What Does The American Diabetes Association Say About Continuous Glucose Monitoring
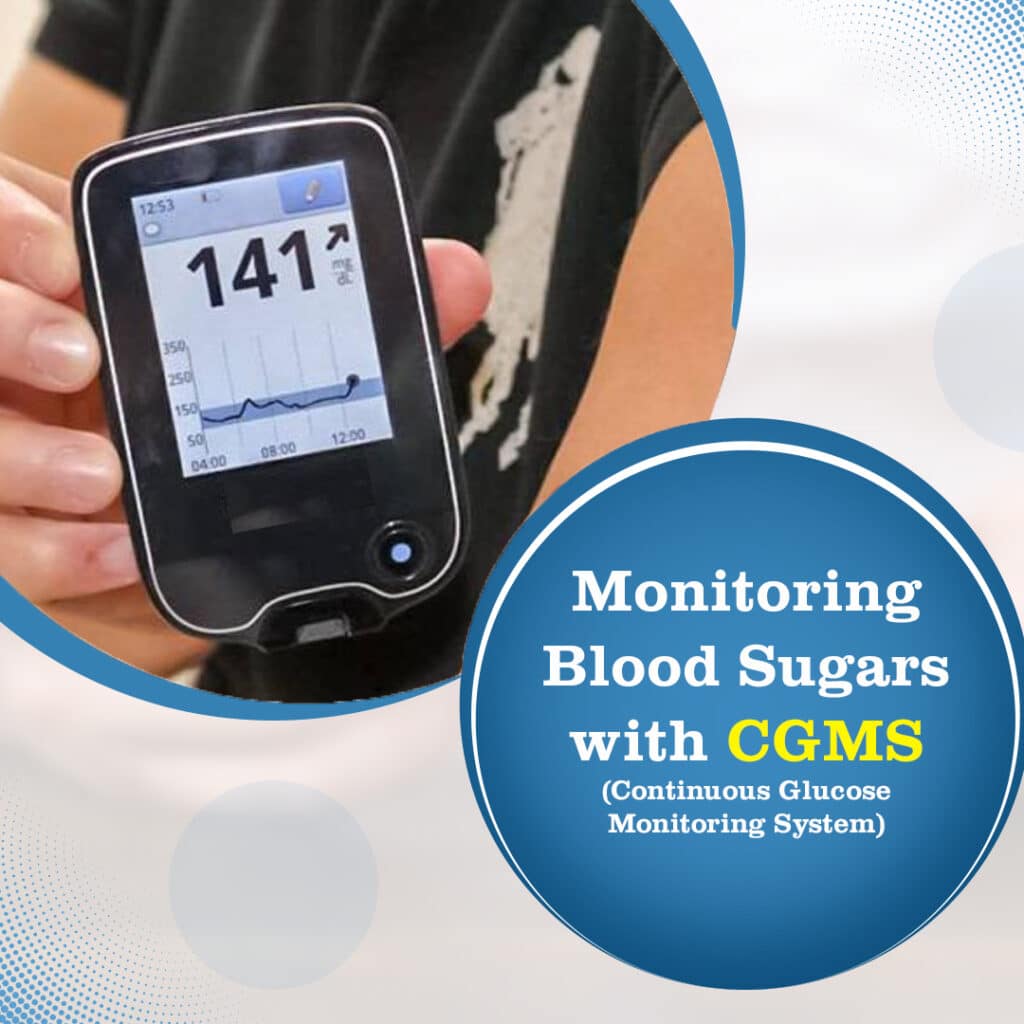
CGMs provide users with real-time, dynamic information about their levels around the clock and alerts to prevent dangerous high or low glucose levels, leading to better diabetes management and ultimately improved health outcomes. And theyre not the only ones.
The Endocrine Society recommends CGM for those with A1C above 7%, the typical goal for type 1 diabetes. In 2017, the Journal of Diabetes Science and Technology published a study that concluded the use of CGM facilitated greater A1C improvements and reduced healthcare system use compared to SMBG use, regardless of how the patients administer insulin.
The National Institute of Diabetes and Digestive and Kidney Diseases explains that a CGMS can help you better manage your glucose levels and have fewer low blood glucose emergencies.
A Few Points About Sensor Care
Veterinary nurses are commonly involved in applying these sensors, showing clients how to use them, and downloading the results. Its therefore really important that we understand how the sensors work and advise clients on their use/care. A few points to mention to your clients are:
-
Not allowing dogs to swim or bathe with a sensor in place
-
Ensuring clients know that though the sensors can last up to 14 days, the full 14 days is not guaranteed in veterinary patients, and sensors may not last this long
-
Any glucose first aid requirements at home – e.g. what to do if the glucose level is below a certain cutoff value around the time of insulin administration
So, continuous glucose monitors are a great new alternative to glucose curves in our diabetic patients. But, as weve discussed, they wont be suitable for every patient – for example, emergency/unstable patients who have not had any initial stabilisation, dehydrated patients, and patients where we want to catch rapid fluctuations in glucose levels. However, for many patients, they will provide us with more information than we can gather using traditional monitoring, and minimise venepuncture, stress and hospitalisation.
Do you use continuous glucose monitors in your practice? Let me know below!
Learning To Use Your Cgm Or Freestyle Libre
Your diabetes healthcare team will set you up with your CGM or Freestyle Libre if its free on the NHS and show you how to use it. Sometimes manufacturers will help you set up the technology this is fine and can help your healthcare team get more people on to the technology more quickly.
Abbott, which supply the FreeStyle Libre, also provide free online learning for people with diabetes using the technology to help them get the most from it.
You may also benefit from going on a diabetes education course if you use Flash or CGM. Ask your GP or other diabetes healthcare professional to refer you.
If you want to share your experiences about using tech or find out information by asking others using it, go to our forum.
Recommended Reading: Does Diabetes Lead To Kidney Failure
Continuous Glucose Monitoring Insurance Coverage
Continuous Glucose Monitoring insurance coverage is, first of all going to be dictated by whether or not you have insurance, and then, by what type of insurance you have. Is it private insurance, or Medicare or Medicaid? All of these factors will play into what type of coverage you have for a CGM system.
There is some really exciting updated coverage news for 2017 Medicare just announced it will cover Dexcoms G5 Mobile CGM under Durable Medical Equipment status. This is excellent news for Dexcom and for anyone who is covered by Medicare. This will only apply for Dexcoms Mobile system which can be accessed from certain Smartphones.
Historically, people with Type 1 diabetes will usually qualify easier for a CGM than those with Type 2 diabetes, but if your physician can prove there is a medical necessity, then you may qualify for coverage. Lets say you have coverage. Next, your insurance company may want to determine if you actually need a continuous glucose monitor. This can be done by providing blood glucose logs which are uploaded from your blood glucose meter. If you are experiencing both high blood sugars and low blood sugars, more than likely you will qualify. What will they consider as high and low? Hyperglycemia is defined as a blood glucose level of 250mg/dL or over. A low blood sugar is 70mg/dL or below.
How Do I Get A Cgm

As with most medical technology, you need a prescription to get a CGM. Your doctor can write a prescription for any of the above CGM devices.
But getting a prescription for a CGM is often not as simple as just walking into your doctors office and asking for one. Instead, youll likely need a prior authorization to get a CGM through your health insurance. A PA is form/process that your doctor has to go through to prove medical necessity to obtain approval from your insurance plan to cover the costs associated with the prescribed treatment .
At this point, most major insurers require a PA before extending coverage for CGM. Heres how to go about securing a PA, according to JDRF, a leading T1D research and support organization:
Don’t Miss: Can You Lose Weight If You Have Diabetes
Why Do People Stop Using Cgm
A 2018 study conducted by GlySens Inc surveyed 1,348 respondents to discover their reasons for quitting their CGM usage. Two of the top five reasons given by adults were too expensive and not covered by insurance. The other top five reasons were that the sensor was uncomfortable, they had too many alerts, and they believed the data wasnt as accurate as their SMBG.
More Insight Into Your Blood Sugar Trends
A 2016 review of self-monitoring of blood glucose presents evidence that CGM is a more effective monitoring method for insulin-dependent diabetes mellitus. CGM devices help prevent hypoglycemia and hyperglycemia by recording the speed and direction of changes in glucose levels. They give you a more complete picture, eliminate missed testing intervals, and alert you at customized thresholds.
Recommended Reading: Type 2 Diabetes Research Studies
Getting The Freestyle Libre App On Your Mobile Phone
To scan your Freestyle Libre 1 or Freestyle Libre 2 sensors from a smart mobile phone, download the the Freestyle LibreLink app from the app store on your phone.
Sharing data with friends and family
You can also share the data from your Freestyle Libre with friends, family or carers via the Libre Linkup app. They will need to download the LibreLinkUp app and create an account. You can then give them access to your data using your own LibreLink app and their email address
If its your first time opening the app, then you may need to set up an account. Once youve done that, hold your phone or device up to the sensor and you should feel it buzz twice. The sensor has been scanned and the app requires 60 minutes to calibrate so youll need to wait that long and then you can use it.
How Accurate Are Continuous Glucose Monitors
The accuracy of certain meters is tested by determining the MARD mean absolute relative difference. MARD measures the difference between a meters result and the corresponding laboratory measurement.
A MARD less than 10% is considered good analytical performance. Clinical data for the Dexcom G6 one of the most popular CGM systems shows a MARD of 9%, and the sensors maintain that MARD over the time theyre worn.
CGM has proven so accurate that medical professionals consider it a better metric for therapeutic decisions. A 2017 German study revealed that it might be risky from a therapeutic point of view to use blood glucose for therapeutic decisions.
They conclude that it may be reasonable to abandon blood glucose measurements as the basis for diabetes management and switch to using ISF glucose as the appropriate therapeutic target.
Sidenote: Keep in mind therapeutic targets are different than acute treatment. You should always check your blood sugar before responding to a dip or spike reported by your CGM device. And talk to your doctor before making any changes to your insulin regimen.
Recommended Reading: How To Lose Weight When You Are Diabetic
Continuous Glucose Monitoring And Flash
You can check your sugar levels at any time with a continuous glucose monitor or flash monitor.
It lets you see patterns in your levels and check if your glucose is too high or low. It can help you control your blood glucose levels, as you’ll have more information and can take action quickly.
It can help you and your diabetes team see:
- if your glucose levels are going up or down
- how your glucose levels change over time
- what happens to your levels when you’re asleep
If your blood glucose reading is:
- high it could be a sign of hyperglycaemia
- low it could be a sign of hypoglycaemia
Do I Need Cgm To Manage Diabetes
You can regularly check your blood glucose levels using a fingerstick blood check and a blood glucose monitor. Many people do just that.
But fingerstick checks only measure blood glucose at one moment in time. Its like reading one page of a book. Doing more fingerstick checks gives you more snapshots, which can offer clues to whats happening with your blood sugar levels.
Read Also: Continuous Glucose Monitor For Dogs
Do Continuous Glucose Monitors Have A Needle
Kind of. Placement of the sensor works like an IV, an intravenous catheter used to deliver fluid and medications. A needle is inserted into the skin. The needle has a tiny filament inside. The needle is removed, and the filament stays in. These two steps happen quickly and automatically when you use a CGM applicator.
Continuous Glucose Monitoring Fact Sheet

Continuous glucose monitoring is a way to check glucose levels throughout the day and night without pricking your finger.
CGM can help you see the effects of insulin and other medicines, food, physical activity, and illness on your glucose levels. It can help you make decisions to keep your glucose levels in a healthy range. It can also help find trends or changes in your glucose levels. You can use this information to make day-to-day decisions about how to manage your diabetes. You can also share this information with your diabetes health professionals to help make decisions about your diabetes management. CGM provides more information than blood glucose monitoring with a finger prick check.
Read more in our fact sheet Continuous glucose monitoring.
Read Also: What Are The Two Different Types Of Diabetes
What Are The Contraindications For Blood Glucose Monitoring
A comprehensive study of the effects of CGM conducted in 2013 by the German Diabetes Association revealed the following contraindications meaning these factors do not predict success with CGM devices:
-
lack of motivation and compliance
-
fear of technology/lack of trust in technology
-
alcohol and drug abuse
-
unrelated psychological conditions like psychoses or eating disorders
Getting Free Flash Sensors And Cgm Sensors
If you get a Freestyle Libre or a CGM on the NHS, you should also get the other things you need like sensors and replacement parts.
Its also worth knowing that sensors only work for individual products, so sensors for a Freestyle Libre wont work for a Freestyle Libre 2 or a CGM.
Using a Freestyle Libre helps me prevent hypos and its much more sociable because when I’m out, I dont have to find somewhere convenient and clean to do a finger prick check. Im lucky I can afford to self-fund.
Read Also: How Can You Cure Diabetes
What About Health Insurance Coverage
Its helpful to know that the Dexcom G6, Abbott FreeStyle Libre 2, and Eversense implantable CGM are all covered by most private and public health insurance plans, including Medicare . Medtronics Guardian Connect, however, was not covered by Medicare as of December 2021.
Historically, people with type 1 diabetes have had a much easier time qualifying for a CGM through insurance than those with type 2 diabetes because it was easier to establish medical necessity.
Still, if you have T2D and your doctor can make a case for medical necessity, you may qualify. But your insurance company may still want to confirm whether you actually need a CGM.
If you can prove youre experiencing both high blood sugars and low blood sugars regularly, you will likely qualify. This can be proven by providing blood glucose logs uploaded from your fingerstick meter. Generally, hyperglycemia is defined as a blood glucose level of 250 mg/dL or over, while hypoglycemia is a blood sugar 70 mg/dL or below.
If your insurance company denies your coverage for a CGM, talk with your doctors office about peer-to-peer reviews and appeals. Pushing your doctor to fight for you matters.
Manufacturers can have your back here, too. Dexcom, for instance, has an easy-to-complete patient information form you can submit along with your insurance information. The company will then contact your insurer to work on getting your device authorized and covered. Medtronic offers a similar service.
Traveling With Your Cgm
When flying, TSA is very familiar with insulin pumps and continuous glucose monitoring systems. Just show them the device that you are wearing, tell them exactly what it is and show them your monitor. Ask that the monitor or sensors not be put through the x ray machine because they may become damaged from the x rays. The following excerpt was taken from Dexcomâs website regarding this important information:
X-Ray Machines
Receiver, Extra Sensors
Dont put your Dexcom G5® Mobile CGM System components through baggage x-ray machines. Before your screening process begins, ask the TSA Officer to perform a visual inspection of the receiver and your extra sensors. Place all Dexcom G5® Mobile components in a separate bag before handing over to the Security Officer. For other medical supplies, such as medications, meters, and strips, check manufacturers instructions or the TSA website.
to download our âNotice of Medical Deviceâ letter. This can be filled out by your physician and presented to airport security to better explain your Dexcom CGM System.
Use of AIT body scanners has not been studied and therefore we recommend hand-wanding or full body pat down and visual inspection in those situations.
Recommended Reading: Can High Cholesterol Lead To Diabetes
Cgm Benefits At A Glance
-
Continuous glucose monitoring requires virtually zero fingersticks.
-
Make proactive treatment decisions by seeing your blood sugar before symptoms.
-
Get more insight into your blood glucose level trends with recorded data.
-
Improve your health and experience a better quality of life.
-
Medicare covers CGM for those who qualify.
How To Remove A Cgm Sensor
Sensor removal can be tricky, especially when patches are too sticky, or there is just simply too many of them. This is where the NJaP patches come to the rescue! Our CGM patches are not only useful to keep the sensor in place, but also to easily remove it after its job is done. We also wrote down some great tips on how to keep your sensor from falling off.
Also Check: How To Deal With Gestational Diabetes
You May Like: Is Nutrisystem Good For Diabetics
Some People Dont Want To Wear A Cgm Sensor
For some people, it comes down to simply not wanting to wear a sensor on their body. This aversion is typically seen in people with new-onset type 1 diabetes who arent yet comfortable with the intensive regimen theyll have to maintain.
Adolescents between the ages of eight and 18 are also more reluctant than other age groups to wear their sensors because of the social stigma they perceive.
No : Understand Your Clients Why
If one of your clients shares with you that theyre using a continuous glucose monitor, getting a sense of their motivation for using the device will help inform the nutrition strategy you create. For example, is your client in the prediabetic range and using the CGM to see which foods may be causing her elevated blood sugar? Or, was your client lured by an Instagram ad or magazine article, and invested in a month-long CGM experience to gain more insights about how her body is responding to the food shes eating and what changes she can make to lose weight? While the reasons your clients will use a CGM will vary, understanding their why? is an essential first step to devise a plan thatll help each client make the most of using a CGM, says Koff.
Also Check: Blood Sugar Levels 1 Hour After Eating
Cost Of Buying A Freestyle Libre
The cost of Freestyle Libre or Freestyle Libre 2 sensors are around £50 every 2 weeks. If you have a compatible smartphone you can just and use your phone to scan the sensor to see the readings. But if you dont, you can buy a small device called a reader, for around £50 and this is a one-off purchase. Speak to your healthcare professional about where you can buy a reader from they can be available direct from the manufacturer , from a pharmacy or online but this can change.