Clinical Indications For Insulin Pump Therapy
Recent clinical guidelines from diabetes organizations worldwide, including the American Diabetes Association, the International Society for Pediatric and Adolescent Diabetes, the Endocrine Society, and the American Association of Clinical Endocrinologists/American College of Endocrinology state that insulin pump therapy may be beneficial for all individuals with type 1 diabetes, regardless of age . Individuals with type 1 diabetes who are not meeting glycemic targets or have high rates of hypoglycemia or hypoglycemic unawareness may benefit the most from pump therapy. Individuals with gastroparesis may also benefit from pump therapy, specifically from the ability to extend bolus delivery to manage the delayed rise in glucose from meals that occurs with gastroparesis. Finally, even individuals who are meeting their glycemic targets with an MDI regimen but who desire more flexibility in their type 1 diabetes management may find improvements in quality of life and treatment satisfaction when switching to insulin pump therapy. Insulin pump therapy is recommended for individuals with type 2 diabetes who are not meeting glycemic targets with MDI, oral medication, and lifestyle modifications .
Travelling With An Insulin Pump
While travelling, an accompanying letter on practice letterhead should be provided stating the medical history of the patient, including the diagnosis of type 1 diabetes, and that management is via an insulin pump. A list of current drugs, with generic names and doses, should be included. The letter should stress that it is important that the patients drugs accompany them, and that the insulin pump should not be disconnected. In particular, the pump should not be put through airport X-ray machines.
Prescriptions should be obtained for insulin and other drugs before travel. In case of pump failure both rapid-acting and long-acting insulin should be obtained along with injecting devices and needles. Sufficient equipment for glucose testing should be packed in the hand luggage. In addition to drugs and glucose-testing equipment adequate quantities of consumables should be packed. As a rule, pack twice as many sets as potentially required for the planned period away from home. An adequate supply of consumables should be included in the hand luggage while flying.
How We Choose Products
The Medical News Today vetting team has evaluated the products and brands below based on medical accuracy and integrity.
Insurance can often cover the price of the products, depending on an individuals plan.
A person should never purchase an insulin pump from a company that does not require a prescription.
Read Also: Recommended Foods For Type 2 Diabetes
Medtronic Minimed 630g System
For an integrated CGM
This model from Medtronic comes with an optional CGM so a person can also monitor their blood sugar levels using the same device. It is also compatible with the Contour Next Link 2.4 blood glucose meter.
Medtronic claims that this system makes a person four times more likely to reach their target A1C level, which is their average blood glucose level over about 3 months.
Other stand out features include:
- alarms if a person goes below their preset glucose levels the device will stop issuing insulin if a person does not respond
- a bolus calculator, which automatically calculates doses and tells a person if they set them too close together
- predictive alerts
- compatible app for smartphones, which displays all readings and allows for notifications and alarms
- suitable for those with type 1 or type 2 diabetes
Many insurance companies cover the Omnipod Dash. It is also available through pharmacies with a prescription.
Continuous Subcutaneous Insulin Infusion

Continuous subcutaneous insulin infusion can give a better quality of life .
There has been a systematic review of 11 studies of at least 10 weeks duration, comparing soluble insulin with the analogues lispro and, in one case, aspart in pumps . The analogue produced a small, significant improvement in HbA1c. There were no differences in hypoglycemia. Ketosis, hyperglycemia, and clogging were not common.
In 132 patients with type 2 diabetes using insulin randomly assigned to continuous subcutaneous insulin infusion or multiple daily injections of insulin aspart and NPH insulin) for 16 weeks, after 8 weeks training to establish optimal dosages there were more episodes of hyperglycemia with multiple daily injections. HbA1c was identical. Most of the patients who expressed a view wanted to stay on the pump.
In 40 patients aged 425 years with type 1 diabetes who were given continuous subcutaneous insulin infusion for 6 months the number of episodes of hypoglycemia was reduced by a half . There were two episodes of diabetic ketoacidosis. In 10 patients lipohypertrophy developed at the insertion site and three patients had signs of skin redness, which improved with local antibiotic treatment.
Sujoy Ghosh MD DM MRCP MRCPS, Andrew Collier BSc MD FRCP, in, 2012
You May Like: Just Diagnosed With Type 2 Diabetes
Benefits Of Insulin Pumps
Insulin pumps have many benefits over traditional insulin injection therapy. Research evidence shows that pumps are better at controlling blood sugar and cause fewer complications. People using insulin pumps have fewer episodes of severe hypoglycaemia and less than half the admissions for the serious complication of diabetic ketoacidosis. Insulin pump advantages include:
- Better diabetes control
- The pump is small and discreet usually smaller than a pack of cards
- Delivers a steady supply of insulin 24 hours a day
- You can add a bolus of insulin at meals quickly and easily
- The insulin is introduced through a cannula, meaning fewer injections
- You only need to change the cannula every 2-3 days
- Pumps simplify your regime because you only need rapid-acting insulin
Who Can Use An Insulin Pump
If you have type insulin-dependent diabetes, your doctor may recommend insulin pump therapy. Insulin pump therapy is also recommended for you if you have difficulty controlling your blood sugar with daily insulin injections to reduce your chance of hypoglycemia.
Do not get an insulin pump if you are pregnant or planning to become pregnant as the risk of ketoacidosis is higher during pregnancy.
Also, if you do not like having the machine in your pocket or on your belt or you do not want to frequently check your blood sugar then an insulin pump may not be right for you.
Also Check: How Can Diabetes Be Managed
Types Of Insulin Pumps
Insulin pump availability can vary depending on a variety of factors. Also, insulin pump manufacturers may introduce new pumps or enhanced models, and phase out older models.
Additionally, some pumps may be recommended for certain ages or types of diabetes. Its important to talk with your doctor about choosing a pump. This can ensure your pump of choice is the right option for you, your insulin needs, and your lifestyle.
Examples of commonly used insulin pumps include:
- Medtronic. Medtronic offers the Minimed 770G system and the Minimed 630G system .
- Omnipod. The Omnipod DASH system is a Bluetooth-enabled patch-based system that provides 3 days of nonstop insulin management. Children and adults can use the Omnipod for both type 1 and type 2 diabetes.
- Tandem.Tandem makes the t:slim X2 insulin pump. This pump is intended for people with type 1 diabetes who are ages 6 and older.
An insulin pump can be a convenient way of managing your blood sugar and keeping your diabetes well managed. Lets look at some of the key advantages.
How Do You Choose The Right Syringe For Injecting Insulin
If your highest dose is near the syringe’s maximum capacity, consider buying the next size up in case your dosage increases
If you measure your doses in half units, be careful to choose an appropriate syringe that has the right measurements
When youre traveling, make sure to match your insulin strength with the correct size syringe if you purchase new syringes in an unfamiliar place
Just as there are different sizes of syringes for administering insulin, there are also varying sizes of insulin needles. Shorter needles usually mean less sting when injecting. The downside is that the shallower the injection is, the longer it takes for the insulin to work. Your doctor will help you find the balance thats best for you.
Recommended Reading: How Does Diabetes Affect The Brain
Why Use An Insulin Pump
For people with type 1 diabetes, keeping blood glucose levels in normal range is the best way to prevent or delay complications of type 1 diabetes, but tight control can increase the risk of hypoglycaemia.
When a pump is used well it can help keep tight control without increasing the risk of hypos because it is so adaptable. Once long-acting insulin has been injected you cannot turn it off or slow it down, but basal insulin delivered by a pump can be slowed, stopped or increased for a few minutes or a few hours.
Boluses for snacks, meals and to correct high blood glucose levels can be delivered all at once, spread over a few minutes to a few hours, or split so some is given straight away and the rest is delivered over a span of time.
Pumps deliver insulin much more precisely than any available pen or syringe. Basal rates are adjustable down to lower than a tenth of a unit per hour, depending on the make of pump. The tiny doses of Insulin from a pump are more consistently absorbed than a larger amount from an injection where it is sometimes not absorbed properly causing glucose levels to run low or high for several hours.
Injected long-acting insulin can be absorbed differently every day-sometimes too quickly, sometimes too slowly, and sometimes only in part. This leads to variable control. With a pump and rapid acting insulin continuously delivering in tiny drops, absorption is much more reliable and your diabetes more stable and predictable.
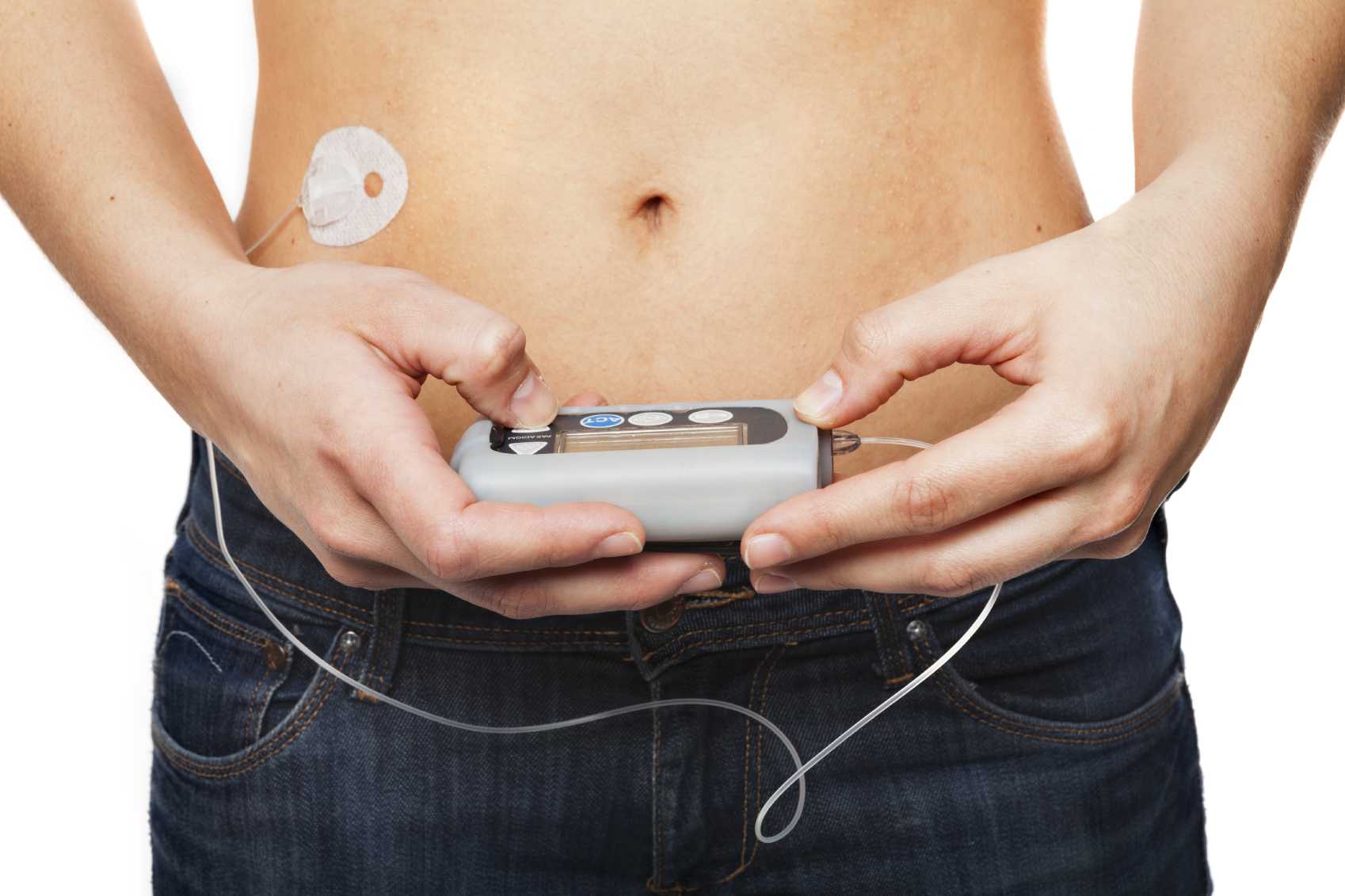
What Sort Of Insulin Pumps Are There
There are two types of insulin pump:
- A tethered pump uses a fine tube to connect the pump to the cannula the pump is worn in a pocket or clipped to a belt.
- A patch pump or micro pump has no tubing or a very short tube, and the pump is usually stuck on to the skin.
To find out what insulin pumps are currently available in the UK, visit Pumps and Infusion Sets Available in the UK.
Read Also: Psoriasis And Diabetes Type 1
Disposal Of Used Insulin Syringes
Used syringes, pen needles, cannulas and lancets must be disposed of in an Australian Standards-approved sharps container, which is puncture-proof and has a secure lid. These containers are usually yellow and are available through pharmacies, local municipal councils and state or territory diabetes organisations such as Diabetes Victoria.
Procedures to dispose of sharps containers vary from state to state.
For sharps disposal information and help, you can contact:
- state or territory diabetes organisations, such as Diabetes Victoria
- state Department of Health
Insulin needs to be stored correctly. This includes:
- Store unopened insulin on its side in a fridge.
- Keep the fridge temperature between 2 and 8 °C.
- Make sure that insulin does not freeze.
- Once opened, keep it at room temperature for not more than one month and then dispose of it safely.
- Avoid keeping insulin in direct sunlight.
Extreme temperatures can damage insulin so it doesn’t work properly. It must not be left where temperatures are over 30 °C. In summer your car can get this hot so don’t leave your insulin there.
There are various insulated insulin carry bags available for transporting insulin.
What Are The Benefits Of Using An Insulin Pump
People who use an insulin pump:
- no longer need injections
- often find it easier to keep their glucose levels in their target range
- can adjust their insulin to match their activity level
- rely on their pump to dose insulin precisely
- can get added safety if they connect their pump to their . When its connected, the pump can respond more quickly to changes in sugar levels.
Using a pump gives a person flexibility. They can choose injections instead of the pump anytime. Some people like to take a break from their pump from time to time.
You May Like: Where Do You Give Insulin Injections
How Do You Take Insulin Without A Syringe
There are several options:
-
Insulin pens look like large writing pens and can help prevent under- and overdosing. They also dont require refrigeration, are conveniently prefilled, and are more durable than syringes.
-
Insulin pumps are attached to a thin tube thats implanted under your skin. Pumps are computerized or motorized, and some models also act as glucose monitors. They deliver insulin before each meal along with small amounts through the course of the day. In the US, about 60% of people with diabetes use some form of .
-
Jet injection devices are a good option if you hate needles. A jet injector holds several doses of insulin. After placing it against your skin, you press a button, and the insulin is pushed through.
-
Inhaled insulin comes in a pre-measured inhaler and was first approved in 2014. Its short-acting and usually not covered by insurance, which makes it more cost prohibitive than other types of insulin for most people with diabetes.
Unless you have an insulin pump that also works as a glucose monitor, insulin dosing is based on self-monitoring your blood glucose levels. You can check them by doing finger pricks or wearing a device that continuously monitors them for you.
What Causes Someone To Be Prescribed Insulin
If your body doesnt make insulin or doesnt make enough, you are eventually diagnosed with type 1 diabetes. It used to be called juvenile diabetes, but new estimates show that as many as half of people with type 1 diabetes are not diagnosed until adulthood. On the other hand, if your body doesnt use insulin properly, you have type 2 diabetes.
While people with type 1 diabetes need to take insulin to survive, many people with type 2 are able to stave off insulin use or even avoid it altogether by exercising, losing weight, adapting healthier eating habits, or using other prescription medications.
Don’t Miss: Is Type 1 Diabetes Genetic
Insulin Pumps With Hypoglycemia Suspension
After the advent of SAP, further integration of pumps with CGM devices occurred with hypoglycemia suspension technology. In hypoglycemia suspension systems, the insulin pump not only displays the sensor glucose values, but also automatically suspends insulin delivery in response to hypoglycemia or anticipated hypoglycemia, based on CGM data, in an effort to prevent low blood glucose levels . This additional layer of protection against hypoglycemia is vital, as severe hypoglycemia remains the most concerning acute complication of intensive insulin therapy .
What Is An Insulin Resistance Diet
An insulin resistance diet is often recommended for people who have insulin resistance, a key component of type 2 diabetes. It incorporates foods that will help maintain your bodys balance of insulin and blood sugar. Think nourishing calories from veggies, fruit, lean proteins, and healthy fats.
-
The History of a Wonderful Thing We Call Insulin.
-
Increasing Insulin Affordability.
-
General Overview of Type 1 and Type 2 Diabetes and Resources for Patients/Families: The American Diabetes Association:
-
General Overview of Type 1 Diabetes and Resources for Patients/Families: The Juvenile Diabetes Research Foundation :
-
Table of Non-insulin Medications:
-
American Diabetes Association. Get a Handle on Diabetes Medication
-
Joslin Diabetes Center. Managing Diabetes: Insulin A to Z: A Guide on Different Types of Insulin..
-
Mayo Clinic. Diabetes treatment: Using insulin to manage blood sugar.
Recommended Reading: Whats A Good A1c For A Type 2 Diabetes
Managing Insulin Pumps In General Practice
The management of a patient on an insulin pump requires the involvement of a specialist diabetes team including an endocrinologist, diabetes nurse educator and dietitian. The GP is an essential member of this team and it is therefore important GPs understand the terminology related to insulin pump therapy .3
What Does An Insulin Pump Do
An insulin pump is intended to imitate the functions of a human pancreas. Your pancreas releases insulin in response to changes in your blood sugar level. But when you have diabetes, your body doesnt release insulin or use it properly. As a result, you have to find another way to get the insulin you need.
Insulin pumps work by delivering a basal, or set, rate of insulin through a tube called a cannula. The cannula is inserted just under the top layer of your skin. Your doctor will work with you to determine the amount of insulin you need each day.
Insulin pumps can also deliver an insulin bolus. This is an extra dose of insulin besides your basal rate. A pump wont automatically give you this extra dose of insulin, though. You need to tell the pump to administer the bolus dose.
Insulin pumps give you insulin according to how you program them. They dont adjust on their own to your changing insulin levels. Some pumps can, however, adjust basal rates based on the blood sugar reading of a continuous glucose monitor.
They require special training on your part to make sure you can use them safely and effectively.
An insulin pump is usually about the size of a deck of cards, although the size can vary depending on the model. You wear the pump outside your body.
The pump usually consists of:
- a display screen
- a place for an insulin container
- a thin cannula, or tube, that attaches to your body
Innovations in pump technology mean that some pumps have extra features, such as:
Don’t Miss: Meal Prep Recipes For Diabetics
Pump Benefits For Type 2 Diabetes
Increased flexibility in scheduling daily activities such as meals, exercise, and social activities may be the main reason for you to consider using an insulin pump if you have Type 2 diabetes. There is also the potential for tighter blood glucose control and a reduced risk of diabetes complications.
Diabetes complication risk. According to the United Kingdom Prospective Diabetes Study , tight control of blood glucose in people with Type 2 diabetes helps to delay or prevent the development of microvascular complications such as retinopathy , nephropathy , and neuropathy . Simply using an insulin pump is no guarantee of tight blood glucose control, of course, but studies have shown that pumps can help people to achieve control that is at least comparable to that of people on insulin injection regimens.
In addition to the benefits of tight blood glucose control, the UKPDS showed that tight blood pressure control can reduce risks of cardiovascular diseases for people with diabetes. Although high blood pressure is more of a proven contributor to heart disease and stroke than high blood glucose levels, getting better control of your blood glucose may help to reduce at least one risk factor for cardiovascular disease.