Dont Inject The Insulin Too Deep
Insulin is supposed to be injected into the fat layer under the skin using a short needle. This is referred to as a subcutaneous injection.
If you inject the insulin too deep and it enters your muscle, your body may absorb it too quickly. The insulin might not last very long and the injection could be very painful.
What Are The Different Types Of Insulin
The American Diabetes Association characterizes insulin by how fast it works. But everyones body is different. If you have diabetes, you should expect deviations in the amount of time any medication takes to reach your bloodstream.
Here are 8 different types of Insulin and how they work.
- Onset is defined as the length of time before insulin hits your bloodstream and begins to lower blood glucose.
- Peak is the time during which insulin is at its maximum effectiveness at lowering your blood glucose levels.
- Duration is the length of time insulin continues to lower your blood glucose levels.
- Rapid-acting insulin begins to affect blood glucose approximately 15 minutes after injection. It peaks in about an hour, and then continues to work for a few more.
- Short-acting insulin reaches your bloodstream within 30 minutes of injection. It peaks in the 2-3-hour range and stays effective for 3-6 hours.
- Intermediate-acting insulin includes NPH insulin which helps control glucose for 10-12 hours. A protamine is a type of protein that slows the action of this insulin.
- Long-acting insulin enters the bloodstream 1-2 hours after injection and may be effective for as long as 24 hours. An advantage to long-acting insulin is there is no pronounced peak, and it works more like typical pancreatic insulin.
- Premixed/combination insulin contains a mix of rapid- or short-acting insulin combined with an intermediate-acting insulin. This eliminates the need to draw insulin from more than one bottle.
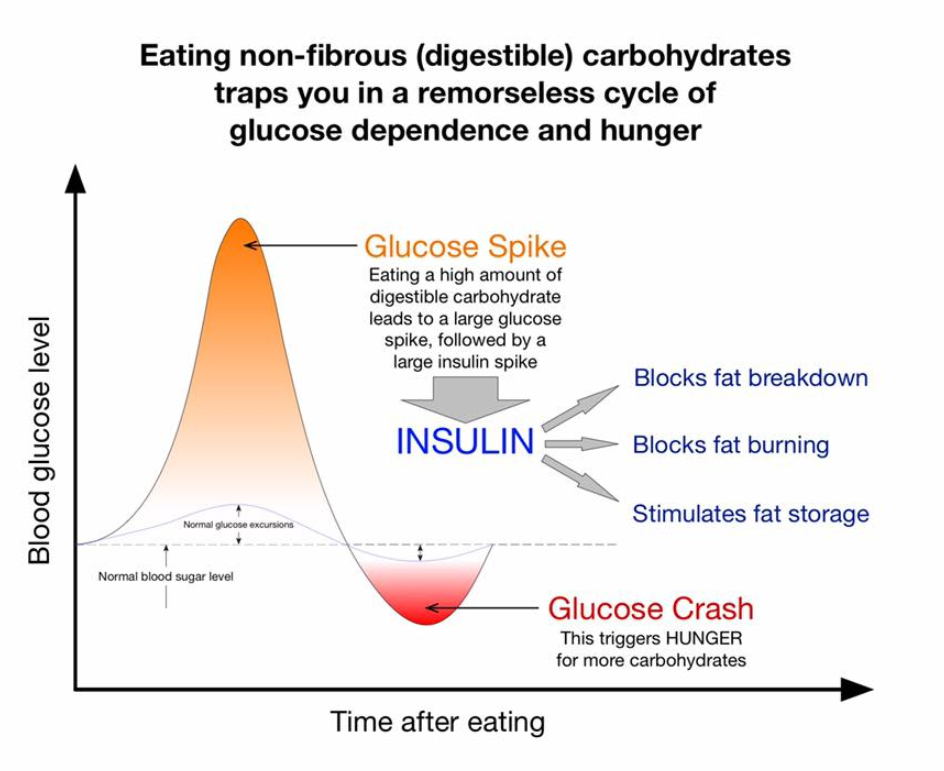
Why Is It Important To Reduce The Size And Duration Of These Spikes
Reducing these spikes may help you to increase the amount of time you spend in your target blood sugar range , which will have a positive impact on your future health. You should consult your healthcare team to understand the best target range for you, as this will differ from person to person. However, the International Society for Paediatric and Adolescent Diabetes recommends a target of 5.0-10.0 mmol/L .
Symptoms of a high blood sugar level also vary in individuals, but they may cause you to feel thirsty, tired, stressed and need to go to the toilet a lot. In the short term, by avoiding prolonged high blood sugar readings after eating, you should also reduce the occurrence of these symptoms and improve your energy, cognitive and athletic ability and overall mood.
You May Like: When Is Insulin Prescribed For Type 2 Diabetes
Why Do People Get Blood Sugar Spikes After Meals
When people eat a meal, especially when it contains carbohydrates, it is normal for them to have a temporary spike in their sugar level before the insulin their body produces immediately starts working to lower the spike. For someone with type 1 diabetes, who cant produce their own insulin, these spikes can be higher and last longer.
This is because it can take longer for the type of insulin they inject to start working, in comparison to the insulin that is produced naturally by the body of someone who does not have diabetes, to reduce these post-meal spikes.
Furthermore, it is important to know that people living with type 1 diabetes may have alterations in different digestive enzymes which will cause faster digestion of our meals . This can obviously impact on the size of the spike too.
Mealtime Insulin Vs Other Types Of Insulin
Mealtime insulin works differently than other types of insulin. The major difference between the different types of insulin is how quickly they start acting in the blood and how long theyre effective. Heres a breakdown:
- Rapid-acting insulin, sometimes called bolus insulin, is designed to quickly act on blood sugar during a meal. The effects of this type of insulin can start in as little as five minutes and peak after about an hour. It works for roughly three hours.
- Regular insulin begins to work 30 minutes after injection, peaks around two hours after the injection, and works for between five and eight hours.
- Long-acting insulin, also called basal or background insulin,works in your body throughout the day to control your blood sugar, even when youre not eating. The effects usually start about two to four hours after injection, and last for between 18 and 42 hours, depending on the exact brand of basal insulin.
- Intermediate-acting insulin is similar to a long-acting insulin, except it doesnt work for quite as long. It reaches the bloodstream about two hours after injection and is effective for about 12 to 16 hours. Youll have to take more doses of an intermediate-acting insulin throughout the day.
- Combination or mixed insulin, also known as basal-bolustherapy, includes both a long-acting insulin and a rapid-acting insulin in the same vial. An injection more closely imitates how the bodys insulin would naturally work throughout a typical day.
Also Check: Low Blood Sugar At Night Without Diabetes
Different Approaches To Managing Blood Sugar After Eating
Each persons body is different, and responds to insulin in a different way. There is no one-size-fits-all insulin treatment.
So, even after youve counted your carbs and figured out how much to inject, there is still another way to influence your blood sugar level after eating. Namely, try different methods and time-periods for injecting.
The common method is to inject before eating. Rapid-acting insulin requires injections 5-15 minutes before eating. Those minutes are the time it takes for insulin to enter the bloodstream. That way, your body will be ready for digestion once eating has begun.
After entering the bloodstream, rapid-acting insulin peaks after 1 hour this is when it is most effective at lowering the blood sugar level after eating.
This insulin will remain effective for 2-4 hours in the body. Find out whether those minutes and hours work best for you by trial-and-error and consulting with a doctor.
If not, splitting the bolus is another route to more efficient insulin treatment. This is especially useful if eating fatty food, such as takeaway pizza or curry.
This means taking a portion of the insulin before eating, and a portion after eating. Again, this is trial-and-error. Experiment and speak to a doctor.
Its always good for a person with diabetes to know what is going on with their body. So, when trying different methods, remember to keep testing. And keep testing even when sticking to the same routine.
Do Count Your Carbs Before Using Mealtime Insulin
The amount of mealtime insulin you need to inject is based on the number of servings of carbohydrates you plan on eating during a meal. Over time, youll get better at figuring out your carb intake. In the meantime, a dietitian can help you come up with a meal plan that works for you.
There are also several smartphone applications and internet-based calculators available to help you figure out your carb intake and your corresponding insulin dosage.
Hypoglycemia can happen when you take the wrong insulin dose, dont eat enough carbs right after taking your insulin, exercise more than usual, or when youre stressed.
You should take the time to learn the signs and symptoms of hypoglycemia, including:
- tiredness
- seizures
- loss of consciousness
You should also learn how to manage hypoglycemia if it happens to you. For example, you can eat or drink glucose tablets, juice, soda, or hard candies. You should also be extra cautious after vigorous exercise, as it can lower blood sugar for hours after the workout.
Recommended Reading: Can You Eat After Taking Insulin
Evidence From Pharmacokinetic And Pharmacodynamic Studies
Pharmacokinetic studies carried out in people with Type 1 diabetes show that all three rapidacting insulin analogues have similar PK and pharmacodynamic profiles , . They demonstrate peak plasma insulin concentrations approximately double those of RHI, and a time to maximum concentration less than half that of RHI, with concentrations of the analogues falling more rapidly, returning to levels < 20% of peak concentrations at about 4 h , , .
Pharmacokinetics of bolus insulins. Panels , and are reproduced from Home et al. Diabetes Obes Metab 2012 14: 780788. Panel is reproduced with permission from Andersen et al. EASD 2016 ePoster #931. Panels and are reproduced from Heise et al. Diabetes Obes Metab 2015 17: 682688 , under a Creative Commons licence. s.c., subcutaneous.
You May Like: Pancreatic Alpha Cell
Always Choosing The Same Spot To Inject Insulin
Insulin is absorbed at different rates depending on where you inject it. It enters your blood fastest when you inject it into your abdomen, a little more slowly when you inject it into the upper arms, and even more slowly when you inject it into the thighs and buttocks, according to the ADA. Youll get the best results by injecting your basal or bolus insulin into the same general body area, but rotating the side of the body where you inject if from day to day. Injecting insulin in the same spot over and over can cause hard, fatty lumps to form. These lumps don’t absorb insulin well. “You could be injecting your usual dose of insulin into one of these areas but potentially 50 percent or less of the insulin is absorbed,” Port says. She recommends checking for these hard lumps from time to time.
For more on how to use insulin properly, check out Diabetes Daily’s article “Habits of a Great A1C: Insulin Use Strategies”!
Recommended Reading: How Do I Control My Diabetes
Why They Happen And How To Try And Reduce Them If You Live With Type 1 Diabetes
Living with type 1 diabetes requires you to regularly check your blood sugar levels before you eat. However, we may not always consider what happens to our sugar levels immediately after we eat where it is very normal for people who dont have diabetes, let alone those who do, to temporarily have high sugar levels. Given that having high sugar levels can give you symptoms like thirst, tiredness and needing to go to the toilet a lot, learning about ways to try and reduce spikes in your sugar levels after meals may make a difference to your overall health and wellbeing.
Blood Sugar After Eating How To Manage It Better
Hi. My name is Christina and I am a nurse specialized in diabetes and also one of the co-founders of Hedia. Let me give you my advice on how to manage blood sugar after eating in this short video or check out my more detailed advice below the video.
As a nurse, and as a family member of a person with diabetes, I have seen first-hand how much must be considered with managing blood sugar after eating.
From that experience, I also know that diabetes doesnt need to take over your life. I have studied the importance of taking a positive approach to diabetes I want you to know that everything with diabetes can be tackled.
This includes blood sugar after eating. Understanding why you might have high blood glucose/sugar after eating is a hurdle that others without diabetes might not need to think about.
However, once you have that knowledge under your belt, you will have the confidence to know that you control your diabetes not the other way round!
To get control of that blood sugar level after eating, we should first look at what happens with the body. From this we can get an understanding of different approaches to handling that after-meal spike, as well as some often overlooked aspects.
You May Like: Diabetes And Metabolism Impact Factor
Diabetes Patients Can Eat Immediately After Taking Insulin
People with type 2 diabetes no longer have to wait to eat after taking insulin.
People with type 2 diabetes are sometimes told to wait after using insulin for the drug to work its way into the body before they can begin eating, but a new study from Germany indicates that it is not necessary to wait.
In a group of about 100 diabetics, researchers found that blood sugar levels remained steady regardless of whether or not participants left a 20 to 30-minute gap between using insulin and eating a meal. The diabetics overwhelmingly preferred being able to eat right away, too.
The result of the study can lead to better adherence and satisfaction.
Injectable insulin is available for diabetics in a newer fast-acting form, but its expensive and many still use human insulin, which takes some time to become active in the body. So doctors often recommend waiting to eat after using human insulin to prevent blood sugar spikes.
Not all experts think waiting is necessary, though, according to the researchers led by Nicolle Mueller of Universitätsklinikum Jena. To see what difference it makes, Mueller and her colleagues randomized type 2 diabetics into two groups.
Using a blood test that measures average glucose levels over time, the researchers found that all the participants had generally higher than ideal blood sugar levels but the difference in those levels between periods when they waited or didnt wait to eat after insulin injections was a negligible 0.08 percent.
Learn More About Treatment Approaches> >
Basal insulin. Small amounts of insulin are released by the pancreas 24 hours a day. On average, adults secrete about one unit of insulin per hour regardless of food intake.
Bolus insulin. In response to food, larger amounts of insulin are secreted and released in two-phase boluses. The first phase starts within minutes of the first bite of food and lasts about 15 minutes. The second phase of insulin release is more gradual and occurs over the next hour and a half to three hours. The amount of insulin that is released matches the rise in blood glucose from the food that is eaten.
In people with normal insulin secretion, insulin production and release is a finely tuned feedback system that maintains blood glucose between about 70 mg/dl and 140 mg/dl at all times, no matter what or when a person eats or when he engages in physical activity. During illness, when insulin needs may rise, the pancreas just produces more.
People whose pancreas does not secrete insulin normally often must inject insulin or infuse it with an insulin pump. People who have Type 1 diabetes, in which the pancreas secretes no insulin or virtually no insulin, must inject or infuse insulin. But learning when to take insulin and how much to take is challenging, because injected or infused insulin does not act exactly like insulin released from the pancreas. The first step to figuring out when to take insulin and how much to take is understanding an insulins action curve.
Also Check: How Do You Know If You Have Gestational Diabetes
Why Is Metformin Taken After Food
Metformin may show some side effects in the first few weeks of medication. Doctors recommend taking it after a meal as it proves to be beneficial in reducing the symptoms of bowelâs side effects.
Dr. SM Kamal Hasan, MBBS, Rangpur Medical College and HospitalRangpur- Dinajpur Highway, Cantt, Near Central Jail, Rangpur 5400, Bangladesh
Also Check: How Much Does Metformin Lower Blood Glucose
Injecting Insulin With An Insulin Pen:
Also Check: Purpose Of Insulin In The Body
Avoiding Injection Bruises And Lumps
Bruising can happen when you catch a tiny blood vessel under the skin where you have injected. It is quite normal for this to happen occasionally when you are injecting regularly and youre not doing anything wrong.
If you are concerned, you could make an appointment with your diabetes specialist nurse who will be able to do a review of your injection technique. In some cases, bleeding and bruising can be reduced by something as simple as using a different sized needle or changing your needle after each injection.
Some people notice hard lumps that can form if you inject in the same place too often. This might be lipohypertrophy , or could be something called cutaneous amyloidosis. These lumps can stop the insulin from working properly, so make sure you rotate where you inject and choose a different spot each time. If you notice any lumps, especially if they’re not going away, speak to your healthcare professional for more advice.
Other side effects from injecting a lot can be itching, rashes and other skin irritations. Changing where you inject helps with this too. You can also get treatments from your local pharmacy that can will help with the irritation.
Do Tell Friends And Family That Youre Taking Insulin
Its a good idea to teach your friends, colleagues, and family members about insulin and its potential side effects. If you do end up taking too much insulin and having a hypoglycemic episode, they should know how to help.
If you become unconscious, a friend or family member can give you a shot of glucagon. Talk to your doctor about keeping a supply of glucagon on hand and learning when and how to use it.
Don’t Miss: What Is Good For Diabetic Dry Skin