose Levels
Food, sleep, and exercise are all of vital importance for regulating your blood sugar when you have diabetes.
Get enough sleep. Evidence shows that lack of sleep can lead to increased secretion of the hormone cortisol, which is inflammatory and can cause greater insulin resistance. Endocrinologist Al Powers MD of Vanderbilt University notes that when youre deprived of sleep or your sleep is disrupted, your glucose levels tend to go up, whether you have diabetes or not.
Exercise regularly. During exercise, insulin sensitivity is increased, and muscle cells use available insulin more efficiently. When your muscles contract during exercise, they also absorb glucose and use it for energy.
Follow an eating pattern that is healthful for you, as recommended by your doctor, such as the DASH diet or the Mediterranean diet. Both have been shown to help stabilize blood sugar levels.
The End: Insulin Degradation In The Kidney
Insulin is no longer detectable in the circulation 30 min after its release from the pancreas, and its half-life once in the circulation is 6 min . In addition to its clearance by the liver , the hormone is also slowly internalized by most cells, including myoblasts and adipocytes, where it is routed to the lysosome for degradation. This is a mechanism to end insulin action, but it accounts for the destruction of only a fraction of the circulating insulin. The brunt of the degradation of the circulating hormone remaining after second pass through the liver occurs when it reaches the kidney. Here, its fate is threesome. Upon filtration at the level of the glomeruli, insulin enters the luminal space and reaches the proximal tubule, from whence it is rapidly reabsorbed by the renal epithelial cells. This reabsorption involves saturable binding to low-affinity, high-capacity sites at the brush border membrane, which are demonstrated to be not the IR but possibly scavenger receptors such as megalin and cubilin, proteins that recover a number of proteins by endocytosis. Insulin thus internalized enters the retroendocytic pathway, where it dissociates from its binding sites to proceed to lysosomes for degradation.
The 4 Different Types Of Insulin
At this time, insulin therapy involves the use of four primary types of insulin differentiated by how rapidly the effect of insulin sets in, when the effect reaches its peak, and how long the effect lasts.
The four types are:
Per information provided by the American Diabetes Association, the first type, rapid-acting insulin, can be detected in the bloodstream within 15 minutes of injection, reaches peak concentrations in the blood between 30 and 90 minutes, and continues to be detectable for approximately 5 hours.
Short-acting insulin can be detected within 30 minutes, reaches peak concentrations about 2 to 4 hours after injection, and remains present for between 4 and 8 hours.
Intermediate-acting insulin reaches the bloodstream between 2 and 6 hours after injection, peaks between 4 and 14 hours after, and stays in the blood for around 14 to 20 hours.
Long-acting insulin does not reach the bloodstream for 6 to 14 hours, reaches peak concentrations shortly after, and remains in the blood for between 20 hours and a full day.
Every diabetic has individual insulin needs and responses, and there’s no single type that’s universally best. Rather, it’s important to tailor insulin therapy to a patient’s specific needs. It’s even possible to use two types mixed together to access a range of different delivery times, peaks, and durations.
You May Like: What Is The Least Expensive Long Acting Insulin
Central Insulin Action: Brief Focus On The Brain
Emerging from the circulation, insulin begins its multifaceted action on central and peripheral tissues. As outlined above, insulin crosses the bloodbrain barrier through a receptor-mediated process . Thought to be insulin unresponsive in the past, the central nervous system is well recognized to be exquisitely responsive to the incoming hormone . The concentration of insulin in the cerebrospinal fluid is one third that in the circulation, but it nonetheless fluctuates according to the latter and acts on IR on neurons and glial cells. Notable among the evoked central functions is the regulation of appetite and energy expenditure . Insulin regulates appetite by reducing expression of neuropeptide Y and Agouti-related peptide and, conversely, elevating expression of pro-opiomelanocortin . Insulin also exerts trophic and developmental actions on neurons and glial cells, and new evidence suggests it modulates cognition, memory, and mood . Conversely, central defects in insulin action are emerging as a potential contributor to the development of Alzheimers disease , possibly as a result of abnormal phosphorylation of tau protein . Insulin acting centrally also evokes efferent inputs into peripheral tissue metabolism , contributing to the suppression of gluconeogenesis in the liver and the counterregulatory response to hypoglycemia . Acting centrally on IR, insulin contributes to thermoregulation by activating heat-liberating mechanisms in brown adipose tissue .
What Is The Function Of Glucagon
Your body normally carefully regulates your blood glucose primarily with the hormones glucagon and insulin. When your blood glucose levels trend lower or fall too low , your pancreas releases more glucagon. Glucagon helps blood glucose levels rise back up in multiple ways, including:
- Glucagon triggers your liver to convert stored glucose into a usable form and then release it into your bloodstream. This process is called glycogenolysis.
- Glucagon can also prevent your liver from taking in and storing glucose so that more glucose stays in your blood.
- Glucagon helps your body make glucose from other sources, such as amino acids.
If your blood glucose levels trend higher, your pancreas releases insulin to bring it back into range.
Read Also: Continuous Glucose Monitoring For Dogs
Other Functions Of Insulin
- Regulating the activity of various enzymes and their effects in the body
- Following illness or injury, muscles get weakened or there is damage to muscle tissue. That is when insulin transports amino acids absorbed from the food we consume to the concerned muscles so that they regain their strength and size .
- DNA replication and synthesis of proteins
- Absorption of potassium by body cells
- Manage removal of excess sodium from the body
- Maintaining fluid volume in the urine
- Enhance cognitive functions such as learning and memory. Insulin reserves a certain amount of blood-sugar for this, all the time.
What Happens If I Have Too Little Insulin
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies , hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels. If the glucose level is high enough, excess glucose spills into the urine. This drags extra water into the urine causing more frequent urination and thirst. This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy are needed to provide this energy. This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products. Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
You May Like: Best Low Carb Diet For Diabetics
Regulates Blood Sugar Levels
The most crucial role of insulin in the human body is, that it helps to regulate blood sugar levels. It interacts with glucose to enter human cells to produce energy for the body. The pancreas is the vital reason for the production of insulin hormones. Insulin helps to open the body cells and use that as a source of energy.
When To Contact A Medical Professional
- Shortness of breath
- Red, painful skin that is spreading quickly
These symptoms can quickly get worse and become emergency conditions .
Also contact your provider if you have:
- Numbness, tingling, or pain in your feet or legs
- Problems with your eyesight
- Sores or infections on your feet
- Symptoms of high blood sugar
- Symptoms of low blood sugar
- Frequent feelings of depression or anxiety
You May Like: Type 1 Diabetes Symptoms In Adults
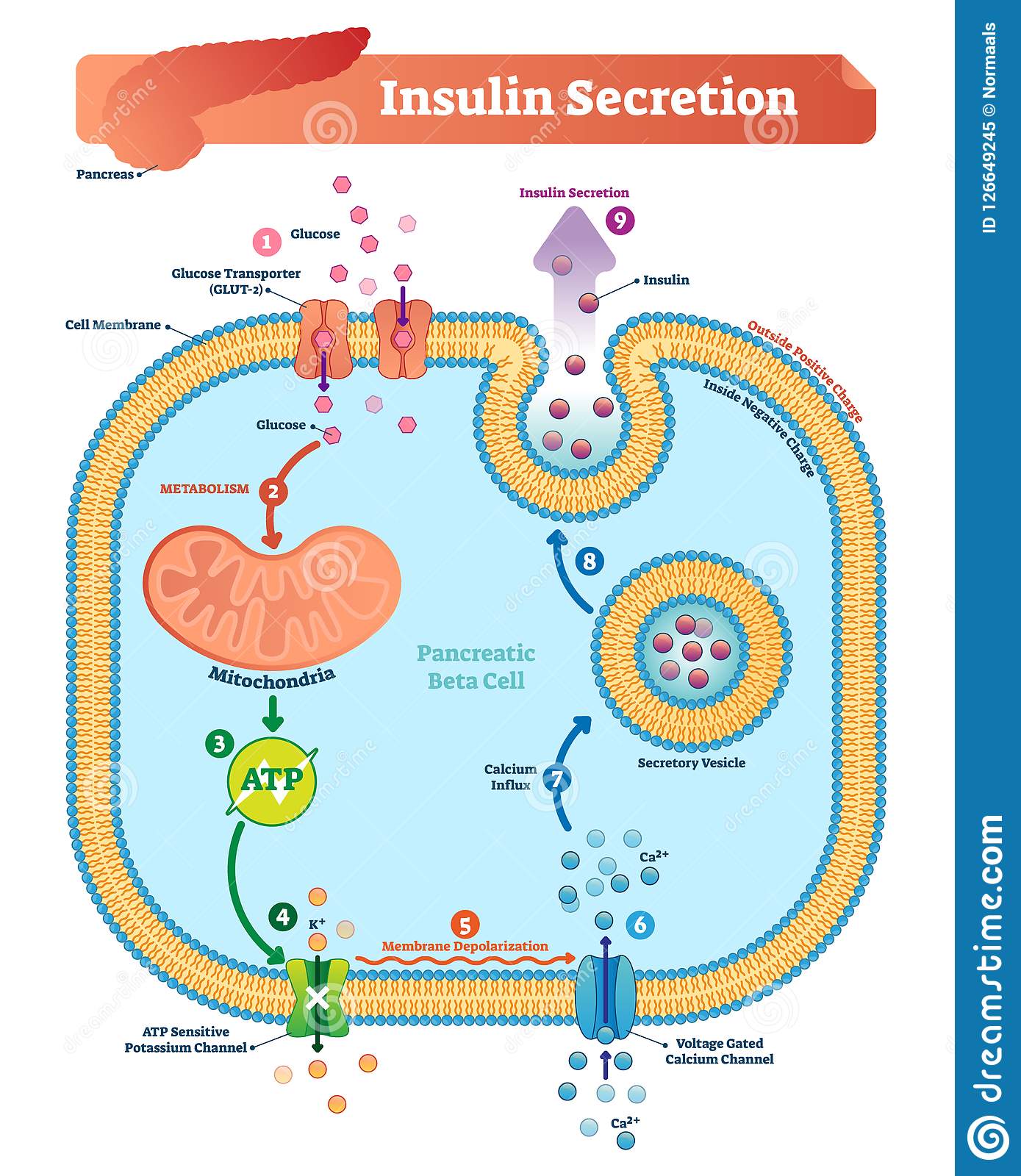
How Is Insulin Controlled
The main actions that insulin has are to allow glucose to enter cells to be used as energy and to maintain the amount of glucose found in the bloodstream within normal levels. The release of insulin is tightly regulated in healthy people in order to balance food intake and the metabolic needs of the body. This is a complex process and other hormones found in the gut and pancreas also contribute to this blood glucose regulation. When we eat food, glucose is absorbed from our gut into the bloodstream, raising blood glucose levels. This rise in blood glucose causes insulin to be released from the pancreas so glucose can move inside the cells and be used. As glucose moves inside the cells, the amount of glucose in the bloodstream returns to normal and insulin release slows down. Proteins in food and other hormones produced by the gut in response to food also stimulate insulin release. Hormones released in times of acute stress, such as adrenaline, stop the release of insulin, leading to higher blood glucose levels to help cope with the stressful event.
Insulin works in tandem with glucagon, another hormone produced by the pancreas. While insulin’s role is to lower blood sugar levels if needed, glucagon’s role is to raise blood sugar levels if they fall too low. Using this system, the body ensures that the blood glucose levels remain within set limits, which allows the body to function properly.
Functions Of Insulin In The Body: Good Guy Or Bad Guy
Insulin is perhaps the most important compound circulating in our bodies. It is involved in more than 60 key biological processes. Impairments in insulin function affect many facets of health and well-being and, if left uncorrected, are ultimately fatal. Despite its paramount importance, the functions of insulin in the body are widely misunderstood.
Insulin is an anabolic hormone, meaning it acts to promote synthesis and building, as opposed to catabolic hormones that break down and deconstruct bodily tissues and compounds. Given its vital importance, it is curious that insulin is sometimes portrayed as the bad guy. Consider, for instance, how we cast insulin as the villain responsible for the development of adverse health conditions: type 1 and type 2 diabetes, metabolic syndrome, polycystic ovary syndrome, and even certain types of cancer.
In this article, we will explore the basic functions of insulin in the body to gain a better appreciation for all it does as well as a clearer understanding of how to keep this hormone functioning in balance and at its optimal capacity.
Recommended Reading: How Can A Diabetic Wound Heal Faster
Insulin And Type 2 Diabetes
Type 2 diabetes is characterised by the body not responding effectively to insulin. This is termed insulin resistance. As a result the body is less able to take up glucose from the blood. In the earlier stages of type 2 diabetes, the body responds by producing more insulin than it would normally need to.
If type 2 diabetes develops over a number of years, the extra demands on the pancreas to produce insulin can lead to a loss of insulin producing cells as they wear out.
Depending on their level of insulin resistance, people with type 2 diabetes may also need to take insulin injections to manage their blood sugar levels.
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
Recommended Reading: What Does High Blood Sugar Feel Like
What Will Insulin Be Like In The Future
Pharmaceutical companies are working on very long-acting versions of insulin that could last for a week. There is also an ultra-fast version of insulin under development that will act in less than 15 minutes.
Another group of researchers is looking at glucose responsive insulin , which would react to the needs of your body in real time. It would have nanosensors bound to the insulin so that when insulin is needed, it releases, and when it isnt, it stops, according to Dr. Hirsch.
Understanding The Functions Of Insulin In The Body
As touched on previously, the presence of glucose stimulates the body to secrete insulin. However, other macronutrients, hormones, and biological compounds also stimulate insulin secretion. The primary function of insulin, as well as its counterpart, glucagon, is to regulate blood glucose concentrations.
Read Also: Contour Next One Blood Glucose Monitoring System
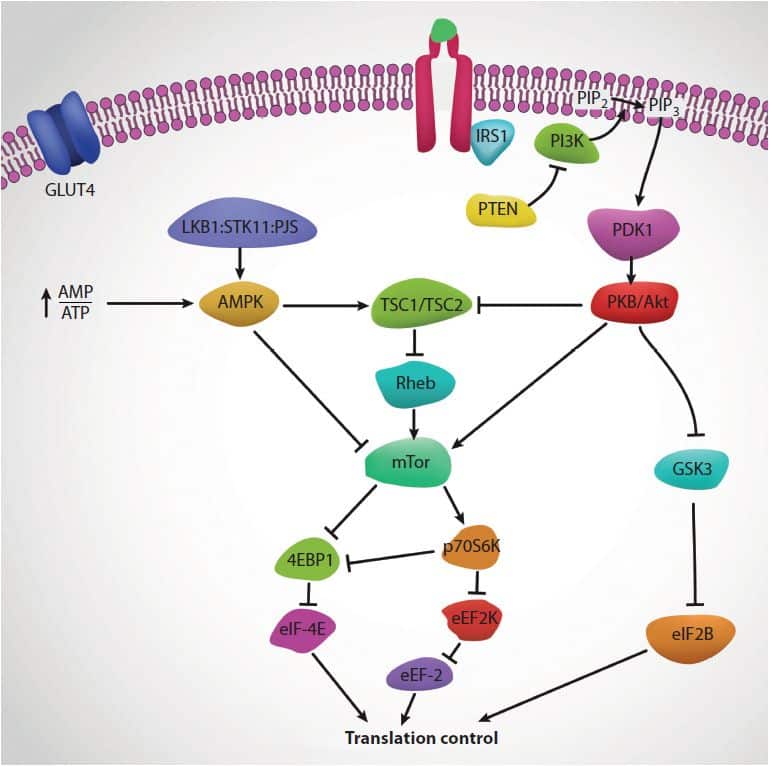
Physiologic Effects Of Insulin
Stand on a streetcorner and ask people if they know what insulin is, and many will reply, “Doesn’t it have something to do with blood sugar?” Indeed, that is correct, but such a response is a bit like saying “Mozart? Wasn’t he some kind of a musician?”
Insulin is a key player in the control of intermediary metabolism, and the big picture is that it organizes the use of fuels for either storage or oxidation. Through these activities, insulin has profound effects on both carbohydrate and lipid metabolism, and significant influences on protein and mineral metabolism. Consequently, derangements in insulin signalling have widespread and devastating effects on many organs and tissues.
The Insulin Receptor and Mechanism of Action
Like the receptors for other protein hormones, the receptor for insulin is embedded in the plasma membrane. The insulin receptor is composed of two alpha subunits and two beta subunits linked by disulfide bonds. The alpha chains are entirely extracellular and house insulin binding domains, while the linked beta chains penetrate through the plasma membrane.
Insulin and Carbohydrate Metabolism
It should be noted here that there are some tissues that do not require insulin for efficient uptake of glucose: important examples are brain and the liver. This is because these cells don’t use GLUT4 for importing glucose, but rather, another transporter that is not insulin-dependent.
Insulin and Lipid Metabolism
Other Notable Effects of Insulin
Biosynthesis And Export Of Insulin In Pancreatic
Insulin synthesis, processing, and packaging in pancreatic -cells
Humans have a single insulin gene, INS , located on chromosome 11, the transcription of which is controlled largely by upstream enhancer elements that bind key transcription factors that include IDX1 , MafA, and NeuroD1 along with numerous coregulators . In the insulin-producing pancreatic -cells, these are required for insulin gene expression and contribute to the regulation of INS transcription in response to glucose and autocrine insulin signaling . Given the role of these enhancer elements, transcription factors, and their coregulators in controlling the expression of insulin and many additional components of the -cell secretory pathway, such as glucose transporter 2 and the insulin processing enzyme PC1/3, they are key defining contributors to the establishment and maintenance of -cell identity .
Transit of immature secretory granules through the TGN, and their subsequent budding and maturation, is controlled by a host of regulatory proteins, including newly identified vesicle-sorting by proteins such as SORCS1 and HID-1 . Insulin biosynthesis in this manner is generally rapid and efficient, with only 12% of the protein remaining as proinsulin within mature secretory granules where insulin couples with Zn2+ and exists as a hexameric crystal with the cation. Transport of the insulin hexamer into the secretory granules is thought to be mediated by ZnT8 or related zinc transporters .
You May Like: Normal Glucose Range For Diabetics
How Do You Take Insulin
The most common way of intaking insulin is Subcutaneous insulin injections. A person can intake insulins through an insulin syringe, insulin pen, insulin pumps and vials. Insulin can be injected into the body via the abdomen, upper arm, lower back, hips and buttocks.
Following are the ways to inject insulin into your body:
- Gently pinch the skin and insert the needle at an angle of 45 degrees.
- If your skin tissues are hard, insert the needle at an angle of 90 degrees.
- Now, push the needle into the skin.
- After injection, rub your skin gently with cotton.
How Insulin Functions On A Cellular Level
The primary functions of insulin in the body’s cells have to do with the metabolism of carbohydrates, fats, and amino acids from protein as well as the transcription and translation of mRNA.
- Carbohydrates: Insulin contributes to carbohydrate metabolism at many points during the process. It facilitates the diffusion of glucose from carbohydrates into fat and muscle cells, signals the presence of an abundance of intracellular energy, and more.
- Fats: Insulin instigates the synthesis of fatty acids in adipose tissue as well as in the liver and in the mammary glands during lactation. It also affects the metabolism of phospholipids.
- Protein: Insulin stimulates protein synthesis throughout the body. It also contributes to the transcription of mRNA as well as aiding translation of mRNA into ribosomal proteins.
In a big-picture sense, insulin’s role has to do with the regulation of the body’s cellular energy supply and the balance of micronutrients. When the body is in a fed, as opposed to fasting, state, insulin orchestrates the anabolic processes that lead to muscle growth , tissue healing, and more. Insulin signals an abundance of energy, indicating to the body that it can halt the breakdown of fat stores and instead carry out fat synthesis.
Also Check: Where Are Insulin Pumps Placed