Who Is At Risk For G6pd Deficiency
G6PD deficiency occurs most often in men. It is rare in women.
The disorder affects about 10% of African-American men in the U.S. It is also common in people from the Mediterranean area, Africa, or Asia.
The severity of the disorder varies, depending on the group. In African-Americans, the problem is mild. It mainly affects older red blood cells. In whites, the disorder is often more serious. In this group, young red blood cells are affected.
The Mechanism Of Hemolysis
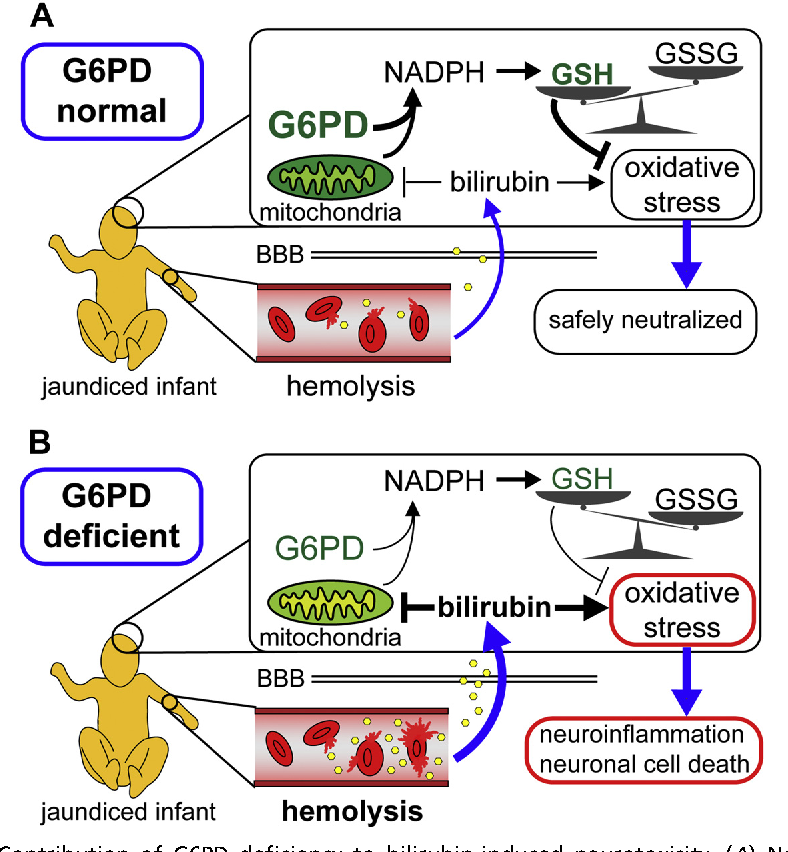
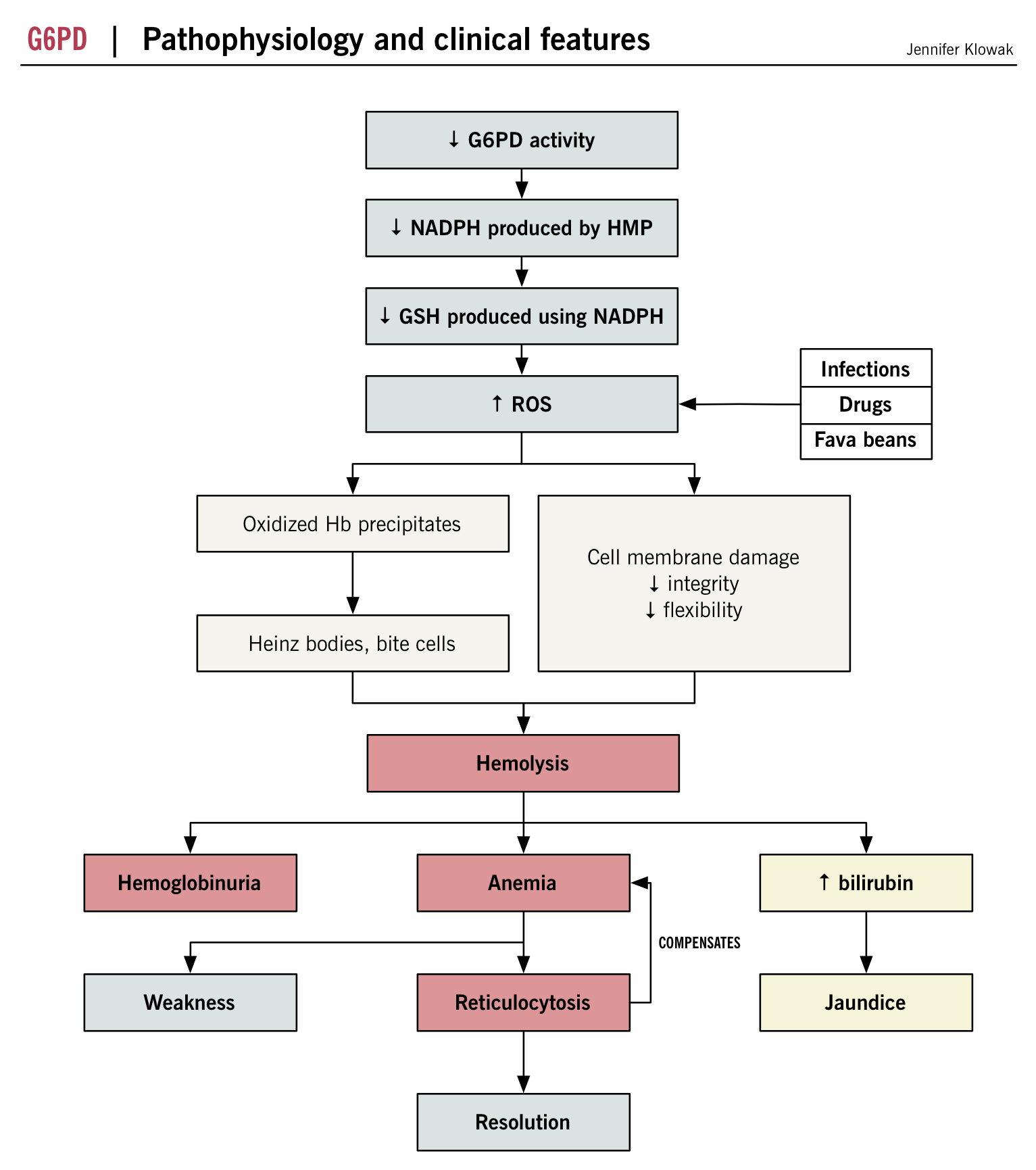
The appearance of Heinz bodies both in vivo and in vitro in G6PD-deficient cells and their inability to protect their GSH against drug challenge suggested that a major component of the hemolytic process was the inability of the erythrocytes to protect sulfhydryl groups against oxidative damage. illustrates a plausible scenario to explain the sequence of events that leads to damage of sulfhydryls in G6PD-deficient red cells. However, it has been shown that in mice, targeted disruption of the gene encoding glutathione peroxidase has little effect on oxidation of hemoglobin of murine cells challenged with peroxides. If the murine model reflects what occurs in man, then different pathways requiring glutathione, such as the thioredoxin reaction, might also be involved.
What Remains To Be Done
Much has been learned about G6PD deficiency and its effects in the past 50 years, but as in every field of science there is still much to learn. Here I can only mention a few of the problems that I consider to be important now.
The development of simple means of testing new drugs in vitro to determine whether they will cause hemolysis in patients has eluded us. Simply incubating drugs with red cells is unreliable, at least in part because it is usually drug metabolites, not the original drug, that are hemolytic. Several different model systems have been proposed, but none have been extensively validated. Perhaps the most attractive of these is the use of plasma from a normal subject ingesting the drug and determining whether it increases metabolism by way of the hexose monophosphate shunt.
Another area of importance is the most devastating result of G6PD deficiency: kernicterus. There has been a resurgence of severe neonatal jaundice and kernicterus in recent years, and G6PD deficiency is one of the causes. Should all newborns be screened? Is the human and the financial cost worth it? Should the screening be limited to ethnic groups who are known to have high gene frequencies, and if so, how will they be identified? Or would it be better simply to monitor bilirubin levels of newborns more closely, thus saving infants from the tragedy of kernicterus, regardless of cause?
Recommended Reading: What Is A1c In Relation To Diabetes
The Population Genetics Of G6pd Deficiency
The prevalence of G6PD deficiency is very high in some parts of the world. Its distribution is largely tropical and paralleled the distribution of malaria, a disease with high morbidity and mortality, and therefore a powerful selective force in human populations. The hypothesis that this infection was responsible for a balanced polymorphism, maintaining a high frequency of G6PD-deficiency mutations as a defense against malaria, was examined in numerous epidemiologic studies in Africa and elsewhere., The most convincing evidence for an effect of G6PD deficiency on malarial infections came from ingenious observations made by Luzzatto et al. Since heterozygous females contained in their circulation a mixture of normal and G6PD-deficient cells, it was possible to examine the percentage of each type of cell parasitized in such individuals, and it was shown that the deficient cells were spared in comparison of the normal ones .
Hows G6pd Deficiency Diagnosed
Your doctor can diagnose G6PD deficiency by performing a simple blood test to check G6PD enzyme levels.
Other diagnostic tests that may be done include a complete blood count, serum hemoglobin test, and a reticulocyte count. All these tests give information about the red blood cells in the body. They can also help your doctor to diagnose hemolytic anemia.
During your appointment, its important to tell your doctor about your diet and any medications youre currently taking. These details can help your doctor with the diagnosis.
Don’t Miss: Benefits Of Bariatric Surgery For Diabetes
Signs And Symptoms Of G6pd Deficiency
Most patients with G6PD deficiency are asymptomatic. Clinical manifestations may include the following:
- Neonatal jaundice
- Episodes of intravascular hemolysis and consequent anemia, triggered by infections, medicines that induce oxidative stresses, fava beans, and ketoacidosis. Hemolysis begins 24 to 72 hours after exposure to oxidant stress. Patients with severe hemolysis present with weakness, tachycardia, jaundice, and hematuria.
- Chronic hemolytic anemia
References
Guide to G6PD deficiency rapid diagnostic testing to support P. vivax radical cure. World Health Organization. Available at . 2018 Accessed: July 19, 2021.
Nkhoma ET, Poole C, Vannappagari V, Hall SA, Beutler E. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. 2009 May-Jun. 42:267-78. .
Beutler E. Glucose-6-phosphate dehydrogenase deficiency: a historical perspective. Blood. 2008 Jan 1. 111:16-24. .
Peters AL, Van Noorden CJ. Glucose-6-phosphate dehydrogenase deficiency and malaria: cytochemical detection of heterozygous G6PD deficiency in women. J Histochem Cytochem. 2009 Nov. 57:1003-11. . .
Beutler E, Westwood B, Prchal JT, Vaca G, Bartsocas CS, Baronciani L. New glucose-6-phosphate dehydrogenase mutations from various ethnic groups. Blood. 1992 Jul 1. 80:255-6. .
Beutler E. G6PD deficiency. Blood. 1994 Dec 1. 84:3613-36. .
The Cloning Of G6pd And Definition Of Mutations
It was possible to show quite rapidly that Yoshida’s deduction that G6PD A was a result of a substitution of aspartic acid for asparagine had been quite correct. Interestingly, it became apparent that G6PD A is not a single variant but a group of variants that had in common the same mutation as G6PD A+, together with one additional mutation, usually c.202 GA .
Read Also: Oral Insulin Pills For Type 1 Diabetes
G6pd Deficiency And Malaria
A close geographic correlation between the frequency of G6PD deficiency and malaria endemicity, reminiscent of what is well known for Hb S, has been observed in very many studies as a result, the coexistence of the 2 abnormalities is not infrequent, and it was natural to wonder whether G6PD deficiency makes sickle cell anemia worse. Overall, the effect is small. When G6PD-deficient red cells are infected by Plasmodium falciparum, they are sensed by macrophages as abnormal at an early stage they are removed, which seems a highly plausible protective mechanism. The original notion that protection is a prerogative of heterozygous females, as in classic balanced polymorphisms, has been confirmed by several recent studies. Perhaps G6PD deficiency protects against cerebral malaria but not against malaria with severe anemia, although this finding has been challenged as possibly due to collider bias. It remains counterintuitive that having only a portion of G6PD-deficient red cells is more protective than having all G6PD-deficient red cells . A convincing mechanistic explanation is still needed.
1960. Based on the close geographic correlation between the frequency of G6PD deficiency and the endemicity of P falciparum malaria, Allison and Motulsky independently suggested that the latter had been a factor in Darwinian selection of the former.
Who Is Affected By G6pd Deficiency
G6PD deficiency affects between 400 and 500 million people across the world. G6PD deficiency is more common among people living in sub-Saharan Africa, the Mediterranean and Southeast Asia regions.
Healthcare providers estimate that 1 in 10 Black men in the United States has G6PD deficiency. Overall, an estimated 4% to 7% of people in the United States have this genetic disorder. About 30% of newborn infants who have severe jaundice have G6PD. Females are less likely than males to have G6PD deficiency.
Also Check: Does Diabetes Affect Your Feet
Genetics And Molecular Genetics
The G6PD gene has 13 exons , and it encodes a polypeptide chain of 514 amino acids, the dimer and the tetramer of which are the enzymatically active forms of G6PD .
There are now 230 G6PD variants with known mutations . All but 2 of them are either missense mutations or small in-frame deletions : these will produce a qualitatively abnormal G6PD protein, which still has some residual enzyme activity. Frame-shift mutations, which would result in zero enzyme activity, are conspicuously absent and the only nonsense mutation , which would do the same, has been found in a heterozygote. These data support the notion that complete loss of G6PD activity is lethal. Some variants have 2 mutations in cis: the best known is G6PD A-, in which a mutation in codon 126 , coexists with 1 of 3 other mutations . It is the combination of the 2 mutations that causes G6PD deficiency. Note: the term variant is currently often used to designate proteins resulting from mutations that may or may not have pathological implications. Algorithms predicting pathogenicity of variants have become popular, but, in the case of G6PD, the finding of enzyme deficiency is the best test because every enzyme-deficient variant has the potential to cause clinical manifestation.
Enhancing Healthcare Team Outcomes
The diagnosis and management of G6PD deficiency are best done with an interprofessional team that includes a geneticist, pediatrician, internist, laboratory professional, pediatric nurses, and a hematologist. In newborns, the treatment focuses on managing jaundice and preventing kernicterus. In older patients, management depends primarily on the overall clinical picture. Less severe presentations may be managed with supportive care and discontinuation and avoidance of the offending agents. Treat any infections as indicated by history and exam. More severe cases may require transfusions.
The primary caregiver, nurse practitioner, and pharmacist must regularly evaluate the patient’s medications to ensure that none is associated with this disorder.
Read Also: How Do You Use A Insulin Pen
Extraerythrocytic Manifestations Of G6pd Deficiency
Because G6PD is ubiquitously expressed, one might expect manifestations of G6PD deficiency not to be limited to red cells, but rather to occur in other cells or tissues as well. Overall, these are not very prominent, mainly because, as stated herein, in most cases the molecular basis of G6PD deficiency is enzyme instability, and presumably nucleated cells can compensate for instability, if need be, through increased G6PD synthesis. The consequence of G6PD deficiency in granulocytes has been best characterized in some of the patients who have CNSHA , who suffered severe bacterial infections. The likely explanation is that granulocytes with severe G6PD deficiency are unable to produce enough NADPH to provide an effective oxidative burst . A possibly related finding is the increased frequency of severe sepsis in G6PD-deficient patients after major trauma : interestingly, this was observed in patients with the common variant G6PD A. There have been isolated case reports in G6PD-deficient persons of acute rhabdomyolysis with myoglobinuria and sometimes acute renal failure. This is a very rare occurrence when compared with AHA, with which it is usually but not always associated.
Correction Of G6pd Deficiency
By transduction of hematopoietic stem cells with a retroviral vector harboring the human G6PD complementary DNA , stable expression of human G6PD was obtained in primary and secondary recipient syngeneic mice. A similar vector was also competent for human G6PD expression in Macaque monkeys. In principle, severe CNSHA due to G6PD deficiency could be treated by allogeneic bone marrow transplantation or by gene therapy, but this has not yet been attempted.
In view of the fact that histone deacetylase inhibitors selectively increase the synthesis of G6PD , butyrate or valproate might correct G6PD deficiency, but chronic administration would be required . Very recently, high-throughput screening has been used to identify a small molecule, AG1 ethyl)ethan-1-amine), which is able to activate G6PD . Although the activation is less than twofold, AG1 might be a lead compound for finding more effective activators.
Read Also: Type 2 Diabetes Age Range
Biochemistry Of G6pd And G6pd Deficiency
G6PD is an enzyme very ancient in evolution, found in all organisms except for Archaea, which are mostly anaerobic, and a few obligate surface parasites and intracellular parasites . G6PD is an oxidoreductase that catalyzes the oxidation of glucose-6-phosphate to 6-phosphoglucono-lactone coupled to the reduction of NAD phosphate to reduced NADP . In all animals, G6PD is ubiquitously expressed, suggesting that it has an essential housekeeping function: indeed, knockout of the G6PD gene is lethal early in embryonic life. G6PD is often referred to as the first enzyme of the pentose phosphate pathway, underscoring its role in the production of pentose sugars required for nucleic acid synthesis . NADPH, produced by G6PD and called its coenzyme, is the electron donor in reactions required for the biosynthesis of deoxyribonucleotides, fatty acids, and steroids it is also the coenzyme of cytochrome P450, central to the metabolism of many drugs and other xenobiotics. The reducing power of NADPH is required in what is commonly referred to as defense against oxidative challenges.
Because mature red cells have no protein synthesis, G6PD activity physiologically decreases as red cells age. Reticulocytes have a high level of G6PD activity, whereas only approximately one-tenth of that remains in the oldest red cells however, in G6PD normal red cells, this amount is still sufficient for their needs.
Key Points About G6pd Deficiency
- G6PD deficiency is the lack of an enzyme in the blood.
- It is a genetic health problem that is most often inherited by men. Women do not usually get it. But they can be carriers and pass it to their children.
- It can cause hemolytic anemia. This is when the red blood cells break down faster than the body can make them.
- It affects about 10% of African-American men in the U.S. It is also common in people from the Mediterranean area, Africa, or Asia.
- Treatment includes avoiding certain medicines, foods, and environmental exposures.
Recommended Reading: What Diet Is Best For Type 1 Diabetes
Symptoms And Signs Of G6pd Deficiency
-
Peripheral smear
-
G6PD assay
The diagnosis is considered in patients with evidence of acute hemolysis, particularly males with a direct antiglobulinânegative hemolytic anemia , red blood cells are removed from the circulation. Hemolysis is defined as premature destruction and hence a shortened RBC life span… read more ). Anemia, jaundice, and reticulocytosis develop during hemolysis.
The peripheral smear may reveal RBCs that appear to have a blister or have one or more “bites” taken from the cell periphery and RBCs with inclusions termed Heinz bodies, which are particles of denatured hemoglobin, which can be recognized only by special stains. These cells may be visible early during the hemolytic episode but do not persist in patients with an intact spleen, which removes them.
Testing for G6PD activity is available. However, during and immediately after a hemolytic episode, tests may yield false-negative results because of destruction of the older, more deficient RBCs and the production of reticulocytes, which are rich in G6PD. Thus, testing may need to be repeated several weeks after the acute event. Several screening tests are available, including point-of-care tests positive results should be confirmed with a quantitative test.
How Do Healthcare Providers Treat G6pd Deficiency
Healthcare providers use different treatments based on your situation. For example, if you have mild jaundice and your doctor knows you have G6PD deficiency, theyll treat your jaundice symptoms and tell you what food or other triggers you need to avoid going forward.
Some people and newborn babies have more severe symptoms. If you have hemolytic anemia, you may need a blood transfusion. If your newborn baby has jaundice, their healthcare provider may treat it with phototherapy . In more serious cases, your babys healthcare provider may recommend whats called an exchange transfusion. In exchange transfusions, their healthcare provider removes your babys unhealthy blood while replacing it with healthy, donated blood.
Read Also: Symptoms Of High Blood Sugar Levels In Type 2 Diabetes
Usmle Step 2 Style Questions Usmle
A 30-year-old male presents to the emergency room with severe, intractable abdominal pain localized to the right upper quadrant area of his abdomen. He reports that he had been having intermittent pain over the past few weeks, but this episode has been unrelenting. An ultrasound reveals numerous . The patient is taken to the operating room for a . After the removal of , its contents were exposed, revealing numerous small, black gallstones. Which of the following is most likely finding on this patient’s medical history?
Glucose-6-phosphate dehydrogenase deficiency, or , is a genetic disorder characterized by decreased levels of glucose-6-phosphate dehydrogenase, which leads to the destruction of red blood cells.
Normally, as a part of the , our produces free radicals like hydrogen peroxide, or H2O2.
Free radicals can damage the cells in many ways including destroying the DNA, proteins, and the .
Now, we have a molecule in our called glutathione which acts as an antioxidant and goes around and neutralizes these free radicals.
In order to function, these molecules need to be in the reduced state where they can donate an electron to the H2O2 and convert them into harmless water and oxygen.
However this causes the glutathione to become oxidized, so before it can get back to work, an enzyme called glutathione reductase will use an NADPH as an electron donor and and reduce the oxidized glutathione back into its working state.
Test Of Heterogeneity Between Studies
The Cochrane Q and I2 statistics were used to assess inconsistency among studies. For Chi2 test of heterogeneity, statistical significance was set as p< 0.10. Fixed-effects model was adopted when there was a lack of significant heterogeneity , otherwise heterogeneity among studies is assumed and random-effects model with weighting of the studies was applied.
Read Also: Best Fruit Drinks For Diabetics
Study Inclusion Criteria And Study Selection
All original studies describing association between G6PD deficiency and malaria were included in this systematic review. All eligible studies irrespective of publication type, study design, language and publication date were considered in the qualitative systematic review. There was no restriction on certain population, age, race, ethnicity, or geographic area. Only variables reported by two or more studies and whose primary data can be extracted were included in the meta-analysis. We limited included studies to those performed on human subjects. Reviews, case studies, case series, editor correspondences, news, letters, book chapters and studies whose data could not be reliably retrieved or extracted were excluded. We omitted studies whose data is overlapped with another included study. Two reviewers independently performed initial screening and study selection. Preliminary assessment of the title and abstracts was performed to identify relevant articles. Thereafter, full texts of eligible articles were downloaded and reviewed for qualitative analysis and potential inclusion in the data synthesis. Inclusion of a study by both reviewers was conclusive while discrepancies and disagreements as regards study eligibility were resolved by discussion and/or consensus with a third reviewer.