Management Of Hyperglycemia In Type 2 Diabetes 2022 A Consensus Report By The American Diabetes Association And The European Association For The Study Of Diabetes
Diabetes Care
Melanie J. Davies, Vanita R. Aroda, Billy S. Collins, Robert A. Gabbay, Jennifer Green, Nisa M. Maruthur, Sylvia E. Rosas, Stefano Del Prato, Chantal Mathieu, Geltrude Mingrone, Peter Rossing, Tsvetalina Tankova, Apostolos Tsapas, John B. Buse Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association and the European Association for the Study of Diabetes . Diabetes Care 1 November 2022 45 : 27532786.
What Is The A1c Test
The A1C test is a simple blood test that measures your average blood sugar levels over the past 2 or 3 months. The test is done at a lab or your doctors office in addition tonot instead ofregular blood sugar testing you do yourself.
A1C testing is part of the ABCs of diabetesimportant steps you can take to prevent or delay health complications down the road:
- A: Get a regular A1C test.
- B: Try to keep your blood pressure below 140/90 mm Hg .
- C: Manage your cholesterol levels.
- s: Stop smoking or dont start.
The A1C goal for most adults with diabetes is between 7% and 8%, but your goal may be different depending on your age, other health conditions, medicines youre taking, and other factors. Work with your doctor to establish a personal A1C goal for you.
Glycemic Targets In The Non
3.1 We recommend a premeal glucose target of less than 140 mg/dl and a random BG of less than 180 mg/dl for the majority of hospitalized patients with non-critical illness.
3.2 We suggest that glycemic targets be modified according to clinical status. For patients who are able to achieve and maintain glycemic control without hypoglycemia, a lower target range may be reasonable. For patients with terminal illness and/or with limited life expectancy or at high risk for hypoglycemia, a higher target range may be reasonable.
3.3 For avoidance of hypoglycemia, we suggest that antidiabetic therapy be reassessed when BG values fall below 5.6 mmol/liter . Modification of glucose-lowering treatment is usually necessary when BG values are below 3.9 mmol/liter .
Recommended Reading: Most Accurate Blood Glucose Meter 2021
Key Knowledge Gaps And A Call To Action
In this 100th year since the discovery and partial purification of insulin, we should remember the remarkable speed at which this first glucose-lowering medication was developed and distributed as life-saving therapy for people with diabetes. Through our experience in the last few years with the COVID-19 pandemic, we have demonstrated how quickly many governments, industry, health care systems, and academic institutions can respond to global health care crises. Within a year of identification of the severe acute respiratory syndrome coronavirus 2 virus, preventive and therapeutic products were not only developed and tested but also administered on a massive scale. The annual global mortality rate directly attributable to diabetes is approximately 1.5 million people, with 540 million people affected . Although not as spectacular as the impact of COVID-19 on the health of society, diabetes is sure and steady in its burden, increasing in prevalence and with an increase in mortality and morbidity over time.
Weight management. With the emergence of more effective behavioral and medical therapies and novel surgical approaches for the treatment of people who are overweight with diabetes, more direct comparisons are required to better target interventions based on impact and cost-effectiveness.
Glucose monitoring. Further studies to understand the role and optimal implementation of CGM and/or episodic CGM in type 2 diabetes are needed.
What Are Blood Sugar Targets
A blood sugar target is the range you try to reach as much as possible. These are typical targets:
- Before a meal: 80 to 130 mg/dL.
- Two hours after the start of a meal: Less than 180 mg/dL.
Your blood sugar targets may be different depending on your age, any additional health problems you have, and other factors. Be sure to talk to your health care team about which targets are best for you.
Read Also: Doterra Essential Oils For Diabetes
What Can Happen If Blood Sugars Are High
In the short term, high blood sugars can turn into diabetic ketoacidosis . This is an emergency condition that needs treatment right away. DKA can happen to kids with type 1 diabetes and, less often, kids with type 2 diabetes. Kids with type 2 diabetes also can get another type of emergency called hyperosmotic hyperglycemic state . Both conditions need treatment in the hospital and are very serious.
Untreated hyperglycemia can lead to serious health problems later in life. If it happens a lot, it can harm blood vessels, the heart, kidneys, eyes, and nerves.
Sodiumglucose Cotransporter 2 Inhibitors
The major change in treatment options since the publication of the 2012 position statement has been the availability of a new class of glucose-lowering drugs, the sodiumglucose cotransporter 2 inhibitors . These agents reduce HbA1c by 0.51.0% versus placebo . When compared with most standard oral agents in head-to-head trials, they appear to be roughly similarly efficacious with regard to initial HbA1c lowering . Their mechanism of action involves inhibiting the SGLT2 in the proximal nephron, thereby reducing glucose reabsorption and increasing urinary glucose excretion by up to 80 g/day . Because this action is independent of insulin, SGLT2 inhibitors may be used at any stage of type 2 diabetes, even after insulin secretion has waned significantly. Additional potential advantages include modest weight loss and consistent lowering of systolic and diastolic blood pressure in the order of 24/12 mmHg . Their use is also associated with reductions in plasma uric acid levels and albuminuria , although the clinical impact of these changes over time is unknown.
Properties of available glucose-lowering agents in the U.S. and Europe that may guide individualized treatment choices in patients with type 2 diabetes
| Class . |
|---|
Data on microvascular outcomes with SGLT2 inhibitors are lacking . Effects on macrovascular disease are also unknown cardiovascular safety trials are currently in progress .
You May Like: Best Vitamin C Supplement For Diabetics
How To Prevent Hyperglycaemia And Lower Your Blood Sugar Levels
Testing your blood sugar levels regularly can help you spot the signs of hyperglycaemia. But there are some steps you can take to either prevent a hyper from happening or to bring down your blood sugar levels.
You can start by making sure you are aware of your carbohydrate portions and how they may be affecting your blood sugar levels after eating. Carb countingis one of the ways you can manage this. Avoid foods that have a high glycemic index and choose low GI foods that can help manage your blood sugar levels more effectively. Increase the fibre in your diet. This can help slow down carbohydrate digestion, which can help limit the rise in your blood sugars.
Try to maintain a healthy weight as this promotes regular blood sugar levels in the body. Be as active as possible, regular exercise can help your body process more of the sugar.
Remember to take your insulin and other diabetes medication, and always take them correctly. Continue to take your diabetes medication even if you are ill and not eating.
Concentrate on your emotional wellbeing, get a quality nights sleep and find ways to manage your stress. Stress can cause hormones to be released, which keep your blood sugar levels high.
If your blood sugar levels continue to be high, or youre unsure of what to do, contact your doctor for further guidance.
What If It Goes Untreated
Hyperglycemia can be a serious problem if you don’t treat it, so it’s important to treat as soon as you detect it. If you fail to treat hyperglycemia, a condition called ketoacidosis could occur. Ketoacidosis develops when your body doesn’t have enough insulin. Without insulin, your body can’t use glucose for fuel, so your body breaks down fats to use for energy.
When your body breaks down fats, waste products called ketones are produced. Your body cannot tolerate large amounts of ketones and will try to get rid of them through the urine. Unfortunately, the body cannot release all the ketones and they build up in your blood, which can lead to ketoacidosis.
Ketoacidosis is life-threatening and needs immediate treatment. Symptoms include:
- Shortness of breath
Talk to your doctor about how to handle this condition.
Don’t Miss: How Often Can I Take Insulin
Glycemic Goals Of Therapy
Controlled clinical trials, such as the Diabetes Control and Complications Trial and the Stockholm Diabetes Study in type 1 diabetes and the UK Prospective Diabetes Study and Kumamoto study in type 2 diabetes, have helped to establish the glycemic goals of therapy that result in improved long-term outcomes. The clinical trials, in concert with epidemiological data , support decreasing glycemia as an effective means of reducing long-term microvascular and neuropathic complications. The most appropriate target levels for blood glucose, on a day-to-day basis, and A1C, as an index of chronic glycemia, have not been systematically studied. However, both the DCCT and the UKPDS had as their goals the achievement of glycemic levels in the nondiabetic range. Neither study was able to maintain A1C levels in the nondiabetic range in their intensive treatment groups, achieving mean levels over time of 7%, which is 4 SDs above the nondiabetic mean.
Assiduous attention to abnormalities other than hyperglycemia that accompany type 2 diabetes, such as hypertension and dyslipidaemia, has been shown to improve microvascular and cardiovascular complications. Readers are referred to published guidelines for a discussion of the rationale and goals of therapy for the nonglycemic risk factors, as well as recommendations on how to achieve them .
What Causes Low Blood Sugar
Low blood sugar has many causes, including missing a meal, taking too much insulin, taking other diabetes medicines, exercising more than normal, and drinking alcohol. Blood sugar below 70 mg/dL is considered low.
Signs of low blood sugar are different for everyone. Common symptoms include:
Know what your individual symptoms are so you can catch low blood sugar early and treat it. If you think you may have low blood sugar, check it even if you dont have symptoms. Low blood sugar can be dangerous and should be treated as soon as possible.
Read Also: 30 Carb Meals For Diabetics
Initial Combination Therapy Compared With Stepwise Addition Of Glucose
Consensus recommendation
-
The stepwise addition of glucose-lowering medication is generally preferred to initial combination therapy.
In most patients, type 2 diabetes is a progressive disease, a consequence generally attributed to a steady decline of insulin secretory capacity. The practical impact of gradual loss of -cell function is that achieving a glycemic target with monotherapy is typically limited to several years. Stepwise therapy is supported by clinical trials . While there is some support for initial combination therapy due to the greater initial reduction of HbA1c than can be provided by metformin alone , there is little evidence that this approach is superior to sequential addition of medications for maintaining glycemic control or slowing the progression of diabetes. However, since the absolute effectiveness of most oral medications rarely exceeds an 11 mmol/mol reduction in HbA1c, initial combination therapy may be considered in patients presenting with HbA1c levels more than 17 mmol/mol above their target. Fixed-dose formulations can improve medication adherence when combination therapy is used , and may help achieve glycemic targets more rapidly . Potential benefits of combination therapy need to be weighed against the exposure of patients to multiple medications and potential side effects, increased cost, and, in the case of fixed combination medications, less flexibility in dosing.
Patient And Professional Education
8.1 We recommend diabetes self-management education targeting short-term goals that focus on survival skills: basic meal planning, medication administration, BG monitoring, and hypoglycemia and hyperglycemia detection, treatment, and prevention.
8.2 We recommend identifying resources in the community to which patients can be referred for continuing diabetes self-management education after discharge.
8.3 We recommend ongoing staff education to update diabetes knowledge, as well as targeted staff education whenever an adverse event related to diabetes management occurs.
Don’t Miss: How Much Is Insulin At Walmart
Facilitating Healthy Behaviors And Weight Management
Promotion of healthy behaviors is central to the holistic management of type 2 diabetes and should be addressed at the time of diagnosis and throughout the course of diabetes. Healthy behaviors include healthy nutrition, regular physical activity, adequate sleep, and smoking cessation. Health behaviors should always be assessed and addressed when glycemic targets are not met and when new pharmacotherapy or interventions are initiated.
All individuals with type 2 diabetes should be offered MNT to develop a personal food plan in the context of diabetes. The need for additional dietary advice should be reevaluated over time . There is no single dietary pattern recommended for all individuals with type 2 diabetes many dietary patterns can be effective for achieving treatment goals, and a structured food plan should be based on an individual persons preferences and context.
SMART goals are more effective for achieving behavior change than nonspecific recommendations . An all or none approach related to behavioral goals should be avoided, as any improvement in healthy behaviors can have a positive impact in diabetes . Self-monitoring of achievements is crucial to the achievement of health behavior goals . Behavioral health specialists or psychologists with specific training in behavior change interventions can be of particular value as members of the team to help the person with type 2 diabetes achieve goals.
Practical Tips for Clinicians
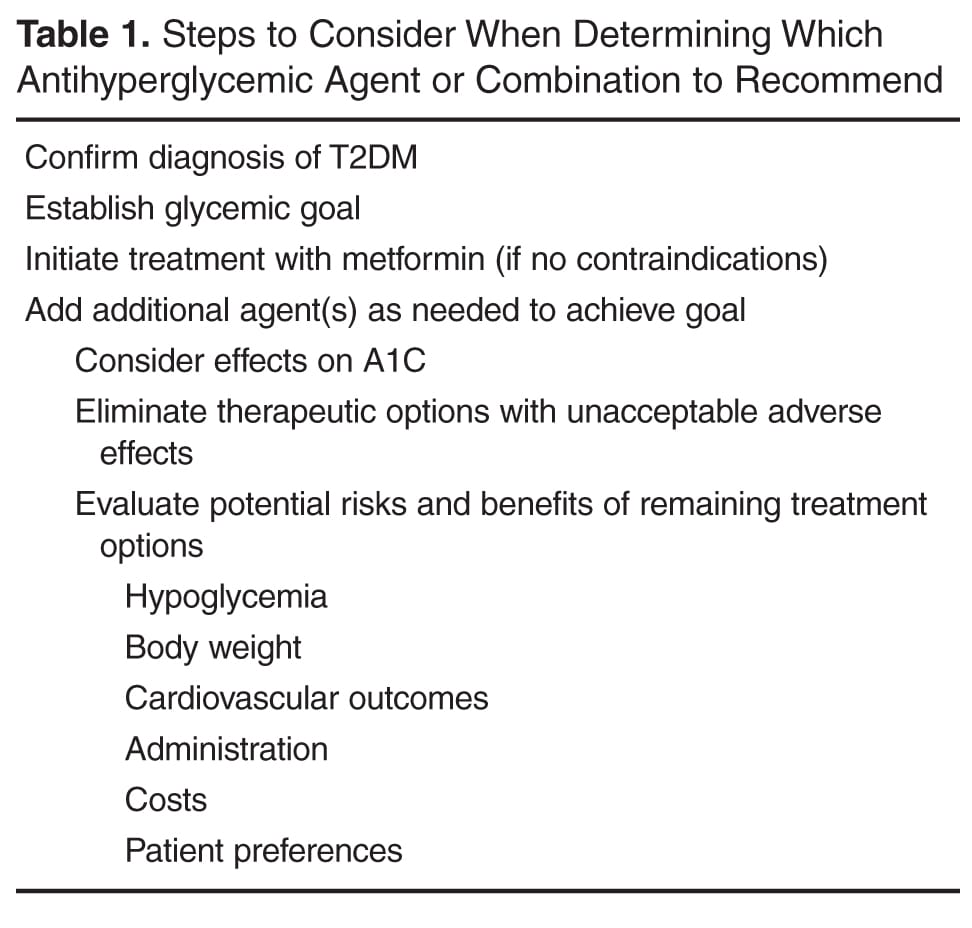
Addition Of A Second Medication
If lifestyle intervention and the maximal tolerated dose of metformin fail to achieve or sustain the glycemic goals, another medication should be added within 23 months of the initiation of therapy or at any time when the target A1C level is not achieved. Another medication may also be necessary if metformin is contraindicated or not tolerated. The consensus regarding the second medication added to metformin was to choose either insulin or a sulfonylurea . As discussed above, the A1C level will determine in part which agent is selected next, with consideration given to the more effective glycemia-lowering agent, insulin, for patients with an A1C level of > 8.5% or with symptoms secondary to ehyperglycemia. Insulin can be initiated with a basal insulin . However, many newly diagnosed type 2 diabetic patients will usually respond to oral medications, even if symptoms of ehyperglycemia are present .
Read Also: Metene Td-4116 Blood Glucose Test Strips
How Can I Treat Low Blood Sugar
If youve had low blood sugar without feeling or noticing symptoms , you may need to check your blood sugar more often to see if its low and treat it. Driving with low blood sugar can be dangerous, so be sure to check your blood sugar before you get behind the wheel.
Carry supplies for treating low blood sugar with you. If you feel shaky, sweaty, or very hungry or have other symptoms, check your blood sugar. Even if you dont have symptoms but think you may have low blood sugar, check it. If your blood sugar is lower than 70 mg/dL, do one of the following immediately:
- Take four glucose tablets.
- Drink four ounces of fruit juice.
- Drink four ounces of regular soda, not diet soda.
- Eat four pieces of hard candy.
Wait for 15 minutes and then check your blood sugar again. Do one of the above treatments again until your blood sugar is 70 mg/dL or above and eat a snack if your next meal is an hour or more away. If you have problems with low blood sugar, ask your doctor if your treatment plan needs to be changed.
Epidemiology And Health Care Impact
Both the prevalence and incidence of type 2 diabetes are increasing worldwide, particularly in developing countries, in conjunction with increased obesity rates and westernization of lifestyle. The attendant economic burden for health care systems is skyrocketing, owing to the costs associated with treatment and diabetes complications. Type 2 diabetes remains a leading cause of cardiovascular disorders, blindness, end-stage renal failure, amputations, and hospitalizations. It is also associated with increased risk of cancer, serious psychiatric illness, cognitive decline, chronic liver disease, accelerated arthritis, and other disabling or deadly conditions. Effective management strategies are of obvious importance.
Also Check: Type 2 Diabetes And Eyes
Treating And Managing Hyperglycaemia
If your blood sugar level is slightly high for a short time, emergency treatment wont be necessary. But if it continues to rise you may need to act fast to avoid developing diabetic ketoacidosis .
If your blood sugar level is 15 mmol/l or more, you should check your blood or urine for ketones. If ketones are present, it is likely that you do not have enough insulin in your body. This means you may need to increase your dose or give yourself an extra dose. Talk to your diabetes team about how to do this if you are unsure.
You should also try to drink plenty of sugar-free fluids to prevent dehydration. And if you are feeling unwell, especially if you are vomiting, you should follow any sick day rules you have been given and contact your diabetes healthcare team for advice.
Advancing To Dual Combination And Triple Combination Therapy
While the SGLT2 inhibitors are approved as monotherapy, they are mainly used in combination with metformin and/or other agents . Given their demonstrated efficacy and clinical experience to date, they are reasonable options as second-line or third-line agents . Similar to most combinations, efficacy may be less than additive when SGLT2 inhibitors are used in combination with DPP-4 inhibitors . There are no data available on the use of SGLT2 inhibitors in conjunction with GLP-1 receptor agonists an evidence-based recommendation for this combination cannot be made at this time.
As noted in the original position statement, initial combination therapy with metformin plus a second agent may allow patients to achieve HbA1c targets more quickly than sequential therapy. Accordingly, such an approach may be considered in those individuals with baseline HbA1c levels well above target, who are unlikely to successfully attain their goal using monotherapy. A reasonable threshold HbA1c for this consideration is 9% . Of course, there is no proven overall advantage to achieving a glycemic target more quickly by a matter of weeks or even months. Accordingly, as long as close patient follow-up can be ensured, prompt sequential therapy is a reasonable alternative, even in those with baseline HbA1c levels in this range.
Also Check: Pendulum Life Glucose Control Reviews