How Long Does Lantus Solostar Last Once I Have Started Using It
The Lantus SoloStar pens expiry, once you have started using it, is 28 days. If you are on a low dose then one Lantus SoloStar pen may contain more than 28 days worth of insulin. In this case it is important to remember to discard the remaining Lantus SoloStar pen 28 days after you have started using it, even if it still contains insulin.
Once you have started using Lantus SoloStar it should be kept at room temperature and NOT in the refrigerator.
You’ll Need To Calculate Some Of Your Insulin Doses
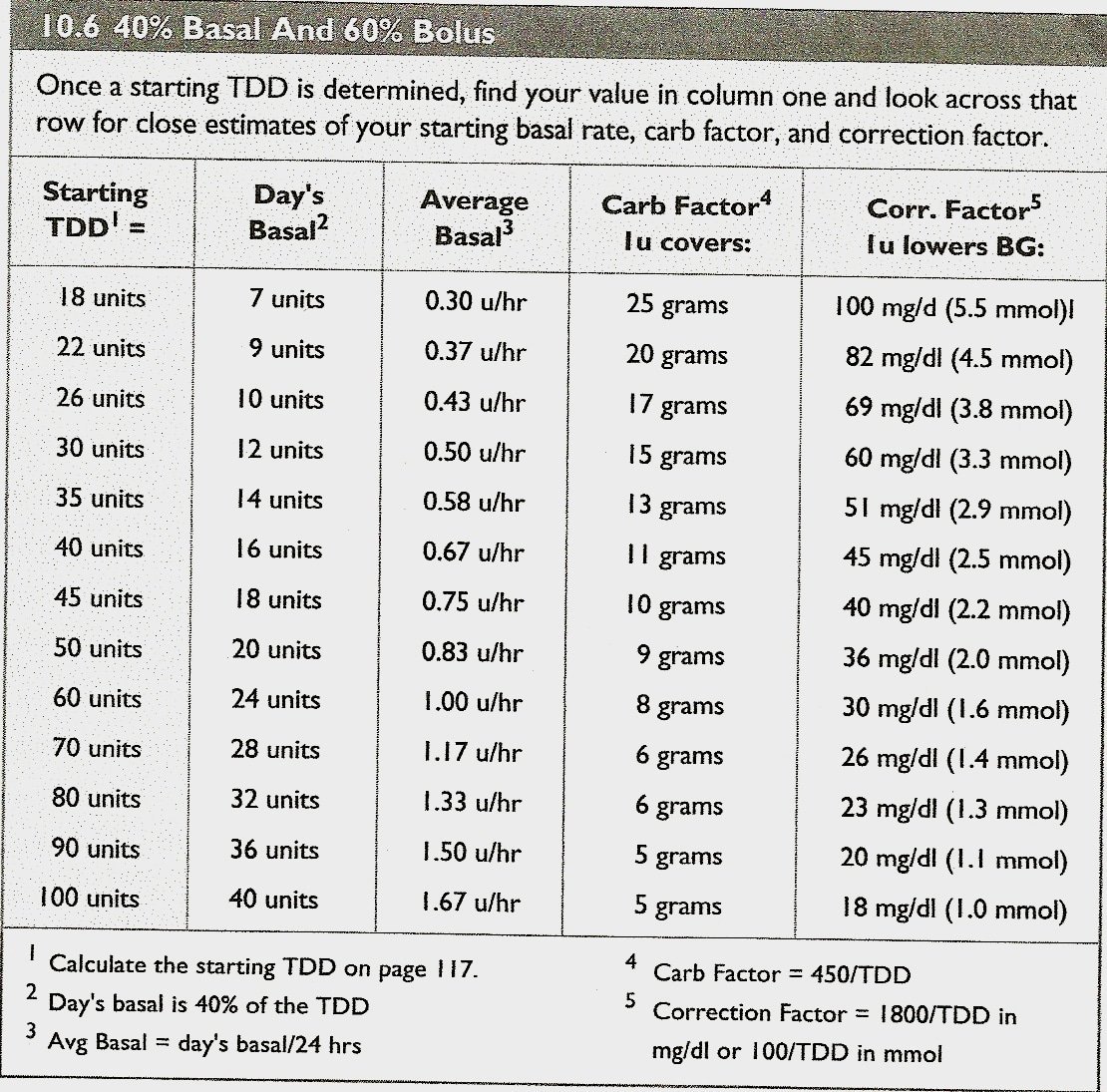
You’ll also need to know some basic things about insulin. For example, 40-50% of the total daily insulin dose is to replace insulin overnight.
Your provider will prescribe an insulin dose regimen for you however, you still need to calculate some of your insulin doses. Your insulin dose regimen provides formulas that allow you to calculate how much bolus insulin to take at meals and snacks, or to correct high blood sugars.
Calculate The Insulin Requirements To Cover The Carbohydrate
Measure the carbs in your meals correctly. Then you can calculate the insulin requirements to cover this carbohydrate using the below formula.
Insulin to cover the carbohydrate = Grams of carb/I:C ratio .
For example, if your meal time carbohydrate is 50 grams, then your insulin requirement to cover the carbohydrate = 50/14.28 = 3.5 units for regular insulin = 50/12.28 = 4 units of insulin to cover 50 grams of carbohydrate.
Recommended Reading: Blood Levels Diabetes Type 2
How Much Does A Vial Of Insulin Cost
In the United States, the price of a vial of insulin is around $200 without health insurance According to a 2018 report, you can find over-the-counter insulins sold at Walmart for as little as $25 per vial, while the newest insulins cost between $175 and $300 per vial.
Using human insulin sold at Walmart may have serious consequences on your blood sugar levels and diabetes management. These insulins do not work the same way as analog insulins do. They may have different times of action, peak times, as well as reduced effectiveness. Always ask for your doctors advice before using a different brand of insulin than the one youve been prescribed.
Related article:What happens if you miss a dose of insulin?
Insulin is a very expensive medicine. Keep your vials safe, and protect them from shattering and bacterial contamination. Use a silicon insulin vial protector like the ones from 4AllFamily. These little things can make you save hundreds of dollars worth of medicine!
Dont Miss: 6.5 A1c To Glucose
Example #: Carbohydrate Coverage At A Meal
First, you have to calculate the carbohydrate coverage insulin dose using this formula:
CHO insulin dose = Total grams of CHO in the meal ÷ grams of CHO disposed by 1 unit of insulin .
For Example #1, assume:
- You are going to eat 60 grams of carbohydrate for lunch
- Your Insulin: CHO ratio is 1:10
To get the CHO insulin dose, plug the numbers into the formula:
CHO insulin dose =
- The carbohydrate coverage dose is 6 units of rapid acting insulin.
- The high blood sugar correction dose is 2 units of rapid acting insulin.
Now, add the two doses together to calculate your total meal dose.
Carbohydrate coverage dose + high sugar correction dose = 8 units total meal dose!
The total lunch insulin dose is 8 units of rapid acting insulin.
You May Like: How Do You Know Diabetes Is Affecting Your Eyes
Rationale Of The Week
Our March 23rd Question caused a lot of commotion. Less than half of respondents chose the best answer, so we wanted to dive deeper into this question of how many pens are needed.
Before we start though, if you dont want any spoilers and havent tried the question yet, you can answer below: Answer Question
Question: JR is 24 years old and uses an insulin pen for their basal insulin injections each evening. JR takes 30 units a night and each insulin pen holds 300 units of insulin.
How many insulin pens would JR need for one month?
Answer Choices:
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 4, and finally option 3.
Lets Look At An Example
Lets say that you check your blood sugar before a meal and its 170. Youll need 1 unit to adjust to your target of 120.
If you plan to eat a meal that has 60 grams of carbohydrates, youll need to give yourself 6 units of insulin to adjust for your meal.
This means youll need 7 units total.
If your child needs help learning to calculate their insulin needs, Childrens Healthcare of Atlanta has created a helpful worksheet just for this.
Remember, there are two components to insulin correction:
- your blood sugar levels before your meal
- corrections for the carbohydrates you eat
Combine both of these when considering how much insulin to inject.
You May Like: What Symptoms Will A Diabetic Experience
How Much Insulin Should I Take For Low Blood Sugar
Insulin will lower your blood sugar. If your blood sugar is already low, you shouldnt inject more insulin.
Signs that your blood sugar is too low include sweating, dizziness, blurred vision, and significant fatigue. If this happens, try to consume rapid-acting carbohydrates, like sugared sodas, fruit juice, or glucose tablets, to get your blood sugar levels back up quickly.
How To Calculate How Many Insulin Pens Per Month
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
Also Check: Bydureon For Weight Loss In Non Diabetics
Factors Affecting Starting And Incremental Doses
As shown in Table 3, a significantly reduced starting dose as compared to the optimal dose was prescribed for patients with eGFR below 60 mL/min/1.73 m2 , those with retinopathy , those with concomitant sulfonylurea use , and women . In checking the factors affecting incremental dose by the comparison of linear regression lines for subcategories, only duration of diabetes was a statistically significant factor affecting the association between changes in dose and HbA1c. An inverse linear trend was observed among patients with a duration of diabetes 5 yrs while there was no trend among those with a duration < 5 yrs .
Prescribing Insulin In Enterprise Rx For Practice Partner 112 Users
Topics:Practice Partnermedisoft clinicalLytec MD
Important prescribing information for users of Practice Partner, Medisoft Clinical and Lytec MD.
Under the new Scripts2017 regulations from NCPDP Vial and Pen are no longer available units during the prescribing process.
The upgrade to the newest version 11.2* of Practice Partner,Medisoft Clinical or Lytec MD EHR provides a significantly improved prescribing process giving providers new tools to allow them to quickly and easily prescribe and manage patient medications and pharmacies.
However to comply with the new regulations there are some changes to existing workflows and processes that providers need to be aware of.
One of those changes is how Insulin is now prescribed for user of the 11.2 version.
The steps below outline the new process to prescribe Insulin in v11.2
Writing the insulin prescriptions:
-
The medication needs to be prescribed in Milliliters . The pharmacist will convert the milliliters ordered to the appropriate number of vials or pens based on the drug name entered.
Calculate the number of milliliters:
-
Take the total max daily dose and multiply by the number of days supply to be prescribed.
-
Divide the total by the number of units per ml
-
Round the result to the next whole number
Example of prescribing by vial: HumaLOG U-100 Insulin, max daily dose 50 units daily, with a 90 day supply.
- Review the package size: HumaLOG U-100 Insulin 100 unit/mL subcutaneous Vial VIAL 10 ml
Also Check: Does Water And Baking Soda Help Diabetes
Calculate The Bs Correction Insulin Dose
When your blood-glucose level goes high, a correct amount of bolus can help to bring it back to normal.
BS insulin correction dose = / BS correction factor
For example, if the present blood sugar number is 200 mg/dl and your target is 110 mg/dl, then BS insulin correction dose = /43 = 2 units and for Humalog or Novolog insulin sensitivity factor of 51 mg/dl = /51 = 1.8 units.
Usual Adult Dose For Diabetes Type 1
Note: Regular human insulin is available in 2 concentrations: 100 units of insulin per mL and 500 units of insulin per mL Doses should be individualized based on patient’s metabolic needs, blood glucose monitoring results, and glycemic goals
- Total daily insulin requirements are generally between 0.5 to 1 unit/kg/day
Insulin U-100 :
- Insulin U-100 should generally be used in a regimen with an intermediate or long-acting insulin
- Humulin R: Dilute to a concentration of 0.1 to 1 unit/mL in an infusion system using polyvinyl chloride infusion bags this insulin is stable in normal saline
- Administer U-500 insulin subcutaneously 2 to 3 times a day approximately 30 minutes prior to start of a meal
- The safety and efficacy in combination with other insulins has not been determined.
Recommended Reading: What Is A Good Meal Plan For Diabetics
Example: Calculating The Bolus Dose
The following lunch contains 80g carbs .
With an ICR of 1 unit of insulin for every 10g carbs, you would need to inject 8 units of insulin for the lunch above.
Alternatively, if you are counting in carbohydrate portions and have an ICR of 1 unit for every 1 CP, you would calculate the insulin dose in the following way, which has the same result of 8 units for the lunch above.
Using A Cf To Correct A 2 Hour Post Meal Blood Sugar
Correcting for a high blood sugar 2 hours after eating is using your best estimate!
Things to consider:
- how your insulin works
- the type of meal you ate – high fat carbohydrate meal vs. high fibre, low fat carbohydrate meal
- is it the type of meal that makes your blood sugars higher than usual for a longer than usual time, or
- is it the type of where your blood sugars return to normal within the 2 hours
Remember how your insulin works insulin action or duration of effect.
Rapid acting
- starts: 10-15 minutes
Also Check: Does Diabetes Weaken The Immune System
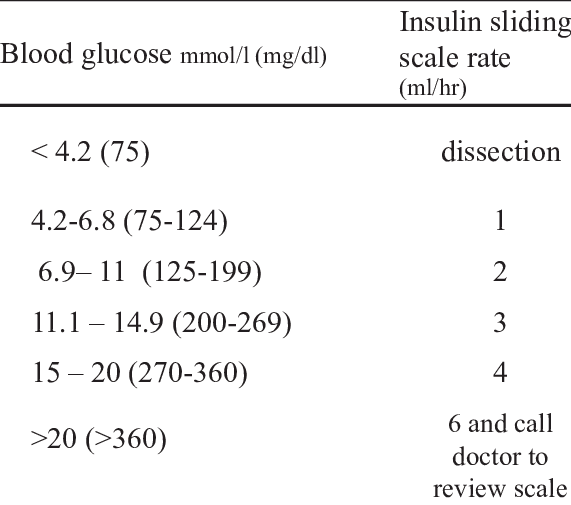
Calculating A Bolus Dose For High Blood Glucose
- Use the high blood glucose correction factor, also called correction factor or sensitivity. Use this to calculate the correction bolus.
- Correction factor is how much 1 unit of rapid-acting insulin will reduce the blood glucose number.
- The target number is the blood glucose number that you want.
NOTE: You should not need to correct a high blood glucose with each meal. If you need insulin to correct high blood glucose often, the insulin dose may need to be changed at each meal. The goal is to predict and prevent high blood glucose.
How Much Insulin Should I Take : Bolus
The amount of insulin needed for the bolus depends on how many carbs youre going to have. You need to know how many units of insulin will cover a certain amount of carbs. This is called the insulin-to-carb ratio.
For instance, one unit of rapid-acting insulin might cover 10 grams of carbs. Your ratio would then be written as 1:10. Accordingly, if you ate 10 grams of carbs, you would need to inject 1 unit of insulin.
The insulin-to-carb ratio varies for each person speak to your healthcare team to get help with figuring out your ratio.
Your ratio will often be established through trial-and-error. However, a standard formula for the ratio is the 500 rule.
This is where 500 is divided by your total daily dose. Your total daily dose is the amount of insulin for your bolus and basal doses combined per day .
Thus: 500 ÷ total daily dose = the number of grams of carbs covered by 1 unit of rapid-acting insulin.
If your total daily dose was 50, this would give you the following calculation: 500 ÷ 50 = 10. This would mean that 10 grams of carbs would require 1 unit of insulin, giving you the ratio of 1:10.
Figuring out your bolus also means figuring out your carb intake. Let Hedias carb calculator help you with this. See how it works by getting Hedia from the App Store or from !
Recommended Reading: Prescription Discount Card For Insulin
Tips For Calculating A Total Daily Dose Of Insulin
You can use one of several methods to determine a safe, initial dose
Evidence keeps mounting that high blood sugars lead to worse outcomes in hospitalized patients and that sliding scale regimens produce both more hyperglycemia and hypoglycemia.
Our November/December 2021 article focuses on the use of sliding scale insulin treatment: Sliding scale insulin for inpatients gets some respect. For more stories that focus on glycemic control for diabetic inpatients, .
But as hospitalists switch from sliding scale to basal and bolus dosing, how do they calculate a safe total daily dose to start with? Experts say that physicians can use any of three different strategies, depending on whether patients have been using insulin as either an outpatient or in the ICU.
The pharmacology is never going to work if we dont follow physiology.
~ Deepak Asudani, MD Baystate Medical Center
Any one of these approaches will produce a safe, conservative initial insulin dose, but experts warn that none of the strategies by itself is a slam dunk. You still have to bring art to each approach, adjusting doses according to such factors as illness severity and eating status.
Heres a look at how two hospitalists use these strategies in their day-to-day practice.
1. Base total sub-Q dose on insulin infusion rates.
Update: Standards of medical care in inpatient diabetes care
Related article: Insulin protocol review: the transition from IV to sub-Q
Online dosing resources
Basal Insulin Dose Chart
For this chart, well assume that your premeal blood sugar target is 120 mg/dL and that 1 unit will decrease your blood sugar by 50 points.
If your blood sugar is below 60, do not administer insulin. Instead, you should immediately consume 15 grams of carbohydrates.
If your blood sugar is 300 and above, check your ketones and contact your doctor immediately.
You May Like: Desserts For Type 1 Diabetes
Mysugr Insulin Calculator Get Help With Your Insulin Dose
3/1/2016 by Scott Johnson
The Insulin Calculator helps you calculate the right amount of insulin or carbs for correction or meals. To make the best use of it, it is important to provide the right settings.
It’s time for lunch. Your blood sugar is 165 mg/dl . You have a big slice of pizza, a bag of chips, and a cold Diet Coke waiting for you. How much insulin do you take?
If you wear an insulin pump, youre probably already using an insulin calculator to inject the correct amount of insulin for corrections and meals. Youre welcome to stay and read, but theres not much new information for you here. However, if youre using injections , like most people with diabetes, then stick around. This article should be helpful.
How To Pick An Insulin Pen With Your Doctors Help
So, which option is best for you? Isaacs suggests asking your healthcare team the following questions to determine the best fit:
- What are my insulin delivery options?
- What options will insurance cover?
- Would I benefit from having a dosing calculator to help calculate insulin doses?
- Would I benefit from a pen that helps keep track of all insulin doses?
- Would I benefit from a pen that knows when a previous insulin dose is still working in my system?
Insurance coverage will likely drive your choice, says Bzowyckyj. If you have multiple options, consider dexterity , whether youll need to administer partial doses, and whether you prefer a disposable pen or a reusable pen that has disposable cartridges, he says. Not everyone prefers to use an insulin pen, but those who do find it easier and much more convenient to use than the traditional vial and syringe, he says.
Read Also: Foods For Type 2 Diabetics
Recommended Reading: Diabetes 1 And 2 Difference
Using The Plate Method To Approximate Carb Counting
Theres another way to approximate carb consumption using the Plate Method. The Plate Method is a visual way of ensuring youre eating enough nonstarchy vegetables and protein while monitoring how many higher-carb foods are on your plate. This method also assumes youre using a 9-inch dinner plate. General guidelines state 1 serving of carbs should be about 15 grams of carbohydrate.
With the Plate Method, you divide your plate into:
- Half non-starchy vegetables
- One quarter with lean protein
- One quarter with foods higher in carbs
Calculate Your Total Daily Insulin Dose
Every individual body is different and thus their insulin requirement is distinct YMMV is an acronym stands for “Your Mileage May Varies.” Therefore, you need to do some trial to find out your exact total daily insulin dose requirement.
To begin with, there is a thumb rule formula to roughly estimating your total daily dose of insulin requirement.
TDD = Body weight x 0.25 Body weight x 0.55
For example, If your body weight is 140 pounds, then your total daily insulin dose = 144 x 0.25 = 35 units of insulin.
Recommended Reading: Keto With Type 1 Diabetes