Reducing Your Risk Of Diabetic Retinopathy
To prevent retinopathy or prevent it from getting worse, keep your blood sugar, blood pressure, and blood cholesterol within a healthy range.
Follow the ABCDEs of staying healthy with diabetes to reduce the risk of eye damage.
A A1C Most people should aim for an A1C of 7%* or less by managing blood sugars well. A1C is a blood test that is a measure of your average blood sugar level over the past 120 days.
B Blood pressure Control your blood pressure to less than 130/80* mmHg.
C Cholesterol The LDL cholesterol target is less than 2.0* mmol/L.
D Drugs to protect your heart Speak with your health-care team about medications.
E Exercise & Eating Regular physical activity, healthy eating, and maintain a healthy body weight.
S Screening for complications Ask your health-care team about tests for your heart, feet, kidneys, and eyes.
S Smoking cessation Stop smoking and seek support for help with quitting.
S Self management, stress, and other barriers Set goals for yourself to reach the targets and live well with diabetes, such as managing stress effectively.
* Discuss your target values with your health-care team. Note that A1C targets for pregnant women, older adults and children 12 years of age and under are different
For more information about diabetic retinopathy, visit the Canadian National Institute for the Blind .
To find a CAO optometrist in your area, visit the Canadian Association of Optometrists.
Prevention Is Still The Best Cure
Because there is no cure for diabetes or diabetic retinopathy, the best way to treat these conditions is to stay on top of your health. Taking care of yourself and following your doctors instructions can help you prevent comorbid conditions from developing.
High blood glucose, hypertension, and high ketone levels can increase your risk of retinopathy. As such, managing them is the first step in prevention.
Even though its difficult, eating a healthy diet and exercising will go a long way toward keeping your eyes healthy in the long run. Along with diet and exercise, monitoring your blood sugar levels and taking your medication as prescribed can help as well.
Finally, the importance of frequent eye exams cant be stressed enough.
If you have diabetes, seeing an eye doctor every few months can help you stop retinopathy in its tracks. You should also get a thorough exam with dilation every year. Your doctor may then be able to notice and treat the damage before you experience any symptoms.
Swelling Of The Eye Lens
Another potential effect from diabetes is swelling of the eye lens, leading to blurry vision. If your blood sugar levels change quickly from low to normal, the shape of your eyes lens can be affected and your vision can be blurred. Your vision goes back to normal after your blood sugar stabilizes. If youre getting eyeglasses, make sure your blood sugar levels are controlled before your exam so that you can get the most accurate glasses prescription, says Cai.
You May Like: Non Insulin Injectables For Diabetes
How Can Diabetes Affect Your Eyes
Diabetes occurs when your body does not properly process food as energy. When you have diabetes, your body either does not respond to or does not produce insulin, which is a hormone that delivers glucose to the cells in your body. Having too much glucose in the bloodstream, outside the cells where it belongs, can lead to damage of the blood vessels and nerves that run throughout your body, including to the eyes.
How The Eye Works
To understand what happens in eye disorders, it helps to understand how the eye works. The eye is covered with a tough outer membrane. The covering in front is clear and curved. This curved area is the cornea, which focuses light while protecting the eye.
After light passes through the cornea, it travels through a space called the anterior chamber , through the pupil , and then through a lens that performs more focusing. Finally, light passes through another fluid-filled chamber in the center of the eye and strikes the back of the eye, the retina.
The retina records the images focused on it and converts those images into electrical signals, which the brain receives and decodes.
One part of the retina is specialized for seeing fine detail. This tiny area of extra-sharp vision is called the macula. Blood vessels in and behind the retina nourish the macula.
Recommended Reading: Can Type 2 Diabetics Get Dka
Two Other Complications Of The Eye: Cataracts And Glaucoma
Diabetes can also cause two other types of eye damage unrelated to the retina:
Cataracts are a condition of the lens the transparent, curved structure at the front of the eyeball that refracts and focuses light on the retina, just like a camera lens. A cataract is a dark or cloudy area of the lens that can make it more difficult to see clearly.
Cataracts are common as we age, but they are much more common in people with diabetes. A meta-analysis found that people with type 2 diabetes are about twice as likely to have cataracts.
The most significant risk factor for cataracts may be the duration of diabetes, although blood sugar control is also likely to be important, as well as age, family history, smoking, and exposure to sunlight. Corticosteroid treatments, occasionally used for diabetic retinopathy, can also cause cataracts.
The only medical treatment for cataracts is surgery, which is usually safe and effective.
Glaucoma is a more serious complication. In glaucoma, damage occurs in the optic nerve rather than the retina. The optic nerve is a bundle of nerve fibers that connects the eye to the brain. Glaucoma typically results in a loss of peripheral vision but can progress toward blindness.
Glaucoma is also common as we age, but diabetes can make its development more likely, possibly when high amounts of blood sugar cause vascular and neuronal injury. A meta-analysis found that people with diabetes are about 36 percent more likely to develop glaucoma.
Diabetes And Eye Damage
The formation of a cloudy layer occurs within the lens of the eye. You should consult with your ophthalmologist for an eye evaluation. A cataract may lead to blurry vision. People with diabetes are more susceptible to cataracts. Other symptoms of cataract include:
- Light sensitivity
- Regular use of tobacco
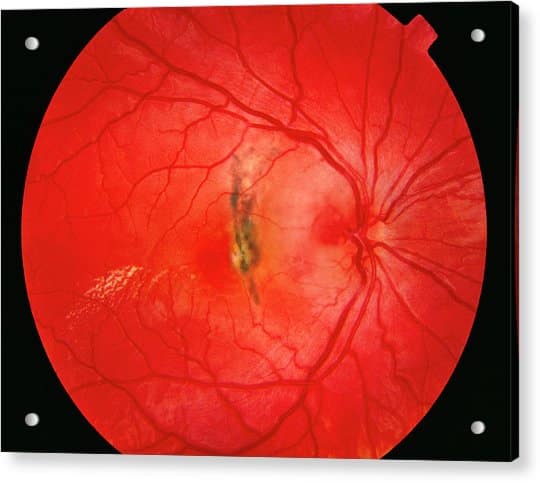
Diabetic retinopathy can lead to other serious eye problems. Problems associated with diabetic retinopathy are:Diabetic macular oedema People with diabetic retinopathy have a high risk of developing DME. It happens due to the swelling of the macula and leakage of fluid. It may lead to blurry vision.Neovascular glaucoma Diabetic retinopathy can cause the development of abnormal blood vessels from the retina into the angle of anterior chamber of the eye. It blocks the fluid to drain out from the eyes.Retinal detachment Diabetic retinopathy can cause the formation of scars in the back of the eye. The pulling of the retina from its base is called tractional retinal detachment.
You May Like: Men’s Insulin Pump Underwear
The Iris Solution For In
IRIS serves healthcare providers by offering an easy-to-use preventative screening measure that can be integrated into any healthcare organizations workflow, but our solution is also ideal for in-home evaluation providers looking to improve their preventive screening measures. The IRIS solution helps insurance payors and in-home healthcare providers meet diabetic patients where they are in their health journey and close gaps in patient care more effectively and efficiently.
The IRIS solution is one of the best ways insurance payors and other organizations who leverage health risk assessments can offer a preventative screening exam for diabetic retinopathy as a part of their in-home screening procedures. Improved quality of care, especially in the home setting, can lead to lower overall costs and a positive change in HEDIS/Star compliance.
Reach out today to see how IRIS can improve your patient care.
SM066 Rev. B
The Four Stages Of Diabetic Retinopathy
DR is defined by four stages. If youve been diagnosed with DR, its important to know which stage youre at.
The following is a direct quote from the American Diabetes Association position statement on diabetic retinopathy, with definitions adapted from the National Eye Institute:
Mild non-proliferative retinopathy . Small areas of balloon-like swelling in the retinas tiny blood vessels, called microaneurysms, occur at this earliest stage of the disease. These microaneurysms may leak fluid into the retina.
Moderate NPDR. As the disease progresses, blood vessels that nourish the retina will swell and distort even more. They may also lose their ability to transport blood. Both conditions cause characteristic changes to the appearance of the retina and may contribute to diabetic macular edema .
Severe NPDR. Many more blood vessels are blocked, depriving blood supply to areas of the retina. These areas secrete growth factors that signal the retina to grow new blood vessels.
Proliferative diabetic retinopathy . At this advanced stage, growth factors secreted by the retina trigger the proliferation of new blood vessels, which grow along the inside surface of the retina and into the vitreous gel . The new blood vessels are fragile and this causes them to bleed easily. Accompanying scar tissue can contract and cause retinal detachment the pulling away of the retina from underlying tissue.
Read Also: List Of Insulins For Diabetes
Who Is At Risk For Diabetic Retinopathy
Anyone with diabetes, whether its type 1, type 2, or gestational, can develop diabetic retinopathy. The better a patient controls their blood sugar, the less risk there is. But the longer a patient has diabetes, the more likely it is to occur. The early diabetic retinopathy stages are the best time to detect and treat the disease, which means that both diabetic patients and healthcare providers alike should take advantage of retinal imaging that catches the disease in its earliest stages.
Researchers have found that nonproliferative diabetic retinopathy was present in 25% of patients 5 years after they were diagnosed with diabetes, 60% at 10 years, and 80% at 15 years. These studies also found that the incidence of proliferative diabetic retinopathy varied from 2% in those who had diabetes for less than 5 years to 15.5% in those who had diabetes for 15 or more years.
While diabetic retinopathy is a common risk all diabetic patients face, technological advancements in the medical field have now made retinal screenings more accessible, which in turn will help to shorten diagnoses timelines and help provide better quality care. Taking precautionary measures to put an end to preventable blindness should be top-of-mind for both providers and patients.
Recovery After Retinal Detachment Surgery
Thinking about life after retinal detachment surgery, there will be a period for recovery and healing before full vision can returnthis time frame may vary depending on individual factors and the severity of the damage before surgery.
Most patients who have undergone successful retinal detachment repair can expect their vision improvement to occur gradually over several weeks following their operation. However, some cases may take longer than others due to more extensive damage before surgery or age-related macular degeneration present at diagnosis that did not respond optimally during treatment with laser photocoagulation therapy .
Most people who undergo successful retinal detachment surgery experience improved sight shortly after they leave the hospital, but peak vision recovery usually occurs between one month – six months postoperatively. However, even up to twelve months, visual improvements can still be seen.
Recommended Reading: Best Milk For Diabetics Australia
Tell Your Doctor About Any Changes To Your Eye Sight
These wont be the same for everyone, but here are some of the early signs of retinopathy:
- seeing floaters these look like whispy clouds, floating in and out of your vision
- dimmer vision like youre wearing sunglasses all the time
- struggling to see when its dark.
If you notice any changes, or youre struggling to see as clearly as normal, make an appointment with your doctor straight away. Dont wait until your next screening.
Your eyesight can also go a bit blurry if your blood sugar goes higher than usual, even for a short time. This is normal and is a symptom of high blood sugars. Get your sugar levels back to your target level and when theyve settled, your vision should go back to normal.
How Does Diabetes Cause Vision Loss

Uncontrolled or poorly controlled diabetes can damage the blood vessels of the retina, the part of your eye that converts light into electrical signals that allow us to see. Damage to these delicate blood vessels can lead to swelling of the macula, the central part of your retina that allows us to see detail.
Diabetic retinal damage can also lead to bleeding in the eye, scarring, high eye pressure and even retinal detachment. Diabetic retinopathy or diabetic retinal damage is a leading cause of irreversible blindness worldwide.
You May Like: Does Goodrx Cover Diabetic Test Strips
How Diabetes Affects The Eyes
Having too much sugar in your blood can damage the blood vessels in the part of the eye called the retina. The retina is the tissue lining the back of the eye.
High sugar levels cause the blood vessels to swell and leak into the retina and cause blurred vision or blind spots. If left untreated, new blood vessels may grow and cause further damage to your vision.
Can Diabetic Retinopathy Be Reversed All You Need To Know
Both types of Diabetes mellitus are often associated with other serious health concerns.
These comorbid conditions can take the form of nerve damage, wounds that wont heal, and organ failure, just to name a few. Theyre also present more often than not a recent study found that of type II diabetic adults, 97.5% have one or more comorbid disease and 88.5% had two or more.
One comorbid condition that fewer people are familiar with is diabetic eye damage, known as retinopathy. Left untreated, this condition can progress into partial or total blindness.
Can diabetic retinopathy be reversed, and how does it affect your vision and eye health long-term? If youre wondering if theres hope for your diabetic vision loss, read on for the answers to those questions and more.
Read Also: What To Do If You Take Too Much Insulin
Can Diabetic Retinopathy Be Reversed
Modern eye surgery has come a long way in the past few decades. While there are advanced treatments available for retinopathy today, there still isnt a cure. The treatments focus on slowing or stopping the progression of the disease to preserve the vision you have left.
The ability of your eye surgeon to treat retinopathy symptoms relies on two things: early detection and early intervention. If you wait until your symptoms are severe to get your eyes examined, there may not be much they can do to help. If you get regular check-ups and visit any time theres a significant change in your vision, though, they may be able to stop your symptoms from getting worse.
Stages Of Diabetic Retinopathy
Diabetic retinopathy has 2 main stages:
Early stage : Blood vessel walls in the retina weaken and bulge, forming tiny pouches . These pouches can leak blood and other fluid, which can cause a part of the retina called the macula to swell and distort your vision. Macular edema is the most common cause of blindness in people with diabetic retinopathy. About half of people with diabetic retinopathy will develop macular edema.
Advanced stage : In this stage, the retina begins to grow new blood vessels. These new vessels are fragile and often bleed into the vitreous . With minor bleeding, you may see a few dark spots that float in your vision. If theres a lot of bleeding, your vision may be completely blocked.
You may not notice symptoms in the early stage. Thats why its very important to get a dilated eye exam at least once a year to catch any problems early when treatment is most effective.
Symptoms in the advanced stage can include:
- Dark or empty areas in your vision
Recommended Reading: Ways To Reduce Type 2 Diabetes
How Can Diabetes Affect Your Ocular Health
Your eyes are supported by various blood vessels in your retina. These blood vessels are sensitive to high blood sugar, putting them at risk of damage if you have diabetes.
Blood vessels may swell, break, and leak fluid if your blood glucose levels are high for long periods. Damaged blood vessels can lead to severe vision loss.
Who Is More Likely To Develop Diabetic Eye Disease
Anyone with diabetes can develop diabetic eye disease. Your risk is greater with
- high blood glucose that is not treated
- high blood pressure that is not treated
High blood cholesterol and smoking may also raise your risk for diabetic eye disease.
Some groups are affected more than others. African Americans, American Indians and Alaska Natives, Hispanics/Latinos, Pacific Islanders, and older adults are at greater risk of losing vision or going blind from diabetes.
If you have diabetes and become pregnant, you can develop eye problems very quickly during your pregnancy. If you already have some diabetic retinopathy, it can get worse during pregnancy. Changes that help your body support a growing baby may put stress on the blood vessels in your eyes. Your health care team will suggest regular eye exams during pregnancy to catch and treat problems early and protect your vision.
Diabetes that occurs only during pregnancy, called gestational diabetes, does not usually cause eye problems. Researchers aren’t sure why this is the case.
Your chances of developing diabetic eye disease increase the longer you have diabetes.
Recommended Reading: Do I Have Type 2 Diabetes
Get Your Eyes Screened
Eye screening is a way of spotting eye problems before you notice any changes to your sight.
Everyone whos over 12 years old and living with diabetes is entitled to an NHS diabetes eye screening at least once every two years. Its one of your diabetes health checks.
Diabetic retinopathy can become quite advanced before it starts affecting your sight, so that’s why it’s important to go to your regular eye screening appointments. That way, you can get the right treatment in time.
Weve also got more information about what happens during an eye screening, so you can feel prepared going to your appointment.
Read our latest update for more information on eye screening and other routine appointments.