How Is G6pd Deficiency Treated
In most cases, G6PD deficiency does not cause problems. Problems may occur if you are exposed to medicines or foods that may harm your blood cells. Depending on your gene flaw, you may be able to handle a small amount of these exposures.
Your healthcare provider will figure out the best treatment based on:
- Your age, overall health, and medical history
- How sick you are
Pearls And Other Issues
A special situation exists in the management of G6PD patients with methemoglobinemia. Methemoglobin forms in red blood cells when the iron in the heme group of hemoglobin molecules undergoes oxidation from the normal ferrous state to the ferric state. This ferric state is a poor binder of oxygen. Symptoms of hypoxia begin to develop when the level of methemoglobin reaches 10%, and death can occur when the level reaches greater than 50%.
Methemoglobinemia should be considered in patients presenting with central cyanosis and hypoxia whose symptoms are resistant to supplemental oxygen. A specific antidote for severe acute methemoglobinemia is methylene blue. Intravenously injected methylene blue is reduced to leucomethylene blue through NADPH-dependent mechanisms. Leucomethylene blue is then used as a substrate to reduce methemoglobin back to hemoglobin. However, patients who are deficient in G6PD lack sufficient NADPH to properly reduce methylene blue. Unreduced methylene blue can cause further oxidative damage in the G6PD-deficient patient resulting in hemolysis and even death. Therefore, it is important that patients who are known or suspected to have any degree of G6PD deficiency not receive methylene blue. Alternative therapies for G6PD deficient patients presenting with methemoglobinemia include transfusing packed red blood cells or providing hyperbaric oxygen therapy.
When Should I See My Healthcare Provider
You should see your healthcare provider any time you develop G6PD deficiency symptoms. Seek immediate medical help if your symptoms are severe and come on quickly.
A note from Cleveland Clinic
If youve been diagnosed with G6PD deficiency, you may feel better knowing most people with G6PD deficiency never have symptoms. But if youre among those who do, or you have a newborn baby who does, youre probably worried about what to expect.
G6PD deficiency cant be cured, but its symptoms can be managed. You can take care of yourself by knowing what food and medications to avoid and by developing healthy habits such as drinking alcohol in moderation, getting enough rest and exercise and avoiding tobacco smoke. You can take care of your newborn baby by monitoring jaundice symptoms that are a sign of G6PD deficiency. Ask your healthcare provider for information to help you manage the impact G6PD deficiency may have on your daily life.
Recommended Reading: A1c To Average Blood Sugar
Who Is Affected By G6pd Deficiency
G6PD deficiency affects between 400 and 500 million people across the world. G6PD deficiency is more common among people living in sub-Saharan Africa, the Mediterranean and Southeast Asia regions.
Healthcare providers estimate that 1 in 10 Black men in the United States has G6PD deficiency. Overall, an estimated 4% to 7% of people in the United States have this genetic disorder. About 30% of newborn infants who have severe jaundice have G6PD. Females are less likely than males to have G6PD deficiency.
What Tests May My Provider Use To Diagnose G6pd Deficiency
Your healthcare provider will focus on your blood cells. They may do some tests to rule out other conditions. Having a test for lactate dehydrogenase for signs of the blood cancer lymphoma doesnt mean you have lymphoma. Some other tests they may use include:
- Complete blood count : CBCs help healthcare providers identify and diagnose diseases.
- Bilirubin levels: This is a blood test.
- Reticulocyte count: This blood test measures your young blood cells to see if your bone marrow is producing enough red blood cells.
- Serum aminotransferases: This test checks on an enzyme in your liver.
- Peripheral blood smear: This blood test involves checking for changes in the number, type, shape and size of blood cells.
Read Also: Is Blood Sugar The Same As Glucose
What Remains To Be Done
Much has been learned about G6PD deficiency and its effects in the past 50 years, but as in every field of science there is still much to learn. Here I can only mention a few of the problems that I consider to be important now.
The development of simple means of testing new drugs in vitro to determine whether they will cause hemolysis in patients has eluded us. Simply incubating drugs with red cells is unreliable, at least in part because it is usually drug metabolites, not the original drug, that are hemolytic. Several different model systems have been proposed, but none have been extensively validated. Perhaps the most attractive of these is the use of plasma from a normal subject ingesting the drug and determining whether it increases metabolism by way of the hexose monophosphate shunt.
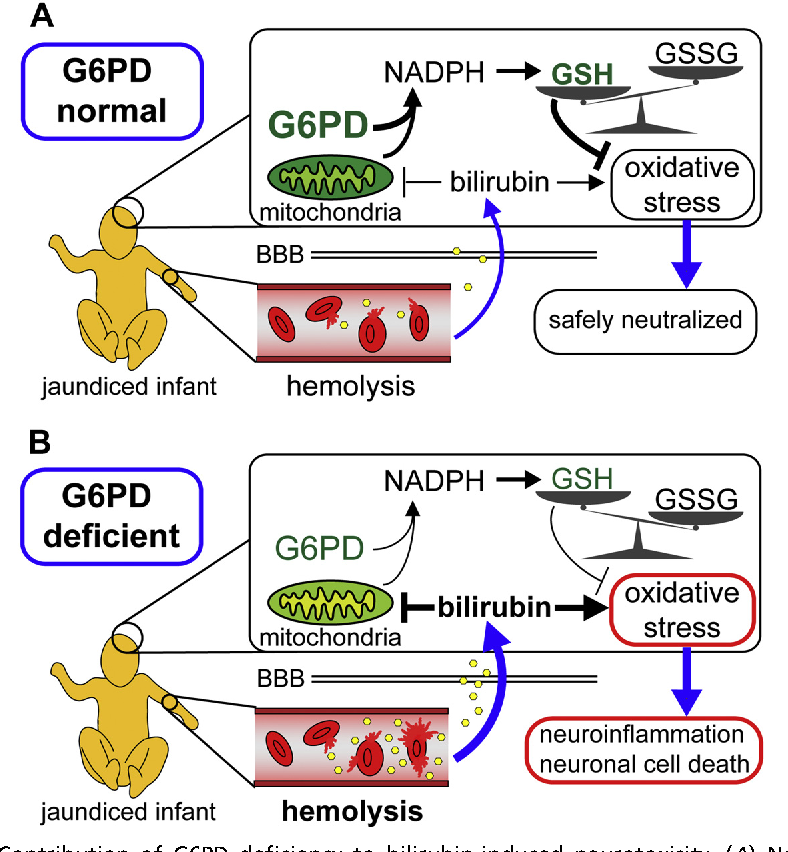
Another area of importance is the most devastating result of G6PD deficiency: kernicterus. There has been a resurgence of severe neonatal jaundice and kernicterus in recent years, and G6PD deficiency is one of the causes. Should all newborns be screened? Is the human and the financial cost worth it? Should the screening be limited to ethnic groups who are known to have high gene frequencies, and if so, how will they be identified? Or would it be better simply to monitor bilirubin levels of newborns more closely, thus saving infants from the tragedy of kernicterus, regardless of cause?
Epidemiological Characteristics Of G6pd Deficiency
The geographical distribution of G6PD deficiency is extensive, with the frequency peak of infections found in Africa, the Middle East the Mediterranean region, and Asia however, due to recent migration, this disease occurs in the United States and Northern Europe. The prevalence of the disease is highest in Africa, Asia, the Middle East, Latin America and the Mediterranean. Among them: Kurdish Jews 6070%, Sardinia 435%, Nigeria22%, Thailand17%, Greece6%, South China6%, India3%. The lack of G6PD affects black Americans, of which up to 24% are carriers, and about 10% are affected by black males . It is found that the distribution of G6PD deficiency is similar to that of malaria endemic areas. This indirect evidence suggests that G6PD deficiency is resistant to malaria , but it does not prove that malaria selects for the gene that causes G6PD deficiency. Natural selection seems responsible for the higher mortality rates of children from malaria in endemic areas. By comparing the incidence of malaria, parasiteia levels, or the severity of malaria in children with G6PD normal and deficiency, studies conducted in Africa and other regions showed that the lack of G6PD appeared to have a protective effect on severe malaria , but the results need more data to support.
You May Like: How To Reverse Ed In Diabetics
How Do Healthcare Providers Treat G6pd Deficiency
Healthcare providers use different treatments based on your situation. For example, if you have mild jaundice and your doctor knows you have G6PD deficiency, theyll treat your jaundice symptoms and tell you what food or other triggers you need to avoid going forward.
Some people and newborn babies have more severe symptoms. If you have hemolytic anemia, you may need a blood transfusion. If your newborn baby has jaundice, their healthcare provider may treat it with phototherapy . In more serious cases, your babys healthcare provider may recommend whats called an exchange transfusion. In exchange transfusions, their healthcare provider removes your babys unhealthy blood while replacing it with healthy, donated blood.
Why Are Males More Likely To Have G6pd Deficiency
G6PD deficiency is inherited as an X-linked recessive condition. Heres what that means:
- Males are more likely to have G6PD deficiency because they only have one X chromosome, which increases the odds a male will pass on the mutated G6PD gene.
- Females, however, have two X chromosomes, which increases the odds a female will pass on a normal G6PD gene instead of a mutated G6PD gene.
- Most females can carry the mutated gene and dont have G6PD deficiency. Some females may be affected if one or both copies of the G6PD gene are mutated. Females with one mutated gene may have lower G6PD activity and less risk of developing symptoms.
Also Check: What Are The 4 Types Of Diabetes
How Can We Overcome Glucose
Protecting the kids from the harmful effects of glucose-6-phosphate-dehydrogenase deficiency is totally in the hands of the parents. Proper supervision is required as the kids are always exposed to several trigger factors. Since a few medications can elevate the risk of glucose-6-phosphate-dehydrogenase deficiency, parents should always get an opinion or prescription from a professional doctor. Getting a second opinion is a high-level safety behavior. You can contact iCliniq.com for this purpose.
How To Prepare For G6pd Deficiency Test
Some medicines may affect the outcomes of these tests. Any medications you are taking, including prescriptions and dietary supplements, should be disclosed to your doctor. Before your G6PD test, they may advise you to stop using them. Testing shouldnt be carried out right away following a blood transfusion. The outcomes might be tainted by this.
Tell your doctor if you recently had fava beans or used sulfa medications. Sulfa medications include:
- Antibiotics or antifungal medications
- Anticonvulsants
Sulfa medications can have negative effects, especially in those who have G6PD deficits.
If you have a hemolytic episode, your G6PD test can be postponed. Throughout an episode, a lot of cells with low levels of G6PD are killed. Your test results can display erroneously normal G6PD levels.
Youll receive detailed instructions from your doctor on how to get ready for your blood draw. Before a G6PD test, it wont be necessary to fast or refrain from eating or drinking.
Don’t Miss: Normal Glucose Range For Diabetics
Genetics Of Leukocyte G6pd Deficiency
G6PD deficiency is the most common enzyme deficiency in humans, with over 140 different mutations described . The most common mutations lead a mild-to-moderate enzyme deficiency and to intermittent hemolysis usually secondary to infections or drugs. Few patients with severe forms of G6PD deficiency present with a CGD-like clinical picture. Profound deficiency of G6PD leads to a defect in NADPH production, causing impaired respiratory burst activity . The gene coding for this G6PD enzyme is located on Xq28 . The G6PD enzyme is a heterodimer, each monomer being associated with an NADP+ molecule. This enzyme has a widely variant polymorphism in different populations in the world. Studies in blacks and whites have shown that whites with G6PD deficiency more often have affected leukocytes . G6PD deficiency in leukocytes is encoded by the same gene as that in erythrocyte precursors and other tissues. G6PD activities in leukocytes are usually higher than those in erythrocytes, so that patients with G6PD-deficiency-associated hemolytic anemia usually have normal leukocyte function. Only leukocytes with < 20% of normal G6PD activity show abnormal bactericidal activity. Whether there are unknown factors in leukocytes from different races that could affect G6PD activity remains to be determined as patients with G6PD deficiency associated with the CGD-like syndrome have been reported in white, but not in black or Mongolian populations.
What Are The Signs & Symptoms Of G6pd Deficiency
Most people with G6PD deficiency don’t have any symptoms. Others might have symptoms of hemolytic anemia if many RBCs are destroyed.
These can include:
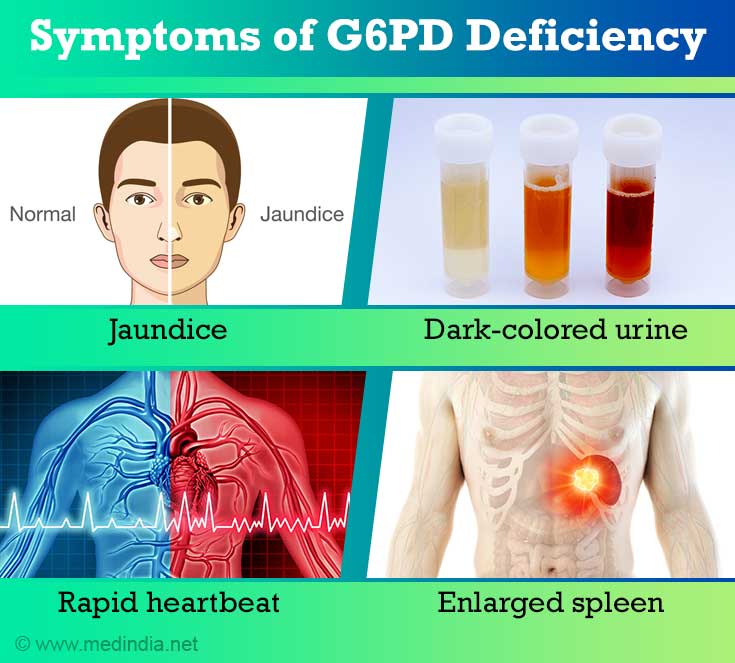
- extreme tiredness or dizziness
- fast breathing or shortness of breath
- dark, tea-colored pee
Mild symptoms usually don’t need medical treatment. As the body makes new red blood cells, the anemia will improve. If symptoms are more severe, a child may need care in a hospital.
Also Check: Normal Blood Sugar 2 Hours After Eating
What Is G6pd Deficiency
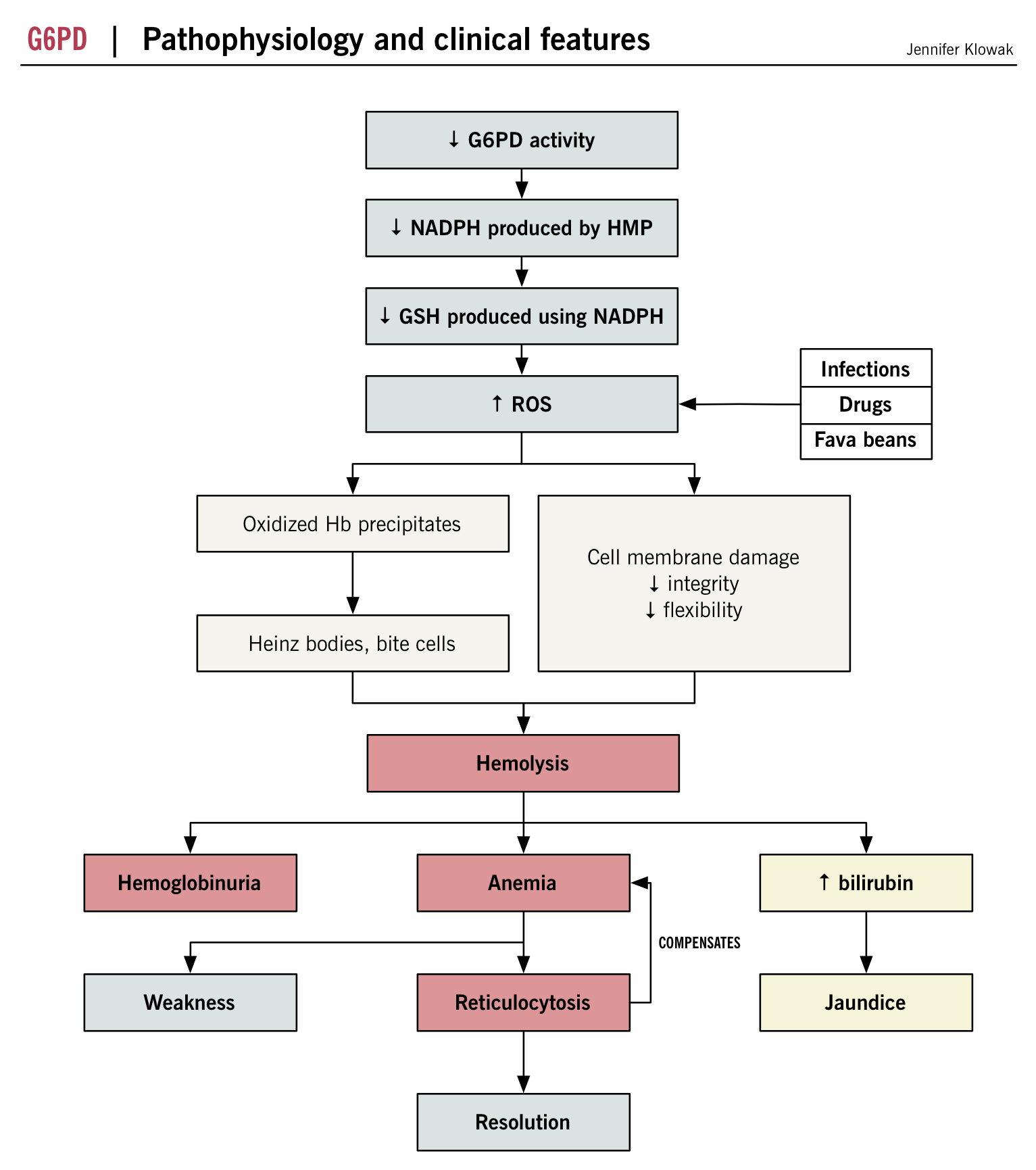
This is a genetic disorder that affects peoples G6PD levels. G6PD stands for glucose-6-phosphate dehydrogenase. G6PD is an enzyme that protects your red blood cells from harmful substances. Deficiency happens when the gene that drives the G6PD enzyme mutates or changes so the enzyme cant protect red blood cells. Certain foods and medications can trigger G6PD deficiency, too.
Most people with G6PD deficiency dont develop symptoms. In some instances, though, G6PD deficiency can cause serious medical conditions such as hemolytic anemia in adults and severe jaundice in newborns. Sometimes, anemia symptoms develop very quickly, causing hemolytic crisis symptoms that require immediate medical attention.
Signs And Symptoms Of G6pd Deficiency
Most patients with G6PD deficiency are asymptomatic. Clinical manifestations may include the following:
- Neonatal jaundice
- Episodes of intravascular hemolysis and consequent anemia, triggered by infections, medicines that induce oxidative stresses, fava beans, and ketoacidosis. Hemolysis begins 24 to 72 hours after exposure to oxidant stress. Patients with severe hemolysis present with weakness, tachycardia, jaundice, and hematuria.
- Chronic hemolytic anemia
References
Guide to G6PD deficiency rapid diagnostic testing to support P. vivax radical cure. World Health Organization. Available at . 2018 Accessed: July 19, 2021.
Nkhoma ET, Poole C, Vannappagari V, Hall SA, Beutler E. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. 2009 May-Jun. 42:267-78. .
Beutler E. Glucose-6-phosphate dehydrogenase deficiency: a historical perspective. Blood. 2008 Jan 1. 111:16-24. .
Peters AL, Van Noorden CJ. Glucose-6-phosphate dehydrogenase deficiency and malaria: cytochemical detection of heterozygous G6PD deficiency in women. J Histochem Cytochem. 2009 Nov. 57:1003-11. . .
Beutler E, Westwood B, Prchal JT, Vaca G, Bartsocas CS, Baronciani L. New glucose-6-phosphate dehydrogenase mutations from various ethnic groups. Blood. 1992 Jul 1. 80:255-6. .
Beutler E. G6PD deficiency. Blood. 1994 Dec 1. 84:3613-36. .
Don’t Miss: Marijuana And Type 1 Diabetes
What Happened After The G6pd Test
The outcomes of your G6PD test will be discussed with your doctor at a subsequent session.
A genetic deficit is indicated by low blood levels of G6PD. This condition is incurable. However, by avoiding certain triggers, you may stop hemolytic episodes and the signs and symptoms of anemia.
A G6PD deficiency hemolytic event has the following triggers:
- Naphthalene, a substance included in moth repellant and toilet bowl deodorizers, is ingested via the consumption of fava beans.
- Taking aspirin and other nonsteroidal anti-inflammatory medicines , such as ibuprofen, are other possible factors .
Your doctor will be aware of other drugs to avoid due to potential problems. Some of these chemicals are:
- Methylene blue nitrofurantoin, often known as Macrobid or Macrodontia, is a medication used to treat Uti .
- Quercetin, a key component of several nutritional supplements, phenacetin, a painkiller, primaquine, an antimalarial medicine
Can G6pd Deficiency Be Cured
Healthcare providers cant cure G6PD deficiency because its a genetic disorder. But there are things you can do to avoid triggering the chain of events that cause G6PD deficiency symptoms. Ask your healthcare provider about the food and medications you should avoid. Here are some other suggestions:
- If you drink alcohol, try to avoid drinking too much. Drinking excessive amounts of alcohol increases oxidative stress. Too much oxidative stress leads to hemolytic anemia.
- If you smoke tobacco products, try to quit. Smoking tobacco weakens your immune system and encourages free radicals.
- Exercise is a good habit, but dont overdo it. Pushing yourself through a workout may increase oxidative stress.
- Try to get enough rest. Sleep supports your immune system, which helps you fight off infections that can trigger G6PD deficiency.
- Stress can trigger G6PD deficiency symptoms. If youre feeling anxious or stressed, ask your healthcare provider for help managing.
Read Also: A1c 5.2 Average Blood Sugar
Who Is At Risk For G6pd Deficiency
G6PD deficiency occurs most often in men. It is rare in women.
The disorder affects about 10% of African-American men in the U.S. It is also common in people from the Mediterranean area, Africa, or Asia.
The severity of the disorder varies, depending on the group. In African-Americans, the problem is mild. It mainly affects older red blood cells. In whites, the disorder is often more serious. In this group, young red blood cells are affected.
What Causes G6pd Deficiency
G6PD deficiency is a genetic condition that is passed along from one or both parents to their child. The defective gene that causes this deficiency is on the X chromosome, which is one of the two sex chromosomes. Men have only one X chromosome, while women have two X chromosomes. In males, one altered copy of the gene is enough to cause G6PD deficiency.
Females are usually affected if there is a mutation present in both copies of the gene, though in some cases, females with one G6PD mutation can also experience symptoms. Since females have two X chromosomes, males are affected by G6PD deficiency much more frequently than females.
You may have a higher risk of having G6PD deficiency if you:
- are of Middle Eastern descent
- have a family history of the condition
Having one or more of these risk factors doesnt necessarily mean that you will have G6PD deficiency. Talk with your doctor if youre concerned about your risk for the condition.
Read Also: What Is A Good Score For Diabetes
What Are G6pd Deficiency Symptoms
Some people who have G6PD deficiency may have hemolytic episodes that cause the following symptoms or conditions:
- Anemia. People can have a severe form of anemia called acute hemolytic anemia.
- Jaundice. When your skin turns yellow.
- Dark-colored pee.
What are hemolytic crisis symptoms?
These symptoms are similar to anemia, but develop very rapidly. Symptoms include:
- You have a sudden rise in body temperature.
- You notice your skin is turning yellow or youre more pale than usual.
- Your pee is dark yellow-orange.
- You have heavy, fast breathing.
- Your pulse is weak and rapid.
- You feel exhausted and generally unwell.
What symptoms are common for newborns who have G6PD deficiency?
Infants rarely develop serious and obvious G6PD deficiency symptoms. The most common symptom is severe jaundice that appears within an infants first 24 hours and/or an infant has a bilirubin level thats greater than the 95th percentile. Left untreated, infants with severe jaundice can develop brain damage.
Overexpression Of Wt G6pd And Canton Variant In Sh
Prior to the cellular-based assays using SH-SH5Y cells, the duration of overexpression of WT G6PD and Canton variant was examined by transfecting the cells seeded in a 12-well plate. The genes encoding human WT G6PD and Canton variant were first PCR-amplified, which was then inserted into pcDNA 3.1/myc-His C using HindIII and XhoI restriction enzyme sites. 0.5g of cDNA and 1.5g of lipofectamine were diluted in 50L of Opti-MEM medium, respectively and incubated for 5min. The diluted DNA was combined with diluted lipofectamine, which was followed by incubation for 20min prior to the addition to cells. The transfected cells were collected at different time points , and the overexpressed G6PD levels were examined by Western blot. The transfection was carried out in 50% serum-starved cells. Once the duration of expression was confirmed, other cellular-based assays were performed.
Recommended Reading: Average Age Of Type 2 Diabetes