How Your Body Regulates Blood Sugar
If you don’t have diabetes, your body naturally regulates blood sugar levels. After you eat a meal, your body breaks down foods into their components, which are absorbed from your gut into your bloodstream. Any carb-based foods, like milk and dairy, starches and fruit, will be broken down into their componentsmuch of which is glucose. Once higher glucose levels are detected in your bloodtypically after a mealthe pancreas releases insulin, which causes the body to absorb glucose from the blood, thereby lowering blood sugar levels back to normal, per the Centers for Disease Control and Prevention. If your blood sugar levels get too low, the insulin level goes down and glucagon is released, which causes the liver to turn stored glycogen back into glucose and release it into the blood. This helps bring blood sugar levels back to normal.
Risk Factors For Prediabetes And Diabetes
The American Diabetes Association recommends testing for prediabetes and diabetes in adults without symptoms who are overweight and have one or more risk factors. They include:
- lack of physical inactivity
- impaired fasting glucose or glucose tolerance in previous testing
- severe obesity and other conditions associated with insulin resistance
- cardiovascular disease
Talk to your doctor about blood test options to diagnose prediabetes. If test results are normal, testing should be repeated at least every three years. In those without these risk factors, testing should begin at age 35.
Glycemic Targets: Standards Of Medical Care In Diabetes2021
American Diabetes Association 6. Glycemic Targets: Standards of Medical Care in Diabetes2021. Diabetes Care 1 January 2021 44 : S73S84.
The American Diabetes Association Standards of Medical Care in Diabetes includes the ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee , are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations, please refer to the Standards of Care Introduction . Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC.
Also Check: Protein Shake For Diabetic Patients
The Big Picture: Checking Your Blood Glucose
Blood sugar monitoring is the primary tool you have to find out if your blood glucose levels are within your target range. This tells you your blood glucose level at any one time.
Its important for blood glucose levels to stay in a healthy range. If glucose levels get too low, we can lose the ability to think and function normally. If they get too high and stay high, it can cause damage or complications to the body over the course of many years.
The logging of your results is vital. When you bring your log to your health care provider, youll have a good picture of your body’s response to your diabetes care plan. To help keep track of your levels, we have a glucose log. We also have a blood glucose log available for purchase that is smaller so you can carry it with you.
What Are The Target Ranges
Blood glucose targets are individualized based on:
- duration of diabetes
- conditions a person may have
- cardiovascular disease or diabetes complications
- hypoglycemia unawareness
- individual patient considerations
The American Diabetes Association suggests the following targets for most nonpregnant adults with diabetes. A1C targets differ based on age and health. Also, more or less stringent glycemic goals may be appropriate for each individual.
- A1C: Less than 7%A1C may also be reported as eAG: Less than 154 mg/dL
- Before a meal : 80130 mg/dL
- 1-2 hours after beginning of the meal *: Less than 180 mg/dL
Don’t Miss: How Do I Get My Diabetic Supplies Through Medicare
What Can Make My Blood Glucose Rise
Hyperglycemia is the technical term for high blood glucose . It happens when the body has too little insulin or when the body can’t use insulin properly. Here are a few of the causes:
- Too much food, like a meal or snack with more carbohydrates than usual
- Not enoughinsulinor oral diabetes medications
- Side effects from other medications, such as steroids or anti-psychotic medications
- Illness, stress, menstrual periods or short or long-term pain
The good news is, there are things you can do to avoid highsand to treat them when you get them.
How Do People With Diabetes Monitor Blood Sugar Levels
“Some people with type 2 diabetes with good levels of control will need to monitor only several times a week and when sick or when their schedule changes,” Weisenberger explains.
Most people use a small hand-held monitor with glucose strips and a small needle to draw blood from a finger. Continuous glucose monitors are becoming more available and more popular. They allow the wearer to monitor their blood glucose levels 24/7, which is especially beneficial for people at risk of extreme highs and lows.
Don’t Miss: Rice For Diabetics Type 2
How To Use A Blood Glucose Meter:
- After washing your hands, insert a test strip into your meter.
- Use your lancing device on the side of your fingertip to get a drop of blood.
- Touch and hold the edge of the test strip to the drop of blood and wait for the result.
- Your blood glucose level will appear on the meter’s display.
Note: All meters are slightly different, so always refer to your user’s manual for specific instructions.
A1c And Cardiovascular Disease Outcomes
Cardiovascular Disease and Type 1 Diabetes
CVD is a more common cause of death than microvascular complications in populations with diabetes. There is evidence for a cardiovascular benefit of intensive glycemic control after long-term follow-up of cohorts treated early in the course of type 1 diabetes. In the DCCT, there was a trend toward lower risk of CVD events with intensive control. In the 9-year post-DCCT follow-up of the EDIC cohort, participants previously randomized to the intensive arm had a significant 57% reduction in the risk of nonfatal myocardial infarction , stroke, or cardiovascular death compared with those previously randomized to the standard arm . The benefit of intensive glycemic control in this cohort with type 1 diabetes has been shown to persist for several decades and to be associated with a modest reduction in all-cause mortality .
Cardiovascular Disease and Type 2 Diabetes
The glycemic control comparison in ACCORD was halted early due to an increased mortality rate in the intensive compared with the standard treatment arm , with a similar increase in cardiovascular deaths. Analysis of the ACCORD data did not identify a clear explanation for the excess mortality in the intensive treatment arm .
You May Like: Type 1 Diabetes Books For Parents
Keeping Blood Sugar Well Managed
What you eat can help keep your blood sugar better regulated whether you have diabetes, prediabetes or neither. Weisenberger advises people to “balance your food groups and your macronutrients at each meal. I prefer to do this with the Plate Method of meal planning.”
The American Diabetes Association created the Diabetes Plate Method to help people with diabetes plan their meals more practically. Nonetheless, people without diabetes can also use this method. Before beginning, you want to start with a dinner plate about 9 inches in diameter. If you need more calories than averagebecause you work out regularly, for exampleyou can use an 11- or 12-inch plate. In comparison, someone who needs fewer calories can use a smaller dinner plate of 8 inches in diameter. Remember that the number of calories you need depends on factors like age, height, sex, health conditions and exercise, among others.
- Step 1: Fill half your plate with nonstarchy vegetables.
Examples of nonstarchy vegetables include artichokes, beets, broccoli, cabbage, carrots, celery, radishes, tomatoes, turnips and salad greens. Nonstarchy vegetables do not have a significant effect on blood sugar levels.
- Step 2: Fill one-quarter of your plate with lean protein.
- Step 3: Fill the last one-quarter of your plate with carbohydrate foods.
- Step 4: Add water or another zero-calorie beverage to complete your meal.
- Step 5: Choose healthy fats in small amounts.
Glucose Assessment By Continuous Glucose Monitoring
Recommendations
-
6.3 Standardized, single-page glucose reports from continuous glucose monitoring devices with visual cues, such as the ambulatory glucose profile , should be considered as a standard printout for all CGM devices. E
-
6.4 Time in range is associated with the risk of microvascular complications, should be an acceptable end point for clinical trials moving forward, and can be used for assessment of glycemic control. Additionally, time below target and time above target are useful parameters for reevaluation of the treatment regimen. C
CGM is rapidly improving diabetes management. As stated in the recommendations, time in range is a useful metric of glycemic control and glucose patterns and it correlates well with A1C in most studies . New data support that increased TIR correlates with the risk of complications. The studies supporting this assertion are reviewed in more detail in Section 7 Diabetes Technology they include cross-sectional data and cohort studies demonstrating TIR as an acceptable end point for clinical trials moving forward and that it can be used for assessment of glycemic control. Additionally, time below target and time above target are useful parameters for reevaluation of the treatment regimen.
Also Check: Diabetes Feet Tingling At Night
Other Tips For Checking:
- With some meters, you can also use your forearm, thigh, or fleshy part of your hand.
- There are spring-loaded lancing devices that make sticking yourself less painful.
- If you use your fingertip, stick the side of your fingertip by your fingernail to avoid having sore spots on the frequently used part of your finger.
What Is Prediabetes
Prediabetes involves blood glucose levels that are higher than normal but not high enough to be classified as diabetes.
Prediabetes usually occurs in people whoalready have some insulin resistance or whose pancreas isnt making enough insulin to keep blood glucose in the normal range.
Studies show that most people with prediabetes develop type 2 diabetes within 10 years. This can be slowed by making changes in your diet and physical activity and losing a small amount of weight.
Like people with diabetes, those with prediabetes have increased risk of heart disease and stroke.
Also Check: Best Type 1 Diabetes Snacks
What Is Diabetes
Diabetes is a disease in which blood glucose, or sugar, levels are too high. More than nine in 10 cases are type 2 or adult-onset diabetes, the kind linked to excess body weight and physical inactivity.
In type 2 diabetes, your body does not produce or make good use of insulin, a hormone that helps glucose enter your cells to give them energy. Without enough insulin, the glucose stays in your blood and can lead to serious or life-threatening cardiovascular, kidney, and eye problems.
According to the American Diabetes Association, diabetes causes more deaths per year than breast cancer and AIDS combined. Having diabetes nearly doubles your chance of a heart attack.
The risk of death among people with diabetes is about twice that of people without diabetes of a similar age, according to the CDC. People with diabetes lose as many as 10-15 years of life on average. Diabetes is also a leading cause of new cases of blindness, kidney failure, and leg and feet amputations not caused by trauma.
Who Should Check
Talk to your doctor about whether you should be checking your blood glucose. People who may benefit from checking blood glucose regularly include those:
- taking insulin.
- having a hard time reaching your blood glucose targets.
- having low blood glucose levels.
- having low blood glucose levels without the usual warning signs.
- have ketones from high blood glucose levels.
Don’t Miss: Low Blood Sugar Pregnancy Symptoms
What About A1c
Your blood glucose isnt the only number that tells you how your diabetes management is doingyour A1C is important, too. So what is A1C?
This relatively simple blood test can tell you a lotit will give you a picture of your average blood glucose level over the past two to three months. The higher the levels, the greater your risk of developing diabetes complications. Your doctor will tell you how often you need the A1C test, but usually youll have the test at least twice a year if youre meeting your treatment goals.
How Do I Check
People with diabetes check their blood glucose levels by poking their fingertips and using a blood glucose meter or a continuous glucose monitor to measure the blood glucose level at that moment. Read on to find out how to use a blood glucose meter. To find out more about CGMs, start by talking to your doctor.
Read Also: Blue Cross Blue Shield Diabetic Supplies
Blood Glucose Sometimes Gets A Bad Rap But Its Not Always Bad
Blood glucose is an important number when it comes to diabetes management.
Many foods break down into blood glucose, which is used for energy to fuel our brain, heart and muscles. Blood glucose either comes from the food we eat or is made by the liver, and is found in the blood stream and inside the cells .
If you’re struggling to manage your blood glucose levels, youre not alone.
The good news is, with the latest tools and strategies, you can take steps to manage your blood glucose, prevent serious complications and thrive.
Correlation Between Smbg And A1c
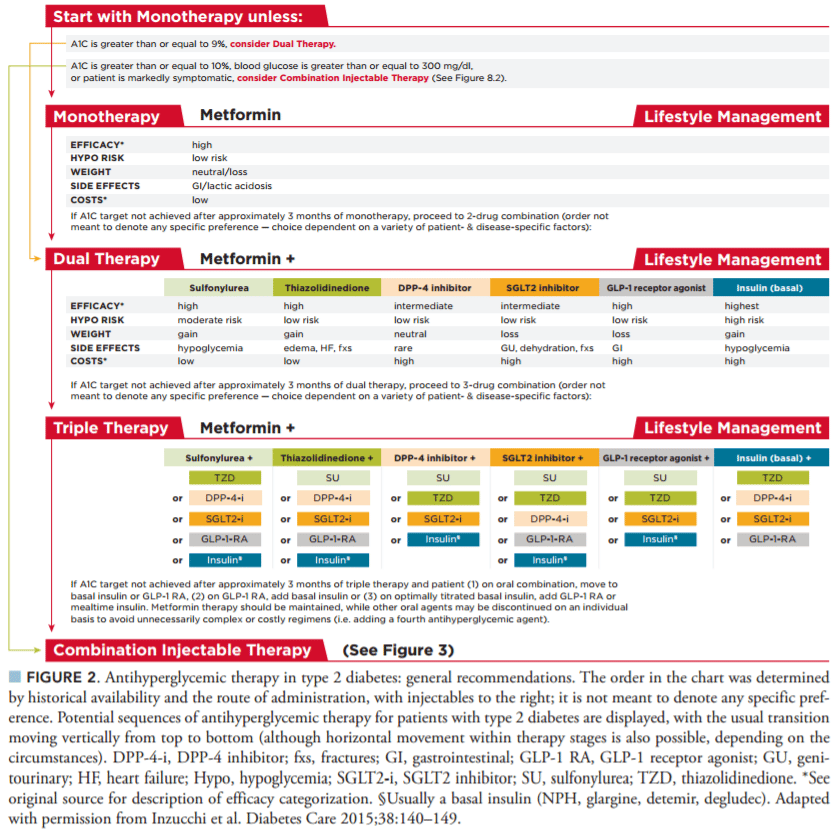
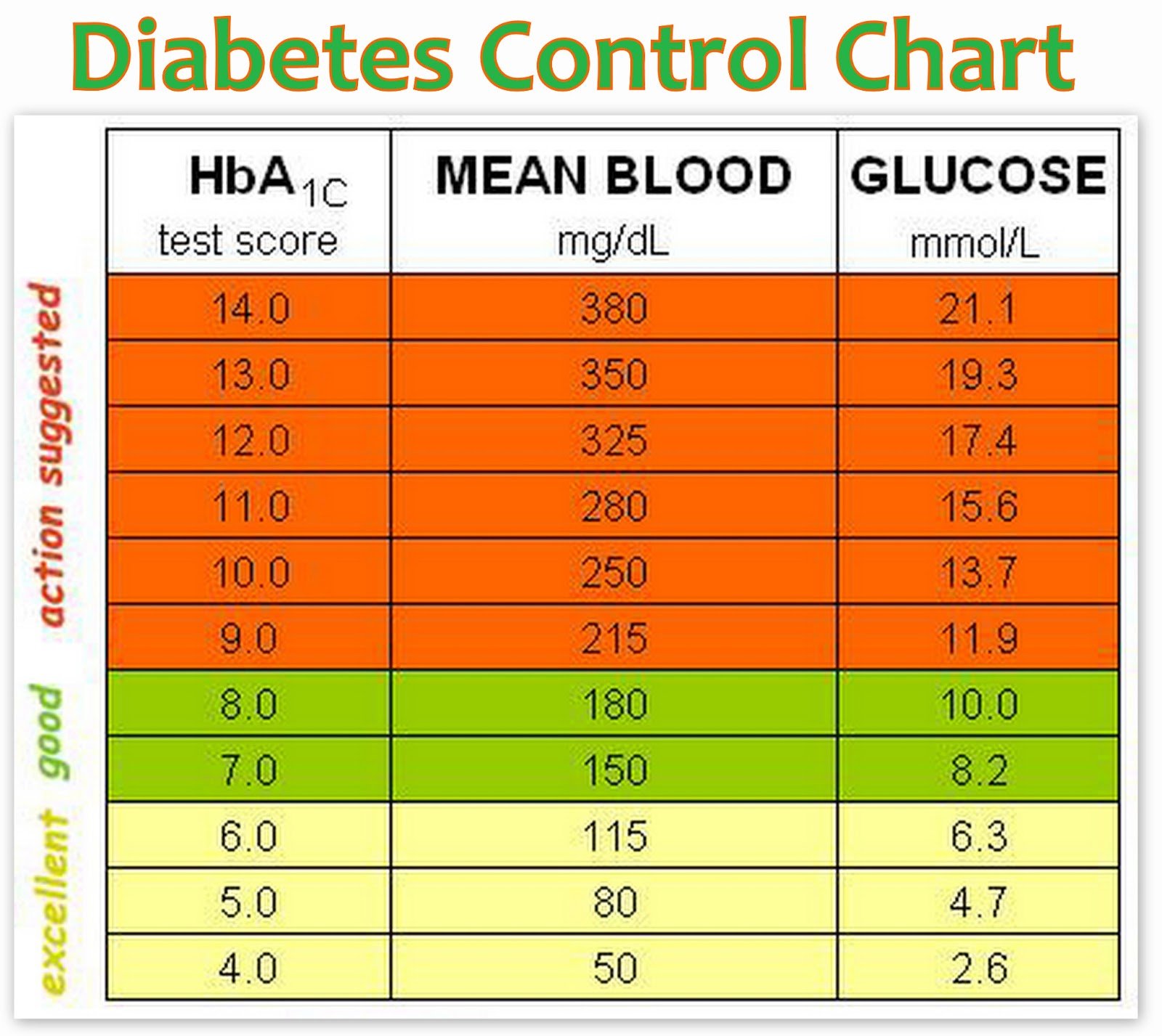
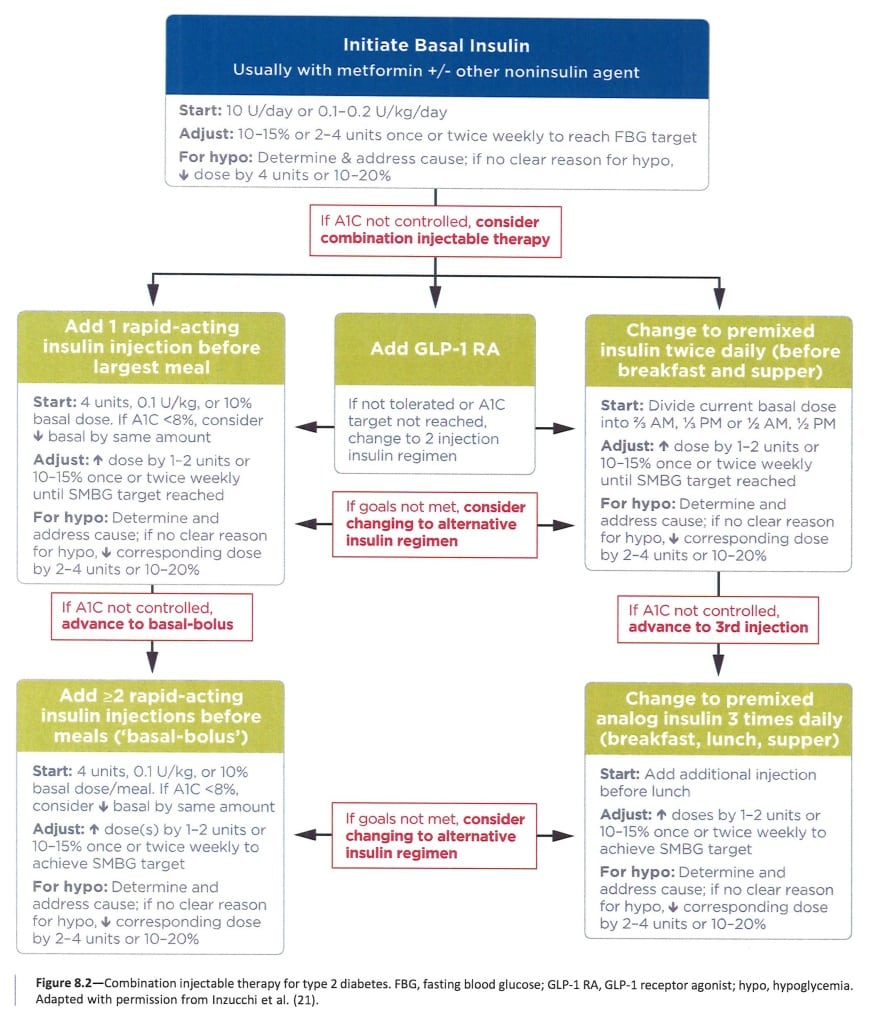
shows the correlation between A1C levels and mean glucose levels based on the international A1C-Derived Average Glucose study, which assessed the correlation between A1C and frequent SMBG and CGM in 507 adults with type 1, type 2, and no diabetes , and an empirical study of the average blood glucose levels at premeal, postmeal, and bedtime associated with specified A1C levels using data from the ADAG trial . The American Diabetes Association and the American Association for Clinical Chemistry have determined that the correlation in the ADAG trial is strong enough to justify reporting both the A1C result and the estimated average glucose result when a clinician orders the A1C test. Clinicians should note that the mean plasma glucose numbers in are based on 2,700 readings per A1C in the ADAG trial. In a recent report, mean glucose measured with CGM versus central laboratorymeasured A1C in 387 participants in three randomized trials demonstrated that A1C may underestimate or overestimate mean glucose in individuals . Thus, as suggested, a patient’s SMBG or CGM profile has considerable potential for optimizing his or her glycemic management .
Read Also: 2-nbdg Glucose Uptake Assay
Setting And Modifying A1c Goals
Numerous factors must be considered when setting glycemic targets. The ADA proposes general targets appropriate for many patients but emphasizes the importance of individualization based on key patient characteristics. Glycemic targets must be individualized in the context of shared decision-making to address the needs and preferences of each patient and the individual characteristics that influence risks and benefits of therapy for each patient in order to optimize patient engagement and self-efficacy.
The factors to consider in individualizing goals are depicted in . This figure is not designed to be applied rigidly but to be used as a broad construct to guide clinical decision-making and engage in shared decision-making in people with type 1 and type 2 diabetes. More stringent targets may be recommended if they can be achieved safely and with acceptable burden of therapy and if life expectancy is sufficient to reap benefits of stringent targets. Less stringent targets may be recommended if the life expectancy of the patient is such that the benefits of an intensive goal may not be realized, or if the risks and burdens outweigh the potential benefits. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals.
Why Would Someone Without Diabetes Monitor Blood Sugar
Dana Angelo White, M.S., RD, a cookbook author and owner of Dana White Nutrition, Inc., says she really doesn’t see the point of monitoring blood sugar if you don’t have diabetes. “As a temporary experiment, it may be interesting to monitor the blood sugar fluctuations that occur during meals, sleep and exercise. Seeing how your body responds appropriately may provide some reassurance and, of course, may help you make some changes .”
Read Also: Can Prednisone Cause High Blood Sugar
A1c And Microvascular Complications
Hyperglycemia defines diabetes, and glycemic control is fundamental to diabetes management. The Diabetes Control and Complications Trial , a prospective randomized controlled trial of intensive versus standard glycemic control in patients with type 1 diabetes, showed definitively that better glycemic control is associated with 5076% reductions in rates of development and progression of microvascular complications. Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications study demonstrated persistence of these microvascular benefits over two decades despite the fact that the glycemic separation between the treatment groups diminished and disappeared during follow-up.
The Kumamoto Study and UK Prospective Diabetes Study confirmed that intensive glycemic control significantly decreased rates of microvascular complications in patients with short-duration type 2 diabetes. Long-term follow-up of the UKPDS cohorts showed enduring effects of early glycemic control on most microvascular complications .
What Is Insulin Resistance
Insulin resistance is when cells in your muscles, fat, and liver cant use the insulin it makes. As a result, the pancreas produces more insulin to help glucose get into your cells. The CDC relates insulin to a key that lets sugar into cells for use as energy.
Eventually, your pancreas cant keep up with increased insulin production, causing blood sugar to rise. If you have insulin resistance, you want to become less insulin resistant which will allow your cells to better use insulin. This is where increased physical activity and weight loss come into play.
You May Like: Is Glucose The Same As Blood Sugar