How Do I Take It
Many people get insulin into their blood using a needle and syringe, a cartridge system, or pre-filled pen systems.
The place on the body where you give yourself the shot may matter. You’ll absorb insulin the most evenly when you inject it into your belly. The next best places to inject it are your arms, thighs, and buttocks. Make it a habit to inject insulin at the same general area of your body, but change up the exact injection spot. This helps lessen scarring under the skin.
Inhaled insulin, insulin pumps, and a quick-acting insulin device are also available.
Inhaled Insulin And Respiratory Side Effects
An inhaled form of ultra-rapid-acting insulin called Technosphere® Insulin has been developed to help diabetic patients control their postprandial glucose levels . TI has a faster onset of action and a shorter duration of action compared to subcutaneously injected insulins. A comprehensive safety review of TI analyzed data from 13 controlled phase 2/3 clinical studies. In these studies, treatment with TI was compared to either inhaled placebo or an active-comparator treatment in both Type 1 and Type 2 DM patients. The safety review specifically looked for respiratory treatment-emergent adverse events , pulmonary function alterations, and lung malignancies. The study reported an increase of frequency in mild cough in the TI group compared to active-comparator therapy . The cough was generally mild, non-productive, usually occurred within 10 min of inhalation, and diminished over time. TI therapy also resulted in a slight decline in pulmonary function from baseline compared to the TP group and the active-comparator treatment group. The decline in pulmonary function returned to baseline after the first month. Importantly, the study reported lung malignancies in two patients with a history of smoking in the TI treatment group. Overall, the incidence of malignancies in the TI study population was similar to that in the study population with diabetes. In summary, the safety review concluded that inhaled TI is a safe alternative with no persistent pulmonary safety concerns.
Insulin Analogs Are Now Replacing Human Insulin In The Us
Insulins are categorized by differences in onset, peak, duration, concentration, and route of delivery.
Human Insulin and Insulin Analogs are available for insulin replacement therapy. Insulins also are classified by the timing of their action in your body specifically, how quickly they start to act, when they have a maximal effect and how long they act.Insulin analogs have been developed because human insulins have limitations when injected under the skin. In high concentrations, such as in a vial or cartridge, human clumps together. This clumping causes slow and unpredictable absorption from the subcutaneous tissue and a dose-dependent duration of action . In contrast, insulin analogs have a more predictable duration of action. The rapid acting insulin analogs work more quickly, and the long acting insulin analogs last longer and have a more even, peakless effect.
You May Like: Healthy Breakfast Bars For Diabetics
Different Types Of Insulin
Insulin A to Z: A Guide on Different Types of Insulin Elizabeth Blair, A.N.P., at Joslin Diabetes Center, helps break down the different types of insulin and how they work for people with diabetes. Types of Insulin for People with Diabetes Rapid-acting: Usually taken before a meal to cover the blood glucose elevation from eating. This type of insulin is used with longer-acting insulin. Short-acting: Usually taken about 30 minutes before a meal to cover the blood glucose elevation from eating. This type of insulin is used with longer-acting insulin. Intermediate-acting: Covers the blood glucoseelevations when rapid-acting insulins stop working.This type of insulin is often combined with rapid- or short-acting insulin and is usually taken twice a day. Long-acting: This type of insulin is often combined, when needed, with rapid- or short-acting insulin. It lowers blood glucose levels when rapid-acting insulins stop working. It is taken once or twice a day. A Guide on Insulin Types for People with DiabetesContinue reading > >
Just Say No To The Sliding Scale
Rapid-acting insulins are also effective for use as a corrective measure, aka correction factor , to maintain optimal blood glucose targets for patients in hospital. This approach replaces the commonly used insulin sliding scale. Sliding scales represent a reactive, rather than a proactive, approach to blood glucose control. They deliver variable amounts of insulin at variable times, generally resulting in those swinging blood glucose levels. Instead, the use of a rapid-acting insulin CF at mealtimes alongside an established diabetes medication regimen will result in much smoother blood glucose control. The application of this principle will be explained for each hospital setting.
Derek G. Waller BSc , DM, MBBS , FRCP, Anthony P. Sampson MA, PhD, FHEA, FBPhS, in, 2018
Also Check: Where Do You Take Insulin Shots
The High Blood Sugar Correction Factor:
Correction Factor = 1800 ÷Total Daily Insulin Dose = 1 unit of insulin will reduce the blood sugar so many mg/dl
This can be calculated using the Rule of 1800.
Example:
= 1800 ÷ TDI = 1 unit insulin will drop reduce the blood sugar level by 45 mg/dl
While the calculation is 1 unit will drop the blood sugar 45 mg/dl, to make it easier most people will round up or round down the number so the suggested correction factor may be 1 unit of rapid acting insulin will drop the blood sugar 40-50 mg/dl.
Please keep in mind, the estimated insulin regimen is an initial best guess and the dose may need to be modified to keep your blood sugar on target.
Also, there are many variations of insulin therapy. You will need to work out your specific insulin requirements and dose regimen with your medical provider and diabetes team.
How Are Doses Scheduled
Follow your doctor’s guidelines on when to take your insulin. The time span between your shot and meals may vary depending on the type you use.
In general, though, you should coordinate your injection with a meal. You want to time your shot so that the glucose from your food gets into your system at about the same time that the insulin starts to work. This will help your body use the glucose and avoid low blood sugar reactions. From the chart on page 1, the “onset” column shows when the insulin will begin to work in your body. You want that to happen at the same time you’re absorbing food. Good timing will help you avoid low blood sugar levels.
- Rapid acting insulins: About 15 minutes before mealtime
- Short-acting insulins: 30 to 60 minutes before a meal
- Intermediate-acting insulins: Up to 1 hour prior to a meal
- Pre-mixed insulins: Depending on the product, between 10 minutes or 30 to 45 minutes before mealtime
Recommended Reading: Can You Control Type 2 Diabetes
Disposal Of Used Insulin Syringes
Used syringes, pen needles, cannulas and lancets must be disposed of in an Australian Standards-approved sharps container, which is puncture-proof and has a secure lid. These containers are usually yellow and are available through pharmacies, local municipal councils and state or territory diabetes organisations such as Diabetes Victoria.
Procedures to dispose of sharps containers vary from state to state.
For sharps disposal information and help, you can contact:
- state or territory diabetes organisations, such as Diabetes Victoria
- state Department of Health
Insulin needs to be stored correctly. This includes:
- Store unopened insulin on its side in a fridge.
- Keep the fridge temperature between 2 and 8 °C.
- Make sure that insulin does not freeze.
- Once opened, keep it at room temperature for not more than one month and then dispose of it safely.
- Avoid keeping insulin in direct sunlight.
Extreme temperatures can damage insulin so it doesn’t work properly. It must not be left where temperatures are over 30 °C. In summer your car can get this hot so don’t leave your insulin there.
There are various insulated insulin carry bags available for transporting insulin.
How Does It Work
Type 1 Diabetes, formerly known as Juvenile Onset Diabetes, is an autoimmune disorder that often develops at younger ages, however can occur at adulthood as well. It is believed that the immune system of the Type 1 Diabetic attacks the cells in the Pancreas called Beta Cells, which are responsible for producing insulin. Insulin is a hormone that helps regulate levels of blood sugar in the bloodstream. Symptoms of Type 1 Diabetes can include excessive hunger, thirst and urination, weight loss, blurred vision and tingling in the hands and feet. For people who do not have Diabetes, insulin is produced at a normal, constant levels on a consistent basis, with surges of extra insulin released after meals are ingested. Without the Beta Cells in the Pancreas producing insulin, there is no way for the blood glucose to be controlled in a Type 1 Diabetic without proper medical intervention. Uncontrolled Blood Glucose levels can be life-threatening and need to be managed as quickly as possible by a physician.
1515 North Flagler Drive Suite 440 West Palm Beach, FL 33401
© Metabolic Research Institute, Inc. 2016-2017 All Rights Reserved. Website Design & Manager: VKA
Also Check: How Much Does Type 1 Diabetes Cost Per Year
Data Collection And Analysis
Two review authors independently extracted data and assessed the risk of bias. We assessed dichotomous outcomes by risk ratios , and Peto odds ratios , with 95% confidence intervals . We assessed continuous outcomes by mean differences with 95% CI. We assessed trials for certainty of the evidence using the GRADE approach.
First Some Basic Things To Know About Insulin:
- Approximately 40-50% of the total daily insulin dose is to replace insulin overnight, when you are fasting and between meals. This is called background or basal insulin replacement. The basal or background insulin dose usually is constant from day to day.
- The other 50-60% of the total daily insulin dose is for carbohydrate coverage and high blood sugar correction. This is called the bolus insulin replacement.
Bolus Carbohydrate coverage
The bolus dose for food coverage is prescribed as an insulin to carbohydrate ratio.The insulin to carbohydrate ratio represents how many grams of carbohydrate are covered or disposed of by 1 unit of insulin.
Generally, one unit of rapid-acting insulin will dispose of 12-15 grams of carbohydrate. This range can vary from 4-30 grams or more of carbohydrate depending on an individuals sensitivity to insulin. Insulin sensitivity can vary according to the time of day, from person to person, and is affected by physical activity and stress.
Bolus High blood sugar correction
The bolus dose for high blood sugar correction is defined as how much one unit of rapid-acting insulin will drop the blood sugar.
Generally, to correct a high blood sugar, one unit of insulin is needed to drop the blood glucose by 50 mg/dl. This drop in blood sugar can range from 15-100 mg/dl or more, depending on individual insulin sensitivities, and other circumstances.
Also Check: Does A Child With Type 1 Diabetes Qualify For Disability
Data Synthesis And Analysis
Analyses were conducted using the RevMan 5.3 software. Relative risk was used as a summary measure of effect size for dichotomous outcomes, the mean difference was used for continuous outcomes, and the risk rate was used for outcomes related to the number of events. The meta-analysis was performed using a random-effects model based on the DerSimonianLaird method, 95% confidence interval . A p-value< 0.1 was considered statistically significant. Heterogeneity between the studies was assessed using I2 statistic, in which values above 50% were indicative of high heterogeneity . Heterogeneity as determined by the Chi square test was considered non-significant for I2 values between 0 and 50%, moderate for values between 51 and 79%, and significant for values between 80 and 100%. Where possible, study data were pooled and summarized in meta-analysis charts using the RevMan 5.3 software otherwise, the results of each study were presented individually .
Physical And Chemical Properties
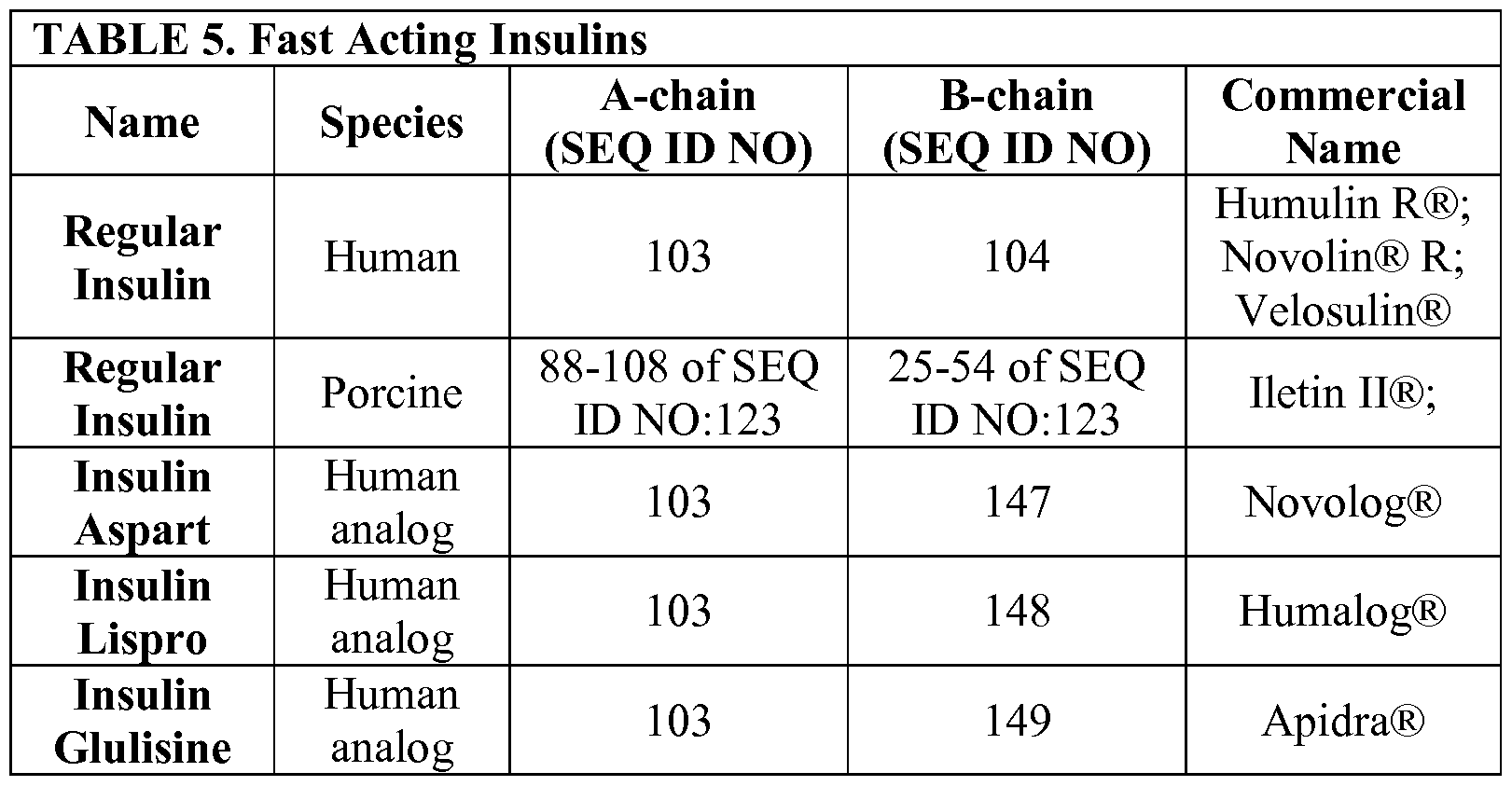
Regular human insulin is crystalline zinc insulin dissolved in a clear solution. It may be administered by any parenteral route: subcutaneous, intramuscular, or intravenous. Insulin aspart, glulisine and lispro are also soluble crystalline zinc insulin, but are intended for subcutaneous injection. When administered intravenously, the action of these rapid-acting insulin analogs is identical to that of regular insulin. NPH, or neutral protamine Hagedorn, is a suspension of regular insulin complexed with protamine that delays its absorption. Insulin suspensions should not be administered intravenously. All insulins, except insulin glargine, are formulated to a neutral pH.
Long-acting insulin glargine is a soluble, clear insulin, with a pH of 4.0 which affects its SQ absorption characteristics, discussed further in the pharmacokinetics section. Insulin glargine should not be mixed with other insulins, and should only be administered subcutaneously . Insulin detemir is an insulin analog coupled to an 18-chain fatty acid that binds to albumin in the SQ tissue. This results in delayed absorption and a prolonged duration of action. Insulin degludec is an ultra-long insulin analog that breaks down into monomers from dissociating zinc molecules after administration . Insulins detemir and degludec should also not be mixed with other insulins and are intended only for subcutaneous use .
Also Check: Doterra Essential Oils For Diabetes
Subgroup And Sensitivity Analysis
Subgroup analyses were designed based on the effects by neutral protamine Hagedorn human insulin vs. long-acting insulin analogues. We also carried out a sensitivity analysis for the primary outcome all hypoglycemic episodes considering the risk of bias in the studies. A second meta-analysis was then performed for this outcome excluding studies with three or more domains classified as high risk of bias.
Data Extraction And Quality Assessment
Two reviewers independently extracted data from each study using an extract table template, which provided the following information: title of the study demographic characteristics study design intervention details and outcomes. A third reviewer further assessed all RCTs to check for completeness of data.
In case of missing data, the authors of the studies were contacted for additional information. If the missing data could not be retrieved, the study was not included. Retrieved missing data were presented in a narrative form.
To assess the internal quality of the studies, we ran each RCT through the Cochrane Collaboration tool for assessing the risk of bias . The following potential issues were assessed: random sequence generation allocation concealment blinding of participants and outcome assessors blinding of outcomes incomplete outcome data selective reporting and other sources of bias. For each domain, the risk of bias was rated as low, high, or unclear. The quality of evidence was assessed using the GRADEpro GDT software . The results were presented in a Summary of Findings table.
You May Like: Sourdough Bread Good For Diabetics
What Type Of Insulin Is Best For My Diabetes
Your doctor will work with you to prescribe the type of insulin that’s best for you and your diabetes. Making that choice will depend on many things, including:
- How you respond to insulin.
- Lifestyle choices. The type of food you eat, how much alcohol you drink, or how much exercise you get will all affect how your body uses insulin.
- Your willingness to give yourself multiple injections per day
- Your age
- Your goals for managing your blood sugar
Your doctor may prescribe more than one type. You might need to take insulin more than once daily, to space your doses throughout the day, or to add other medicines.
Afrezza, a rapid-acting inhaled insulin, is FDA-approved for use before meals for both type 1 and type 2 diabetes. The drug peaks in your blood in about 15-20 minutes and it clears your body in 2-3 hours. It must be used along with long-acting insulin in people with type 1 diabetes.
The chart below lists the types of injectable insulin with details about onset , peak and duration . These three things may vary. The final column offers some insight into the “coverage” provided by the different insulin types in relation to mealtime.
| Type of Insulin & Brand Names | Onset |
| 30 min.-2 1/2 hours | 16-20 hours |
| *Premixed insulins combine specific amounts of intermediate-acting and short-acting insulin in one bottle or insulin pen. |
How Do You Know If The Insulin In Your Body Isnt Working Properly
People with type 1 diabetes are generally diagnosed when symptoms cause them to seek medical care.
Type 2 diabetes is often diagnosed with a simple blood test during a routine physical exam or annual checkup.
A lab test of your fasting blood sugar levels or an A1C test can indicate if your blood sugar is within a healthy range. This can signal whether the insulin in your body is working correctly.
Also Check: What Is Diabetic Retinopathy Screening
Total Daily Insulin Requirement
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
Exceptions To Insulin Dosing And Timing
Long-acting insulins arenât tied to mealtimes. Youâll take detemir once or twice a day no matter when you eat. And youâll take glargine once a day, always at the same time. Deglutec is taken once a day, and the time of day can be flexible. But some people do have to pair a long-acting insulin with a shorter-acting type or another medication that does have to be taken at meal time.
Rapid-acting products can also be taken right after you eat, rather than 15 minutes before mealtime. You can take some of them at bedtime.
For more information about when to take insulin, read the “dosing and administration” section of the insulin product package insert that came with your insulin product, or talk with your doctor.
Read Also: Most Accurate Glucose Meter 2021