Obesity And Kidney Disease On The Rise In Patients With Type 1 Diabetes
Obesity and chronic kidney disease are on the rise among people with type 1 diabetes in the United States, according to a study published in The Journal of Clinical Endocrinology & Metabolism.
Patient records were sourced from the Geisinger Health System, which serves 40 counties in Pennsylvania. Patients with T1D and type 2 diabetes were retrospectively reviewed for trends in obesity and kidney function between 2004 and 2018. As a comparator group, adults without diabetes were assessed for trends using National Health and Nutrition Examination Survey data collected between 1999 and 2018.
The T1D and T2D groups were aged median 39 and 62 years, respectively, and the NHANES cohorts were aged median 43 years. In the T1D, T2D, and NHANES groups, 48.5%, 50.6%, and 51.7% were women and 91.2%, 93.6%, and 68.6% were White, respectively. Among the same 3 groups, 66.2%, 86.8%, and 26.9% had hypertension and 47.7%, 40.3%, and 25.8% used angiotensin-converting enzyme inhibitors, respectively.
Among the T1D cohorts, metformin was the most prescribed non-insulin medication. Metformin, glucagon-like peptide-one receptor agonists , and sodium-glucose transport protein 2 inhibitors use increased over time while sulfonylureas and thiazolidinediones use decreased over the study period.
Among the T1D cohort, low eGFR was associated with obesity , but was attenuated when adjusting for hypertension .Albuminuria trends were similar to low eGFR in the T1D cohort.
Reference
Strategy For Glycemic Control And Other Risk Factors
The primary goal of optimizing glycemic control to reduce the development of microvascular and macrovascular complications is universal. The medication regimen is based on the comfort of the patient and physician and should be individualized, especially as renal function changes.
For those who need insulin, MDI with an average of 4 daily injections is common. The closest approximation of physiologic insulin secretion can be achieved with an insulin pump delivering a continuous subcutaneous infusion. A single type of insulin is used in the pump such as a rapid-acting analog that serves as the basal, bolus and correction insulin. Insulin pumps require vigilance on the part of the patient and their use should be overseen by endocrinologists and experienced diabetes educators.
Continuous Glucose Monitoring Systems are available that can continually measure glucose levels. A small plastic catheter is inserted subcutaneously and measures glucose every 5 min. Patients can view this in real-time and detect upward and downward trends in glucose. The added benefit is that alarms for high and low readings can be set.
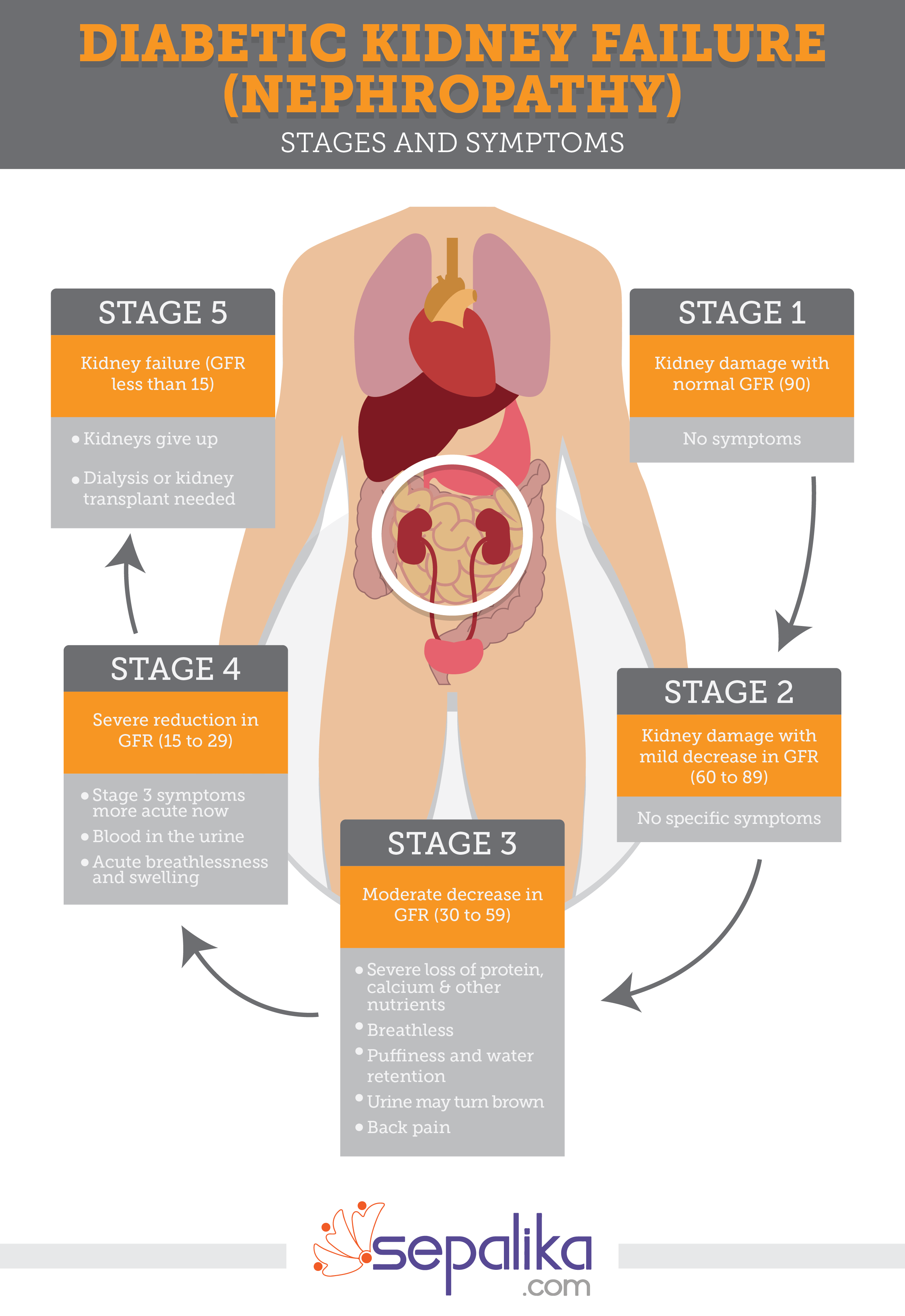
What Are The Symptoms
The kidneys work hard to make up for the failing capillaries so kidney disease produces no symptoms until almost all function is gone. Also, the symptoms of kidney disease are not specific. The first symptom of kidney disease is often fluid buildup. Other symptoms of kidney disease include loss of sleep, poor appetite, upset stomach, weakness, and difficulty concentrating.
It is vital to see a doctor regularly. The doctor can check blood pressure, urine , blood , and organs for other complications of diabetes.
Recommended Reading: Cinnamon For Diabetes Type 2
Hydrophilic Interaction Chromatographyultraperformance Liquid Chromatography
Fluorescently labeled N-glycans were separated by hydrophilic interaction chromatography on an ACQUITY ultraperformance liquid chromatography instrument , as described previously . Glycan peaks were pooled based on similar structural or compositional features of the peak glycan members. Chromatograms for the total and IgG N-glycans were separated into 39 and 24 peaks using manual integration of chromatograms and a semisupervised approach for the automatic chromatogram extraction , respectively. The amount of glycans in each peak was then expressed as a percentage of the total integrated area. The N-glycan traits are described in Supplementary Table 1.
What Is Renal Failure
In a research conducted by Ravi Retnakaran et al. entitled Risk Factors for Renal Dysfunction in Type 2 Diabetes, they confirm that type 2 diabetes was the leading cause of end-stage renal disease . While not all, many patients with type 2 diabetes will likely develop renal dysfunction during their lifetime. In the U.K. Prospective Diabetes Study, it was shown that 24.9% of patients developed microalbuminuria within 10 years of diagnosis of type 2 diabetes, but only 0.8% of those developed ESRD, as assessed by elevated plasma creatinine or the need for renal replacement therapy.
Each year, over 100,000 people will be diagnosed with kidney failure in the United States. Forty-four percent of these cases are caused by diabetes. It presents a significant financial burden, as well as a physical, mental and emotional on patients and their families, and accounts for 32 million in medical costs per year.
Renal failure is the end result of CKD . Renal failure, also known as nephropathy, renal insufficiency, or kidney failure, is a condition in which the kidneys do not function properly, and do not filter waste products from the blood. Renal failure is Filtering waste products from the blood is the main function of the kidneys.
Don’t Miss: How Many Carbs Should A Pre Diabetic Eat Per Day
How Do I Know If I Have Kidney Damage
Most people with early kidney damage do not have symptoms. The best way to find early kidney damage is to have a urine test once a year. This test checks for very small amounts of protein in the urine called albuminuria. It helps show kidney damage at an early stage in people with diabetes. Not everyone with kidney disease gets kidney failure. With the right treatment, you can prevent kidney disease from getting worse.
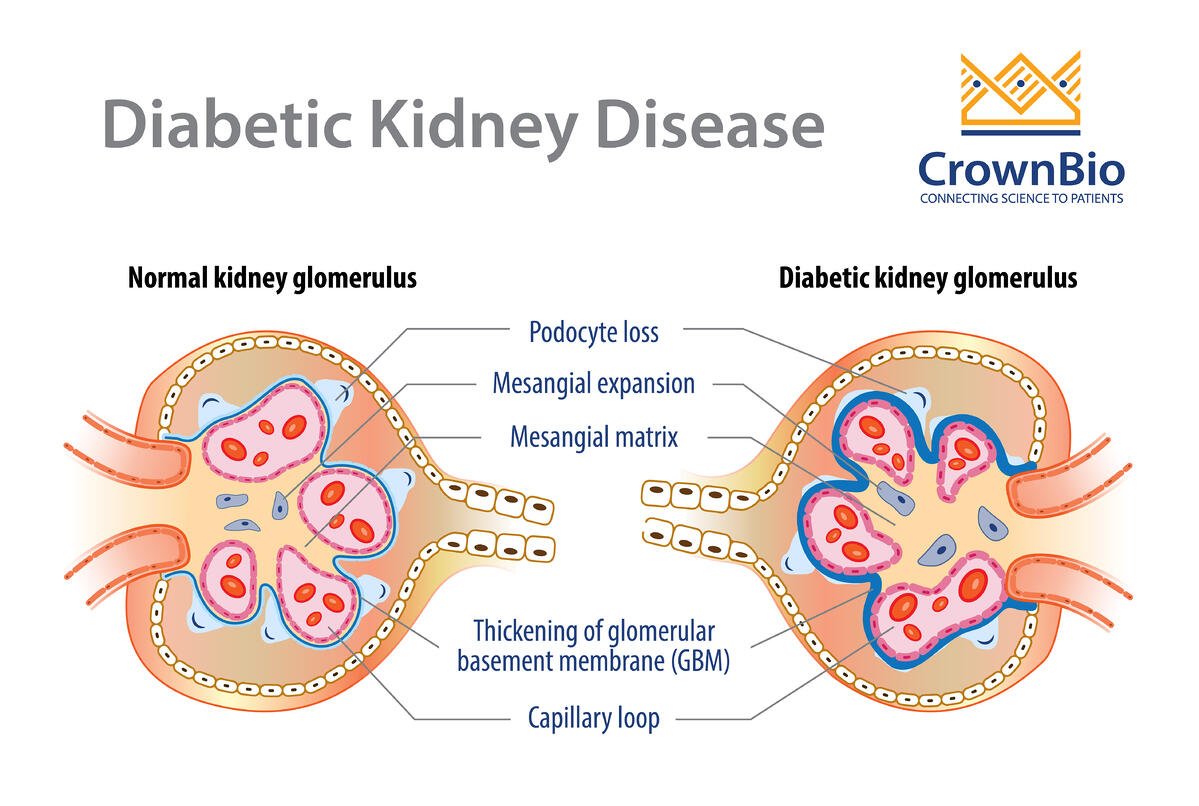
The Mechanism Is Unknown
It is clear that diabetes can lead to kidney disease, but just why high blood sugars should damage the glomeruli is unclear. High blood pressure is a known risk factor for kidney disease and people with diabetes are prone to hypertension. The renin-angiotensin system â which helps regulate blood pressure â is also thought to be involved in the development of diabetic nephropathy.Other risk factors include cigarette smoking and family history. Diabetic nephropathy progresses steadily despite medical intervention. However, treatment can significantly slow the rate of damage.
Don’t Miss: Does Viagra Work For Diabetics
What Is The Outlook
- If you have microalbuminuria , this may clear away, especially with treatment.
- If you have proteinuria , over time the disease tends to become worse and progress to end-stage kidney failure. However, the length of time this takes can vary and it may take years. If your kidneys do begin to fail you should be referred to a kidney specialist.
- Once the kidney function goes below a certain level then you will need kidney dialysis or a kidney transplant.
- A main concern is the increased risk of developing cardiovascular diseases. Cardiovascular diseases, such as heart attack and stroke, are the main causes of death in people with diabetic kidney disease. The treatments outlined above will reduce the risk of these occurring.
Tests For Kidney Disease
The two tests for kidney disease are included in your annual review. You should normally have these tests every year but they might be happening differently at the moment because of the coronavirus pandemic. we’ve got more advice about what care you can expect during this time.
As part of your 15 Healthcare Essentials, you should have both of the tests for kidney disease every year.
Read Also: Is Diabetes 2 An Autoimmune Disease
For People With Type 2 Diabetes
At the time the diabetes is first diagnosed, about 1 in 8 people have microalbuminuria and 1 in 50 have proteinuria. This is not because diabetic kidney disease happens straightaway in some cases but because many people with type 2 diabetes do not have their diabetes diagnosed for quite some time after the disease had begun.
Of those people who do not have any kidney problem when their diabetes is diagnosed, microalbuminuria develops in about 1 in 7 people and proteinuria in 1 in 20 people, within five years.
Diabetic kidney disease is much more common in Asian and black people with diabetes than in white people.
Diabetes And Chronic Kidney Disease
If you have diabetes, ask your doctor about kidney disease.
Chronic kidney disease often develops slowly and with few symptoms. Many people dont realize they have CKD until its advanced and they need dialysis or a kidney transplant to survive.
If you have diabetes, get your kidneys checked regularly, which is done by your doctor with simple blood and urine tests. Regular testing is your best chance for identifying CKD early if you do develop it. Early treatment is most effective and can help prevent additional health problems.
CKD is common in people with diabetes. Approximately 1 in 3 adults with diabetes has CKD. Both type 1 and type 2 diabetes can cause kidney disease.
- Kidney diseases are the 9th leading cause of death in the United States.
- Approximately 1 in 3 adults with diabetes has CKD.
- Every 24 hours, 170 people with diabetes begin treatment for kidney failure.
You May Like: A1 Diabetes And Medical Supply
Control Your Blood Pressure
Blood pressure is the force of your blood against the wall of your blood vessels. High blood pressure makes your heart work too hard. It can cause heart attack, stroke, and kidney disease.
Your health care team will also work with you to help you set and reach your blood pressure goal. The blood pressure goal for most people with diabetes is below 140/90 mm Hg. Ask your health care team what your goal should be.
Medicines that lower blood pressure can also help slow kidney damage. Two types of blood pressure medicines, ACE inhibitors and ARBs, play a special role in protecting your kidneys. Each has been found to slow kidney damage in people with diabetes who have high blood pressure and DKD. The names of these medicines end in pril or sartan. ACE inhibitors and ARBs are not safe for women who are pregnant.
What Is The Kidney Disease Solution Program Work
The ebook, cookbook, and audio guides people through the process step-by-step. The book contains tips on changing your lifestyle to improve the health of your kidneys. In addition the book provides recipes for supporting kidney function and health. Additionally, it offers some natural remedies that can aid in the treatment of your problem.
The audio materials provide guided meditation as well as Morning yoga flows. The audio guided meditation can be effective in relieving stress and improving sleep quality. Yoga flow exercises in the morning, led by renowned yogini Antonella Milo, are designed to energize you for the day while supporting kidney health.
The overall collection of products offers a comprehensive and natural method of treating kidney disease. Through simple lifestyle adjustments, releasing stress with meditation, and practicing yoga exercises, you can put an end to the pain and discomfort due to kidney diseases.
Also Check: Hiv And Diabetes Life Expectancy
How Are The Kidneys Kept Working As Long As Possible
The kidney doctor, called a nephrologist, will plan your treatment with you, your family and your dietitian. Two things to keep in mind for keeping your kidneys healthy are controlling high blood pressure in conjunction with an ACE inhibitor and following your renal diabetic diet. Restricting protein in your diet also might be helpful. You and your dietitian can plan your diet together.
Diet For Renal Failure
If you already have chronic renal failure, your doctor or dietician will want you to start on an eating plan called the Renal Diet.
Your kidneys are damaged therefore, your kidneys cannot handle a regular amount of protein as they could in the past. Your kidneys also cant handle excessive amount of salt or potassium, due to the kidneys role in regulating these electrolytes. If you choose not to decrease your protein, sodium, and potassium levels, it makes your kidneys work harder to filter waste, and you will experience ESRD sooner. A renal diet is lower in protein, fat, sodium or salt, and potassium. You will most likely be asked to:
- cut back on protein containing foods, especially animal products such as milk, eggs, and cheese
- eat a low fat diet that is also low in cholesterol, as your body cannot handle high cholesterol foods like it used to, and you will get plaque build-up in your arteries from all of the excessive cholesterol in your bloodstream
- avoid high salt or sodium in your diet, and keep sodium to 1500 mg/day to keep your blood pressure in a better range to protect your kidneys
- avoid excess potassium since your kidneys can no longer regulate this electrolyte. Potassium keeps your heart beating regularly and helps your muscles to work right, but kidney disease may result in high potassium levels, an irregular heartbeat, or even cardiac arrest. Avoid foods like apricots, oranges, potatoes and bananas, which are all high in potassium
Read Also: Can You Reverse Blindness From Diabetes
Causes Of Renal Failure
As we have said, diabetes is the cause of renal failure in almost half of all cases. From the chart below, we can see that the most prevalent cause of kidney failure is diabetes, followed by high blood pressure, glomerulonephritis, cystic diseases, urological diseases, and other factors.
How many people with diabetes actually get kidney failure?
From a study of veterans, we can see the prevalence of renal disease in those with diabetes is largely male and Caucasian. When looking at ESRD associated with diabetes, the prevalence was higher among males, and higher among those of the black population.
44,671 of the 415,910 veterans with diabetes had a diagnosis of any renal disease. With the average age of 67 years, about 98% were male and 60% were of white ethnicity. The prevalence of diabetic nephropathy was 6.0%. ESRD was present in 4.2% of subjects. ESRD caused by diabetes-associated prevalence was higher amongst black compared to white veterans and male compared female veterans.
Diabetes And Kidney Disease: Can It Be Reversed
September 30, 2020 by Diabetes Care
Kidney disease is a common complication of diabetes, and diabetes is the leading cause of kidney disease in Canada. It is estimated that 50% of people with diabetes will have signs of kidney damage in their lifetime. Read on to learn if it is possible to reverse diabetic kidney disease.
Read Also: Are Omelettes Good For Diabetics
Glycemic Goal To Attain A1c ~70 %
Glycemic control is essential to delay or possibly prevent nephropathy. In general, the recommended target A1c for diabetes control by the ADA has been less than or around 7 % . The ADA advises both higher or stricter A1c goals for certain populations . AACE suggests a goal A1c of 6.5 % in healthy patients who are at low risk for hypoglycemia but also acknowledges the goals need to be individualized . The 2007 Kidney Disease Outcomes Quality Initiative guidelines for Diabetes and CKD endorse a target A1c of < 7.0 % but their updated 2012 guidelines instead recommend an A1c of ~7.0 % .
The ACCORD study showed higher risk of hypoglycemia and mortality in patients with type 2 diabetes treated with intensive glucose control , without any risk reduction on CVD. The increased mortality could not be attributed to hypoglycemia . In the ADVANCE trial, more intensive glycemic control showed no reduction in CVD. However, the intensive group had a 21 % reduction in nephropathy . The VADT study also showed no benefit on CVD risk with stricter glucose control .
The data clearly show that lowering A1c leads to benefit in regards to nephropathy. Benefits in A1c reduction are also seen on rates of retinopathy and neuropathy. However, the effect of lowering A1c is much less in regards to macrovascular disease. Thus, it is reasonable that a target A1c ~7.0 % offers an optimal risk to benefit ratio rather than a target that is considerably lower.
Yearly Screening For Kidneys
- Microalbumin or ACR urine test
Besides practicing good self-management skills and keeping your A1C below 7 percent, you should also get annual screenings to make sure that diabetes is not damaging your kidneys. A microalbumin test should be done on diagnosis of diabetes, then yearly. The laboratory will need to get a urine specimen to perform this test. If you do have protein in your urine, your doctor may want you to see a Registered Dietician to discuss reduction of salt and protein in your diet to help keep your kidneys safe. A value less than 30 is considered normal. In other words, you dont have much protein spilling into your urine. This is a good thing.
- Glomerular Filtration Rate
The estimated Glomerular Filtration Rate should also be done to make sure your kidneys are working like they should. Less than 60 ml/minute can signal kidney disease. A GFR should be done on diagnosis, and then yearly .
You May Like: Diabetes Injection Pen For Weight Loss
What About A Kidney Transplant
Dialysis saves lives for those with chronic kidney failure, but it serves to provide only about ten percent of a normally functioning kidneys ability to filter wastes from the body. In addition, dialysis can cause other serious health issues including:
- anemia or decreased number of normal red blood cells
- nerve damage
- high blood pressure
Medical Therapy In Dialysis And Post

There are a few oral agents that can be used safely in patients on dialysis, particularly if the diabetes is fairly mild. Most others, however, will need insulin for glycemic control.
Patients receiving hemodialysis can have different clearance rates of insulin that may be affected by the timing of dialysis. We have done continuous glucose monitoring on patients undergoing HD and found that patients glycemic responses during HD are quite idiosyncratic and their insulin regimens need to be individualized to avoid both hyper-and hypoglycemia during and after HD. Patients who are on peritoneal dialysis have exposure to large amounts of glucose in the dialysate that can lead to uncontrolled hyperglycemia. In patients receiving PD continuously, a standard basal/bolus insulin regimen is best. However, with overnight PD using a cycler, coverage of the increased glucose load may best be accomplished using a fixed mixture insulin combination, such as 70/30 or 75/25 insulins, given at the onset of PD. The nephrologist prescribing the PD will often change the glucose concentration of the dialysate because of the need for more or less fluid removal and such changes need to be discussed with the endocrinologist so that the insulin doses may be appropriately changed.
You May Like: How Many Carbs In A Low Carb Diet For Diabetics