Testing Stratification Loci In T1dgc Set 3 Families
Families from the final T1DGC cohort were stratified as above, but the analyses were only performed for the loci with LOD > 3 or with significant differences between stratified sets, as discussed above. Results of these confirmation tests are summarized in . Three stratified loci could be confirmed unequivocally: the locus on chromosome 19q for HLA IBD siblings and the loci on chromosome 6q13/14 for male and INS Tx siblings the same gene may be responsible for these chromosome 6q loci. Another two loci had significant scores on the same chromosome but outside the region within one LOD unit of the peak : 8q13 for INS AA genotype siblings and 7q36 for older age-of-onset siblings. In complex diseases, the location of causative genes may be displaced compared with both the peak and LOD-1 interval therefore, these regions warrant further investigation.
The correlation with GWAS-identified loci also is presented in . The following are five of the stratified loci that had suggestive LOD scores in regions that gave significant results in the T1DGC GWAS : PRKD2, CTRB2, CENPW , INS, and C19orf19. Association of these SNPs listed in could be followed-up in future studies of subsets of type 1 diabetes cases.
What Do I Need To Know About Genetic Testing And Counseling
Genetic testing for monogenic diabetes involves providing a blood or saliva sample from which DNA is isolated. The DNA is analyzed for changes in the genes that cause monogenic diabetes. Genetic testing is done by specialized labs.
Abnormal results can determine the gene responsible for diabetes in a particular individual or show whether someone is likely to develop a monogenic form of diabetes in the future. Genetic testing can be helpful in selecting the most appropriate treatment for individuals with monogenic diabetes. Testing is also important in planning for pregnancy and to understand the risk of having a child with monogenic diabetes if you, your partner, or your family members have monogenic diabetes.
Most forms of NDM and MODY are caused by autosomal dominant mutations, meaning that the condition can be passed on to children when only one parent carries or has the disease gene. With dominant mutations, a parent who carries the gene has a 50 percent chance of having an affected child with monogenic diabetes.
In contrast, with autosomal recessive disease, a mutation must be inherited from both parents. In this instance, a child has a 25 percent chance of having monogenic diabetes.
For recessive forms of monogenic diabetes, testing can indicate whether parents or siblings without disease are carriers for recessive genetic conditions that could be inherited by their children.
New Genetic Risk Test For Type 1
Dr Oram and colleagues have developed a test which looks for 30 genetic changes in a persons DNA. Each of the 30 genetic changes carries a small risk of Type 1 diabetes, and the test combines all these risks into a single score, which represents a summary of a persons genetic risk for Type 1 diabetes. If a person score is high, they are more likely to have Type 1 diabetes. If the score is low, they are more likely to have Type 2 diabetes.
You can watch a video about this exciting research on theReuters website.
Dr Oram says There is often no going back once insulin treatment starts. This may save people with Type 2 diabetes from being treated with insulin unnecessarily, but also stop the rare but serious occurrence of people with Type 1 being initially treated with tablets inappropriately and running of the risk of severe illness.
Read Also: Does Diabetes Affect Your Stomach
Identification Of Eggs From Enterobius Vermicularis
Parents of children participating in MIDIA have been asked to collect tape samples touching the anal region on three following mornings. They have then sent the samples in specially designed containers for tape sampling to the central laboratory in Oslo. Here all the tape samples have been examined by two scientists at different times. A child has been regarded as positive if down to one egg have been identified on one of the tapes.
Testing Gwas Snps In The Stratified Datasets
To test whether any of the linkage peaks observed in the stratified sets could be explained by SNPs associated with type 1 diabetes susceptibility in the T1DGC GWAS study , families were stratified according to criteria above and tested by the transmission disequilibrium test . Twenty SNPs were significantly associated in the overall dataset . However, for the linked regions listed in and , only regions 6p21, 11p15, 19q13, and 2q33 contained SNPs showing associations with type 1 diabetes by analysis of allele transmissions . There were significant differences in transmission for the HLA SNPs between the HLA identical and mismatched ASP sets, confirming a similar earlier analysis of 3,000 HLA SNPs in the T1DGC families . There also was an apparent bias in transmission of the HLA-DQA1 SNP in affected brothers. However, there were no significant differences in the non-HLA SNPs between any of the sets stratified by the other criteria .
Don’t Miss: Proliferative Diabetic Retinopathy Icd 10
New Developments In The Field
To date, the field of diabetes genetics has focused on detecting monogenic disorders, but now attention is turning to utilisation of information about the polygenic risk of diabetes. Single nucleotide polymorphisms can modify the risk of type 1 and type 2 diabetes, both polygenic conditions. Summing up the risk of individual SNP genotypes can provide a composite polygenic risk score. In diabetes, these risk scores have been used to support diabetes classification, given the challenge of differentiating type 2 diabetes from adult-onset type 1 diabetes and also MODY.21,22 The impact of using this clinical information and its applicability in all ethnicities have yet to be determined, and those in the field await further studies.23
Shivani Misra, Consultant in Diabetes and Metabolic Medicine, Imperial College Healthcare NHS Trust, London
Red Flags To Consider Genetic Testing Or Genetic Consultation45
Most of the time, a diagnosis or family history of type 2 diabetes is not a strong indication for a referral for genetic counselling. Patients may prefer a conversation with their healthcare provider about their empiric risks of developing this disease as genetic testing for type 2 diabetes susceptibility gene variants is not currently available in Canadian Genetic Clinics and is not recommended for risk assessment at this time because the presence of these variants is neither necessary nor sufficient for development of type 2 diabetes.
Although uncommon, attention should be paid to individuals where there is:
Young age at onset of diabetes, with features atypical for type 1 or 2
The presence of other medical conditions that, in conjunction with the diabetes, suggest a genetic syndrome
These rare forms of diabetes can be caused by a single gene mutation and, in these cases, genetic counselling and/or genetic testing may be appropriate and may influence treatment and prognosis.
Read Also: Type 2 Adult Onset Diabetes
Major Histocompatibility Complex Molecules
The major histocompatibility complex is a group of genes found in humans and animals that aids the immune system in recognizing foreign organisms.
In 2004, found that the presence of major histocompatibility complex molecules on certain chromosomes is a precursor to the development of type 1 diabetes.
Research Design And Methods
This study was approved by review boards of all contributing institutions, and appropriate informed consent was obtained from families. Inclusion criteria have been reported . Briefly, a family must contain at least one affected sib-pair affected indicates a type 1 diabetes diagnosis before the age of 35 years with insulin required within 6 months of diagnosis. Samples from 1,505 newly recruited families, as well as previously untyped members from 84 families recruited earlier , were available for genotyping. Families came from four T1DGC networks: Asia-Pacific , Europe , North America , and the U.K. . Of samples sent for genotyping, 1,396 families had two affected full siblings, 63 families had three, and 3 families had four or more. Four pedigrees also provided affected half-siblings. The remaining 117 families included samples from other family members that were unavailable for genotyping for the previously reported cohorts thus, they were available for the analyses of the total T1DGC dataset. Both parents were available for 914 families, whereas 397 families consisted of a single parent.
Don’t Miss: Nursing Care Plan For Diabetes
Genetic Prediction Models For Type 2 Diabetes Can Be Valuable In The Future
Previously published genetic studies have severe limitations that underestimate the true significance of genetic variants in predicting type 2 diabetes . Genetic prediction models can be improved by increasing the precision of the diagnosis of type 2 diabetes, by identification of low-frequency and rare genetic variants, by identification of risk variants for type 2 diabetes in nonEuropean ancestry populations, by increasing knowledge on structural variation and epigenetics, and by developing statistical techniques to evaluate gene-gene and gene-environment interactions.
Necessity of improving the precision of the diagnosis of individuals with diabetes.
Type 2 diabetes is a chronic hyperglycemic condition that is not type 1 diabetes or other subtypes of diabetes, which include genetic defects of insulin secretion and action, diseases of exocrine pancreas, endocrinopathies, drug- or chemically induced diabetes, diabetes in connection with infections, uncommon forms of immunomediated diabetes, other genetic syndromes sometimes associated with diabetes, or gestational diabetes mellitus . In other words, there is no precise definition of type 2 diabetes. In fact, this main subtype of diabetes is defined by excluding all other conditions leading to chronic hyperglycemia.
New sequencing techniques will identify low-frequency and rare variants with large effect sizes.
Genetic Heterogeneity And Epistasis
Another reason for the scant returns from this study could be disease heterogeneity, which could be increased by the requirement of worldwide recruitment of families to achieve sufficient statistical power. If there were multiple type 1 diabetes subtypes involving different genetic pathways, then the numbers of sib-pairs sharing haplotypes at relevant genes would be swamped by the remaining siblings with Mendelian-sharing ratios. Support for a notion of different genetically determined type 1 diabetes subtypes comes from the variation seen in disease, with some families having an earlier onset, and from studies that suggest that the increase in type 1 diabetes in recent decades is associated with lower risk HLA alleles . To address this issue, we compared sib-pairs selected for relevant criteria that have been shown previously to increase linkage evidence for particular loci . Although seven loci were implicated using this approach, the LOD scores for these could not support a hypothesis that they played a major role even in the type 1 diabetes subtype studied.
Also Check: Cold Medicine For Diabetics With High Blood Pressure
Genetics And The Stages Of Type 1 Diabetes
The onset of T1D symptoms is the clinical manifestation of the disease process that results from the interaction of predisposing genetic factors with environmental exposures, which eventually leads to a T-cell mediated, B-cell facilitated, autoimmune attack on beta-cells. The presence of islet cell autoantibodies is presently the earliest and more robust biomarker of islet autoimmunity. Autoantibody responses to at least two islet antigens define the first stage of T1D at this point remissions are rare. Stage 2 T1D is defined as the presence of two or more islet autoantibodies and dysglycemia, that is, glucose metabolism abnormalities that do yet not meet diabetes criteria. Stage 3 develops when the established glycemic thresholds for diabetes diagnosed are exceeded. Although remissions after Stage 1 are rare, the risk and rate of progression vary based upon genetics, age at seroconversion, autoantibody titers and body mass index .
Genetic Testing Could Help Identify Risk Of Type 1 Diabetes
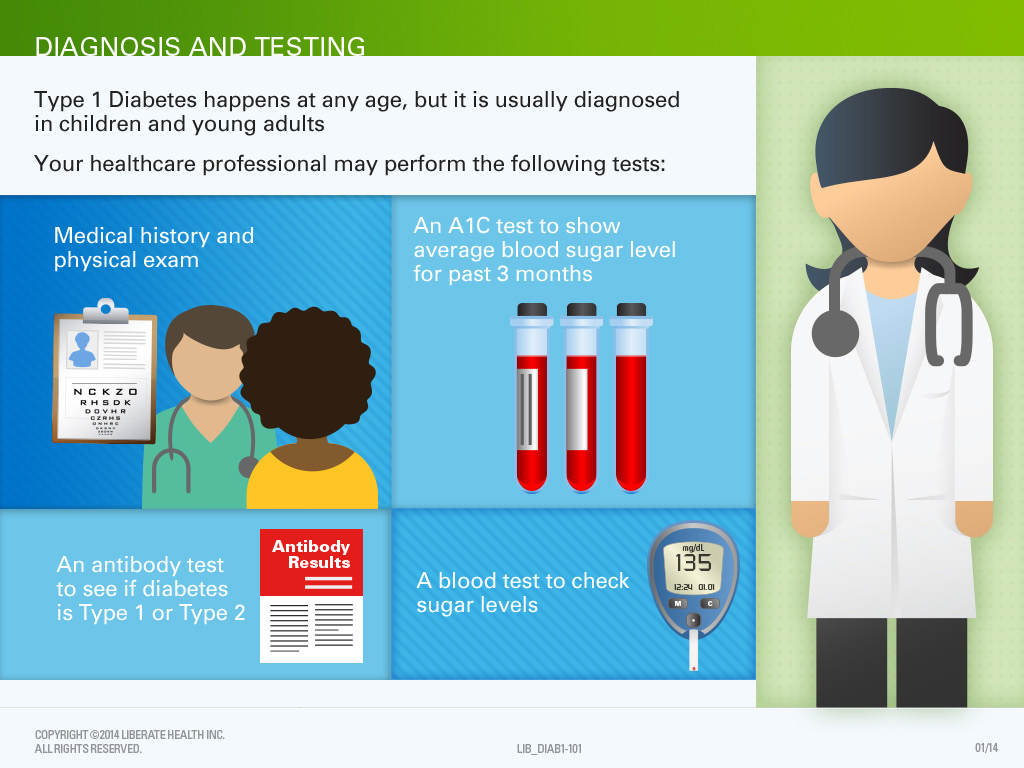
For many patients with type 1 diabetes, testing doesn’t begin until their symptoms land them in the emergency room. But researchers at the University of Virginia are trying to see if a genetic test can determine if someone is more likely to develop the disease.
NPR reports around 2,000 children have participated in the study so far, and about 60 of those children carry a higher genetic risk.
According to the U.S. Centers for Disease Control and Prevention, type 1 diabetes is typically diagnosed in children and teens, although adults can be diagnosed too. It could be months or years before symptoms become apparent.
Dr. Janette Nesheiwat, a board-certified physician in family and emergency medicine, told CBS News the the study is testing a simple cheek swab that could tell patients if they’re at a higher risk although that doesn’t mean they already have type 1 diabetes.
“The goal and purpose of this test is to give us an idea of whether parents should watch and monitor their children versus just waiting for something serious to happen,” she said.
Symptoms of diabetes can include fatigue, dizziness, weight loss, or an increased thirst or urination. In some cases, Nesheiwat said symptoms can become so severe that a patient collapses or suffers from a seizure.
You May Like: Can I Cure Diabetes With Diet
What Are Monogenic Forms Of Diabetes
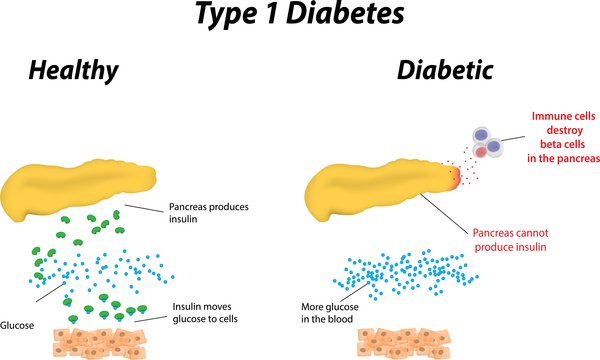
Some rare forms of diabetes result from mutations or changes in a single gene and are called monogenic. In the United States, monogenic forms of diabetes account for about 1 to 4 percent of all cases of diabetes.1,2,3,4 In most cases of monogenic diabetes, the gene mutation is inherited from one or both parents. Sometimes the gene mutation develops spontaneously, meaning that the mutation is not carried by either of the parents. Most mutations that cause monogenic diabetes reduce the bodys ability to produce insulin, a protein produced in the pancreas that helps the body use glucose for energy.
Neonatal diabetes mellitus and maturity-onset diabetes of the young are the two main forms of monogenic diabetes. NDM occurs in newborns and young infants. MODY is much more common than NDM and usually first occurs in adolescence or early adulthood.
Complete T1dgc Linkage Results
The total T1DGC collection of 4,422 ASPs constitutes the largest linkage study conducted for any disease. Results from the linkage analysis of the total dataset are presented in , and a summary is shown in . As expected, the evidence for linkage to the HLA region increased, with a peak LOD score of 398.6 , reinforcing the importance of this complex in the etiology of type 1 diabetes.
Chromosome 6 linkage was further examined, taking into account the HLA linkage that may mask other susceptibility loci on this chromosome. One way to account for this is by calculating the expected LOD based on the decay of linkage from HLA, assuming a Kosambi map function . Region showing linkage significantly higher than the ELOD may contain gene that affect type 1 diabetes risk. These analyses were carried out as previously described . This analysis showed additional linkage signals on chromosome 6q , which overlapped with the previously reported locus IDDM15 .
Recommended Reading: Cauliflower Pizza Crust For Diabetics
Whole Genome Sequencing For Type 1 Diabetes
Using very new genome technologies and cutting edge scientific methods, my team is embarking on a new program with the aim of functionally annotating the gene changes in type 1 diabetes. To start, we have sequenced the entire genomes of 50 individuals with type 1 diabetes.
Already, even at this early stage of this newest program, we have made an exciting discovery. We have shown how single-nucleotide polymorphism changes in one particular gene called A20 not only contributes to diabetes susceptibility, but also enhances rejection in islet transplantation.
This exciting data provides tantalising new information that will help to bring us closer to a better understanding of type 1 diabetes and hopefully, to a cure.
Every day, scientists all around the world are making progress toward a cure for type 1 diabetes. While it is difficult to say how long it will be before a cure is finally realised, we can reflect on how far we have come since the discovery of insulin in the early twentieth century, and look forward to more new and exciting discoveries that will bring us closer to a cure for type 1 diabetes.
How Is Mody Diagnosed
A blood sugar test is the first step toward diagnosing MODY. If your results indicate you have diabetes, your doctor may order additional tests to determine if you have MODY or another type of diabetes, such as type 1 or 2.
Since MODY is caused by a genetic mutation, a genetic test can also help diagnose it. This testing will determine the exact type of MODY.
MODY is caused by a genetic mutation passed on through the family. Theres currently no way to prevent or cure it, but it can be managed, and predicted. Knowledge is power.
Also Check: Safe Male Enhancement Pills For Diabetics
Dna Testing For Type 1 Diabetes
Type 1 Diabetes is the least common version of the condition, affecting around 5% of the 2.3 million people with diabetes in the UK. Often developing in people before the age of 40, type 1 diabetes occurs when the body fails to produce any insulin, which is a hormone that regulates the level of glucose found in the blood. Type 1 diabetes will produce many of the same symptoms as experienced by sufferers of type 2 diabetes, which includes excessive thirst, fatigue, weight loss and increased or more frequent urination. Other symptoms of type 1 diabetes tend to develop more rapidly than those of type 2 diabetes for instance, blurred vision, constipation, skin infections and genital thrush often take just a matter of days or weeks to become noticeable. Hyperglycaemia and hypoglycaemia can occur with either form of diabetes and both can be extremely dangerous if left untreated.
For support and more information about type 1 diabetes, please visit the Diabetes UK website, the largest charity in the UK devoted to the treatment and care of people with diabetes to improve the quality of life for people with the condition.