Pump Problem : The Occlusion Error
I have trouble detecting whether my pump has an occlusion problem. An occlusion is any blockage of the thin plastic cannula that serves as the entry port into your body for insulin. Sometimes cannulas get bent on insertion, reducing or cutting off the flow of insulin. Other times the body fouls the cannula over time. Pumps are supposed to detect occlusions
Suspending & Resuming Your Pump
Device: MiniMed® 530G , MiniMed® Paradigm RevelTM , MiniMed Paradigm® 522/722, MiniMed Paradigm ®515/715, MiniMed Paradigm ®512/712
Manually Suspending your Pump
Manual Suspend stops all insulin delivery, including the current basal and any bolus or Fill Cannula deliveries in progress. While manually suspended, your pump will not deliver insulin until you manually resume your pump. When you resume your pump, the basal delivery will continue.
The pump will beep or vibrate about every 15 minutes on the hour to remind you that it is not delivering insulin. When manually suspended, your pump is in Attention mode with a solid circle showing on the pump. When in manual Suspend, you can only resume your basal or view the STATUS screen. Any bolus or Fill Cannula deliveries that were in progress when you suspended will not resume. If the Sensor feature is turned on, you can also view the sensor graphs and the SENSOR STATUS screen. No other functions are available
To manually suspend the pump:
Resuming Pump Delivery
Which Pump Is Best
All insulin pumps have benefits and drawbacks. Your choice will depend on whatâs most important to you. Do you want easy setup? Low up-front cost? Ease of use? Since most insurance companies will replace your pump only after several years of use, itâs important to find one that works for you.
Some things to think about:
- Which is best for your lifestyle: a traditional pump, tubeless pump, or pump with handheld remote?
- Pump reservoirs hold between 176 and 315 units of insulin. Kids may be fine with smaller reservoirs adults may want larger.
- Can the pump deliver insulin in small amounts? Kids and people who are very sensitive to insulin may want one that does.
- Does the pump come with carb counts of common foods to help you decide how much insulin you need?
- Can the pump interact with a blood glucose meter or continuous glucose meter ?
- Does the pump software work with your phone or laptop?
Also Check: What Salad Dressing Is Good For Diabetics
Excuse Me While I Turn Off Your Insulin Pump
Interested in learning what’s next for the gaming industry? Join gaming executives to discuss emerging parts of the industry this October at GamesBeat Summit Next. Learn more.
Diabetics beware. It is possible to hack your insulin pump, from a distance, so that it can harm you rather than save your life. Other medical devices are also vulnerable to hacking in the current age of cyber insecurity. As if patients dont have enough to worry about.
In a talk at the Black Hat security conference in Las Vegas, Jerome Radcliffe, a diabetic himself and a security researcher, showed how he figured out how to hack into insulin pumps for diabetics.
With diabetes, a patient cant properly process sugar in his or her blood because the body cant make enough insulin, which bonds with the sugar and turns it into fat. Patients have to inject themselves with synthetic insulin as many as several times a day to keep their blood sugar under control. If they have too little or too much sugar in their blood, the results can be incapacitating or even life threatening.
Insulin pumps use wireless sensors that detect blood sugar levels and then communicate the data to a screen on the insulin pump. The patient can monitor the readings and inject the insulin as needed. Radcliffe reverse-engineered the pumps and the wireless connectivity and figured out that the system was relatively unprotected. It was configured much more like a dumb device where the manufacturers assumed no one would try to hack it.
Whats So Great About The Pump

The list is an important one, in large part because pumps provide more precise and tailored insulin delivery. As a result, they offer greater lifestyle flexibility. Tailored insulin delivery can help:
- The dawn phenomenon by matching your early-morning increase in insulin resistance, so you avoid high blood sugar.
- Post-meal glucose rise from slowly digested foods or gastroparesis .
- Shift workers by adjusting the basal rates to your varying work schedule
- Frequent travelers by adjusting the basal and bolus rate to your travel schedule and time zone changes
- Prevent low blood sugars during physical activity and exercise by use of temporary basal insulin rate settings
- Extremely insulin sensitive people by delivering small doses of insulin
You May Like: Urine Test For Diabetes Type 2
Pump Problem : The Disconnect Dilemma
Im worried about the insulin I lose when I disconnect. In the shower. Getting a CAT scan. Swimming. Intimate moments. These are times when you want or need to take the darn thing off. The problem is that as a pumper, you have no long-acting insulin in your body, so if youre separated from your constant drip of fast-acting for too long, your blood sugar will spike, perhaps dangerously so.
- Fix-It: Set a smartphone stopwatch timer when you disconnect. When youre ready to hook up again, check the sans-insulin time and multiply it by your average basal rate during the time you were disconnected, then take that amount as a manual makeup bolus.
How To Get An Insulin Pump
To get a pump for free, youll have to meet certain criteria set by the National Institute for Health and Care Excellence .
If you live in England and Wales, youre over 12 years old and have type 1 diabetes, you need to meet one or more of the following criteria:
- You cant get to your target HbA1c without severe hypos.
- Your HbA1c remains high despite carefully trying to manage your diabetes.
If you live in Scotland or Northern Ireland, the criteria is different. Your healthcare team will give you advice on whether you meet your local criteria for getting a pump and what the next steps are.
If youre thinking about an insulin pump for your child, the criteria is different. Pumps are recommended for children under 12 when multiple daily insulin injections arent practical or appropriate. Make sure you speak to your diabetes specialist about if this is the best option for your child.
We understand that trying to get an insulin pump can be very frustrating, and you might feel disappointed if you cant get one. If you have any questions at all, or you just need someone to talk to, call our helpline.
Pumps are currently not available for people with Type 2 on prescription. You can self-fund, but make sure you have a discussion with your healthcare professional if youre thinking of trying one.
Don’t Miss: Can Diabetics Eat Ramen Noodles
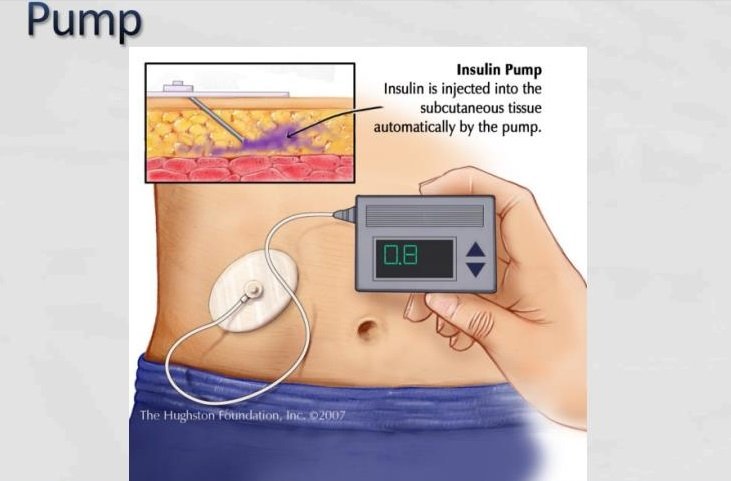
How Is An Insulin Pump Worn
Insulin pumps are connected to the body via the infusion set. The small needle or plastic cannula sits under your skin through the day whilst the infusion set is held in place by an adhesive that is similar to the sticky backing of a plaster.
The infusion set can usually be placed in the same sites on the body as are used for injections. The infusion set can usually be left in for two to three days. After this you must insert a new infusion set into a different place on your body. It is important to rotate sites, just as you should do with standard insulin injections.
The pump itself can be safely and discretely attached in lots of different ways, such as to a belt or the waist of trousers, held in pockets or in pouches attached to your thigh or upper arm.
What About Product Recalls
It can be a bit concerning when device recalls make the headlines, especially if the particular pump model thats supposed to keep you alive is the subject.
The Food and Drug Administration keeps a comprehensive database of safety notices, and according to an Associated Press analysis of that database from 2008 to 2018, insulin pumps and their components are collectively responsible for the highest overall number of malfunctions, injury and death reports.
Yikes, that certainly sounds scary.
But the FDA database can be difficult to navigate and even a bit misleading if searched without the proper context.
During an investigation of the database a few years ago, then-director of the FDAs division of chemistry and toxicology devices Dr. Courtney Lias told DiabetesMine: You cant just look at the number of recalls and make conclusions based on those numbers alone You have to take into context what the recall was, how it was found, and what else was going on with the company at the time. Thats hard to do from the outside because you dont have those conversations and context all the time.
In addition, this 2015 study from a team of researchers in Australia and New Zealand found that 40 percent of insulin pump users experienced problems, with a minority, particularly in children, requiring hospital management.
You May Like: What Is The Best Thing For Diabetes
Managing Insulin Pumps In General Practice
The management of a patient on an insulin pump requires the involvement of a specialist diabetes team including an endocrinologist, diabetes nurse educator and dietitian. The GP is an essential member of this team and it is therefore important GPs understand the terminology related to insulin pump therapy .3
The Daily Bolus Of Lr
by dailybolusoflr
Take Away: When discontinuing the insulin infusion in your DKA patient, schedule the subcutaneous long acting insulin to be given 1-2 hours prior to it stopping to ensure a proper transition. The current recommendations for insulin naïve patients is to start long acting insulin 0.1-0.2 units/kg and for patients on insulin prior to admission to resume home insulin regimen. If patients are NPO, more conservative long acting insulin dosing should be considered. Once the insulin infusion is stopped, discontinue the dextrose containing fluids as well.
Diabetic ketoacidosis is a serious emergency in diabetic patients and is associated with a mortality rate of up to 5%.1,2
The mainstay of therapy for DKA is insulin that is administered as a continuous intravenous infusion.1 The purpose of insulin is to resolve the ketone production associated with DKA.1
Continuous insulin therapy should be maintained until resolution of DKA .
Patients will require a transition from the continuous infusion to a subcutaneous long acting insulin with short acting insulin regimen.1 The purpose of the long acting insulin with short acting insulin bolus is to mimic the physiologic insulin secretion. The lack of initiating appropriate long acting insulin could cause the patient to revert back into DKA. The combination of long acting insulin with short acting insulin has been shown to have a lower incidence of hypoglycemic events compared to a regimen of mixed NPH and regular insulins.3
Read Also: What’s The Treatment For Type 2 Diabetes
Medtronic Minimed 630g Insulin Pump System
The MiniMed® 630G Insulin Pump System is a complete solution designed for advanced diabetes control. Waterproof design with a user-friendly color screen and simple menu Built-in CGM allows for wireless transmittal of glucose information Remote insulin dosing with the Bolus Wizard®, which helps to calculate mealtime insulin and may avoid insulin stacking Continuously delivers insulin, with a tubing change needed only every two or three days Multiple insulin delivery settings to meet unique needs Enlite Sensor® sends readings to insulin pump every 5 minutes, helping to identify trends and make adjustments CGM tracks glucose levels throughout the day, including the effects of food or exercise Predictive alerts given up to 30 minutes ahead, if trending high or low CCS Medical offers Ascensia Diabetes Care strips for use with Medtronic pumps for many insurance plans.Continue reading > >
Future Of Insulin Pumps
- Many insulin pumps on the market today are associated with a glucometer or continuous glucose monitor . These are termed closed loop insulin pumps systems that use continuous real time glucose levels to adjust dosage rather than adhering to a preset basal rate and calculated boluses.2 Closed loop systems are meant to better mimic physiologic pancreas activity and have the potential to improve patient adherence and glycemic control. However, closed loop systems still have limitations, including delays in response times, accurate signal feedback, software malfunctions, high cost, and user errors.9
- Other technological advances are being integrated into insulin pump therapy, including smartphone applications, Bluetooth compatibility, and data sharing.9 Research involving biological models of insulin therapy, including nanopolymer-mediated insulin delivery and pancreatic islet regeneration, are currently being investigated and may provide improved therapy options for diabetic patients in the future.17,18
Don’t Miss: How Are Insulin Pumps Attached
How Much Time And Effort Commitment Does Pump Therapy Require
Starting pump therapy requires commitment. It is not unusual to check blood sugars 8-12 times per day in the beginning of pump therapy to assess basal and bolus insulin needs. This often means lots of interruptions during the workday and during family time. It also means disturbing your sleep in order to take blood sugar readings in the middle of the night. Think about your schedule and commitments. Talk to your family for support. Plan ahead.
Cgm Problem : Sensor Falls Off
My sensor always falls off before it expires! Especially in hot weather, many PWDs find that the sensor doesnt want to stay on for the entire session.
- Fix-It: Think about when you attach a sensor. Kamil Armacki of NERDabetic YouTube fame says, One thing I have found helpful is applying the sensor when my skin is dry and cold, so not within 4 hours of taking a bath or shower. If that doesnt work, many PWDs cover the sensor with an over bandage, either from the very start or once the edges of the adhesive pad on the sensor start peeling loose. Dont use duct tape or Band-Aids! Dexcom offers free over patches for its users. For something more artistic, Pump Peelz offers a wide range of creative over bandages. Or for the active crowd, Skin Grip offers a 4-way stretch hypoallergenic fabric patch in a wide range of both skin and primary colors. What also helps is using an adhesive wipe on the skin before insertion. See Problem No. 3 below.
Also Check: Any Breakthrough In Diabetes Treatment
Contacting Your Insulin Pump Maker
Once upon a time, PWDs using insulin pumps were sometimes given two devices, so theyd always have a backup if one broke. Today, with more advanced technology and tighter budgets, that is no longer the case.
But some of the insulin pump makers still offer a travel loaner option, which allows you to borrow an extra pump for a modest fee for a limited time.
All of the companies now have fairly cut-and-dry recommendations for what you should do if your insulin pump suddenly becomes a very expensive paperweight.
This usually involves contacting a call center, where a representative will take down your product and customer information for their database, and walk you through a step-by-step troubleshooting process to see if they can fix the problem first, without needing to send a new device.
If its determined that you do need a replacement, the units are generally sent by overnight shipment or second-day delivery, meaning youll be up and running again very soon. If you worked with a local rep to get set up on your pump initially and still have that persons contact information, feel free to reach out. Those regional reps can sometimes help out even more immediately by dropping off a new unit to you in case of emergency.
Here are the specifics of what the existing pump companies in the United States tell their customers to do in case of trouble:
What Is Insulin Pump Therapy
An insulin pump is a small device that mimics some of the ways a healthy pancreas works. It is safe, discreet and reliable. It can be attached to the same sites you currently inject in and insulin is simply delivered to your body through a thin tube. An insulin pump replaces the need for frequent injections by delivering rapid acting insulin continuously 24 hours a day. See below its components:
Also Check: How To Get Diabetic Shoes Through Medicare
Insulin Pumps Personal Cgm And Security
- When flying with an insulin pump or CGM system, you can continue to wear your device while going through common security systems such as an airport metal detector as it will not harm the device or trigger an alarm. Do not send the devices through the x-ray machine.
- You need to remove your insulin pump and CGM while going through an airport body scanner. If you do not wish to remove your devices, you may request an alternative pat-down screening process.
- Notify security screeners that you have diabetes, that you are wearing an insulin pump and are carrying supplies with you.
Pump Tip: Understanding The Auto Off Alarm
Since insulin pumps work on your behalf throughout the day every single day, its so important that there are built-in safety features. One feature you might not be familiar with is the Auto Off alarm. Auto Off is a safety feature designed to automatically stop insulin delivery if for some reason you dont press a single button within a given amount of time. Since you likely press buttons throughout the day, this is a feature that you wont see often. You can set this time period to be anywhere from 1 to 24 hours and its best to base this on how often you typical interact with your pump. The factory default on your pump has this feature set to off. To program your Auto Off alarm, head to the Utilities menu. For instructions and more information, check out your user guide.
IMPORTANT SAFETY INFORMATION
Medtronic Diabetes insulin infusion pumps, continuous glucose monitoring systems and associated components are limited to sale by or on the order of a physician and should only be used under the direction of a healthcare professional familiar with the risks associated with the use of these systems.
Successful operation of the insulin infusion pumps and/or continuous glucose monitoring systems requires adequate vision and hearing to recognize alerts and alarms.
Please visit for complete safety information.
You May Like: Stop Type 2 Diabetes Naturally