New Classification And Criteria For Diagnosis Of Diabetes Mellitus
Peter G Colman*, David W Thomas, Paul Z Zimmet*, Timothy A Welborn*, Peter Garcia-Webb§ and M Peter Moore.
First published in the Medical Journal of Australia . Reprinted with permission.
Introduction
Recently, there has been major growth in knowledge about the aetiology and pathogenesis of different types of diabetes and about the predictive value of different blood glucose levels for development of complications. In response, both the American Diabetes Association and the World Health Organization have re-examined, redefined and updated the classification of and criteria for diabetes, which have been unchanged since 1985. While the two working parties had cross-representation, they met separately, and differences have emerged between their recommendations.
The ADA published its final recommendations in 19971, while the WHO group published its provisional conclusions for consultation and comment in June 19982.
The WHO process called for comments on the proposal by the end of September 1998, with the intention of finalising definitive classification and criteria by the end of December 1998 and of publishing these soon thereafter. However, WHO publications need to go through an internal approval process and it may be up to 12 months before the final WHO document appears.
Key messages
Diagnosis of diabetes is not in doubt when there are classical symptoms of thirst and polyuria and a random venous plasma glucose level 11.1 mmol/L.
What are the new diagnostic criteria?
Screening For Type 1 Diabetes Risk
While widespread clinical screening of asymptomatic low-risk individuals is not currently recommended due to lack of approved therapeutic interventions, several innovative research screening programs are available in Europe and the U.S. . Participation should be encouraged to accelerate development of evidence-based clinical guidelines for the general population and relatives of those with type 1 diabetes. Individuals who test positive should be counseled about the risk of developing diabetes, diabetes symptoms, and DKA prevention. Numerous clinical studies are being conducted to test various methods of preventing and treating stage 2 type 1 diabetes in those with evidence of autoimmunity with promising results . Delay of overt diabetes development in stage 2 type 1 diabetes with the anti-CD3 antibody teplizumab in relatives at risk for type 1 diabetes was reported in 2019, with an extension of the randomized controlled trial in 2021 . Based on these data, this agent has been submitted to the FDA for the indication of delay or prevention of clinical type 1 diabetes in at-risk individuals. Neither this agent nor others in this category are currently available for clinical use.
Pathophysiology Of Type 1 Diabetes Mellitus:
Don’t Miss: How Much Does Aflac Pay For Diabetes
Procedures If Measurement Results Are Close To The Diagnostic Criteria Levels
When using the fasting glucose value, a fasting time of 812 h is essential. The guidelines for performing an oGTT must be followed . Using the HbA1c value for diagnosis is currently not recommended, in particular, because the allowed deviation for external quality control tests is ±18% to date in Germany. This value will be reduced to ±8% in the next years in the Rili-BAEK, then using HbA1c as a diagnostic criterion will improve significantly. The sensitivity of the laboratory tests for diagnosing diabetes is specified below in ascending order in relation to the oGTT, i.e. an oGTT should be performed to rule-out diabetes if the HbA1c values and fasting glucose values lie closely below the diagnostic criteria.
Oral glucose tolerance test .
DDG, Deutsche Diabetes Gesellschaft WHO, World Health Organization KLD, Kommission Labordiagnostik in der Diabetologie AGDT, Arbeitsgemeinschaft Diabetes & Technologie.
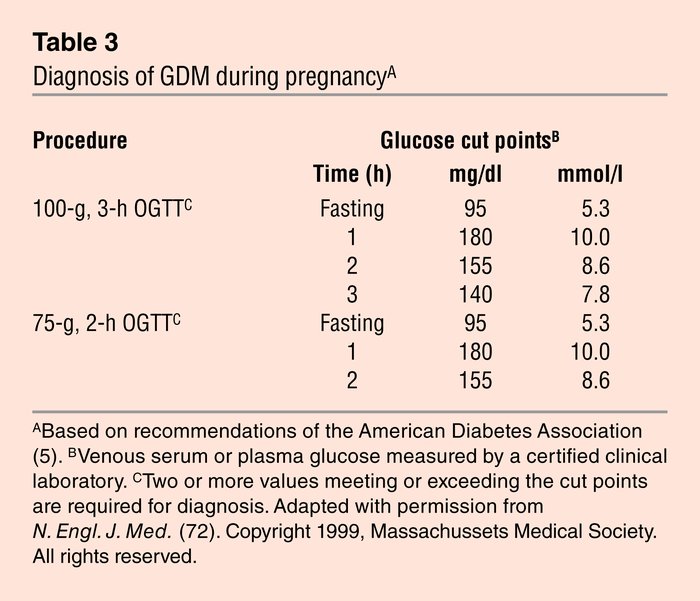
Diagnosis Of Gestational Diabetes
GDM carries risks for the mother and neonate. The Hyperglycemia and Adverse Pregnancy Outcomes study , a large-scale multinational epidemiologic study, demonstrated that risk of adverse maternal, fetal, and neonatal outcomes continuously increased as a function of maternal glycemia at 24-28 weeks, even within ranges previously considered normal for pregnancy. For most complications, there was no threshold for risk. These results have led to careful reconsideration of the diagnostic criteria for GDM. After deliberations in 2008-2009, the IADPSG, an international consensus group with representatives from multiple obstetrical and diabetes organizations, including ADA, developed revised recommendations for diagnosing GDM. The group recommended that all women not known to have diabetes undergo a 75-g OGTT at 24-28 weeks of gestation. Additionally, the group developed diagnostic cutpoints for the fasting, 1-h, and 2-h plasma glucose measurements that conveyed an odds ratio for adverse outcomes of at least 1.75 compared with women with mean glucose levels in the HAPO study. Current screening and diagnostic strategies, based on the IADPSG statement , are outlined in Table 4.
Also Check: What Helps With Insulin Resistance
Hba1c For Diagnosis Purposes
Contributing factors leading to an influence or falsification of the HbA1c value.
|
Hemoglobin variants the extent of the distortion depends on the measurement methods useda,b Conditions with increased or lower life expectancy of erythrocytes a Chemical modifications of hemoglobinb Uremia , high dosed long-term therapy with acetylsalicylic acid b Inhibition of glycolysis . The clinical relevance of this phenomenon has not been investigated adequatelyb Ethnicity and age a |
Who Announces The Latest Criteria For Diagnosis Of Diabetes
| What is Diabetes Causes and Symptoms |
| What is the Latest Diabetes Test Standard? |
Diabetes is a group of metabolic diseases characterized by high blood sugar. Hyperglycemia is caused by defective insulin secretion or impaired biological effects, or both. Long-term hyperglycemia causes chronic damage and dysfunction of various tissues, especially eyes, kidneys, heart, blood vessels, and nerves.
Also Check: How Do You Reverse Type 2 Diabetes
Publication Bias And Risk Of Bias
There was no substantial publication bias for meta-analyses based on the Beggs test . Overall most of studies were judged as having low risk of bias for the evaluated domains details are presented in Additional file : Figures S8, S9 as shown most cross-sectional and casecontrol studies had a low risk of bias in the assessment of exposure, development of outcome of interest in case and controls and selection of cases, approximately one-third of them had a high risk of bias in control of prognostic variables and selection of controls.
In addition, cohort studies had a low risk of bias for selection of exposed and non-exposed cohorts, assessment of exposure, presence of outcome of interest at start of study, outcome assessment, and adequacy of follow up of cohorts however one-third of them had a high risk of bias in controlling prognostic variables and assessment of the presence or absence of prognostic factors and 3% of them had a high risk of bias in presence of outcome of interest at initiation of study.
Gestational Hyperglycaemia And Diabetes
Gestational diabetes is carbohydrate intolerance resulting in hyperglycaemia of variable severity with onset or first recognition during pregnancy. It does not exclude the possibility that the glucose intolerance may antedate pregnancy but has been previously unrecognized. The definition applies irrespective of whether or not insulin is used for treatment or the condition persists after pregnancy.
Women who become pregnant and who are known to have diabetes mellitus which antedates pregnancy do not have gestational diabetes but have “diabetes mellitus and pregnancy” and should be treated accordingly before, during, and after the pregnancy.
In the early part of pregnancy fasting and postprandial glucose concentrations are normally lower than in normal, non-pregnant women. Elevated fasting or postprandial plasma glucose levels at this time in pregnancy may well reflect the presence of diabetes which has antedated pregnancy, but criteria for designating abnormally high glucose concentrations at this time have not yet been established. The occurrence of higher than usual plasma glucose levels at this time in pregnancy mandates careful management and may be an indication for carrying out an OGTT . Nevertheless, normal glucose tolerance in the early part of pregnancy does not itself establish that gestational diabetes may not develop later.
6.1 Diagnosis of gestational diabetes
Don’t Miss: Diagnosis Of Diabetes Random Glucose
What Should I Expect If I Have Been Diagnosed With Diabetes
If you have diabetes, the most important thing you can do is keep your blood glucose level within the target range recommended by your healthcare provider. In general, these targets are:
- Before a meal: between 80 and 130 mg/dL.
- About two hours after the start of a meal: less than 180 mg/dL.
You will need to closely follow a treatment plan, which will likely include following a customized diet plan, exercising 30 minutes five times a week, quitting smoking, limiting alcohol and getting seven to nine hours of sleep a night. Always take your medications and insulin as instructed by your provider.
Other Specific Types Of Diabetes
Genetic defects of the -cell.
Several forms of diabetes are associated with monogenetic defects in -cell function. These forms of diabetes are frequently characterized by onset of hyperglycemia at an early age . They are referred to as maturity-onset diabetes of the young and are characterized by impaired insulin secretion with minimal or no defects in insulin action. They are inherited in an autosomal dominant pattern. Abnormalities at six genetic loci on different chromosomes have been identified to date. The most common form is associated with mutations on chromosome 12 in a hepatic transcription factor referred to as hepatocyte nuclear factor -1. A second form is associated with mutations in the glucokinase gene on chromosome 7p and results in a defective glucokinase molecule. Glucokinase converts glucose to glucose-6-phosphate, the metabolism of which, in turn, stimulates insulin secretion by the -cell. Thus, glucokinase serves as the glucose sensor for the -cell. Because of defects in the glucokinase gene, increased plasma levels of glucose are necessary to elicit normal levels of insulin secretion. The less common forms result from mutations in other transcription factors, including HNF-4, HNF-1, insulin promoter factor -1, and NeuroD1.
Genetic defects in insulin action.
Diseases of the exocrine pancreas.
Endocrinopathies.
Drug- or chemical-induced diabetes.
Also Check: Fasting Glucose Test In Pregnancy
New Diagnostic Criteria For Diabetes Mellitus
The new diagnostic criteria for diabetes mellitus have been greatly simplified .2
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
The oral glucose tolerance test previously recommended by the National Diabetes Data Group has been replaced with the recommendation that the diagnosis of diabetes mellitus be based on two fasting plasma glucose levels of 126 mg per dL or higher. Other options for diagnosis include two two-hour postprandial plasma glucose readings of 200 mg per dL or higher after a glucose load of 75 g or two casual glucose readings of 200 mg per dL or higher. Measurement of the fasting plasma glucose level is the preferred diagnostic test, but any combination of two abnormal test results can be used. Fasting plasma glucose was selected as the primary diagnostic test because it predicts adverse outcomes as well as the 2hrPPG test but is much more reproducible than the oral glucose tolerance test or the 2hrPPG test and easier to perform in a clinical setting.
How Often Do I Need To See My Primary Diabetes Healthcare Professional
In general, if you are being treated with insulin shots, you should see your doctor at least every three to four months. If you are treated with pills or are managing diabetes through diet, you should be seen at least every four to six months. More frequent visits may be needed if your blood sugar isn’t managed or if complications of diabetes are worsening.
Also Check: Healthy Diet For Diabetics To Lose Weight
S And Criteria For Diagnosing Diabetes
What Types Of Diabetes Require Insulin
People with Type 1 diabetes need insulin to live. If you have Type 1 diabetes, your body has attacked your pancreas, destroying the cells that make insulin. If you have Type 2 diabetes, your pancreas makes insulin, but it doesnt work as it should. In some people with Type 2 diabetes, insulin may be needed to help glucose move from your bloodstream to your bodys cells where its needed for energy. You may or may not need insulin if you have gestational diabetes. If you are pregnant or have Type 2 diabetes, your healthcare provider will check your blood glucose level, assess other risk factors and determine a treatment approach which may include a combination of lifestyle changes, oral medications and insulin. Each person is unique and so is your treatment plan.
Read Also: What Is The Best Insulin Pump For Type 1 Diabetes
What Is Hyperglycemic Hyperosmolar Nonketotic Syndrome
Hyperglycemic hyperosmolar nonketotic syndrome develops more slowly than diabetes-related ketoacidosis. It occurs in patients with Type 2 diabetes, especially the elderly and usually occurs when patients are ill or stressed. If you have HHNS, you blood glucose level is typically greater than 600 mg/dL. Symptoms include frequent urination, drowsiness, lack of energy and dehydration. HHNS is not associated with ketones in the blood. It can cause coma or death. Youll need to be treated in the hospital.
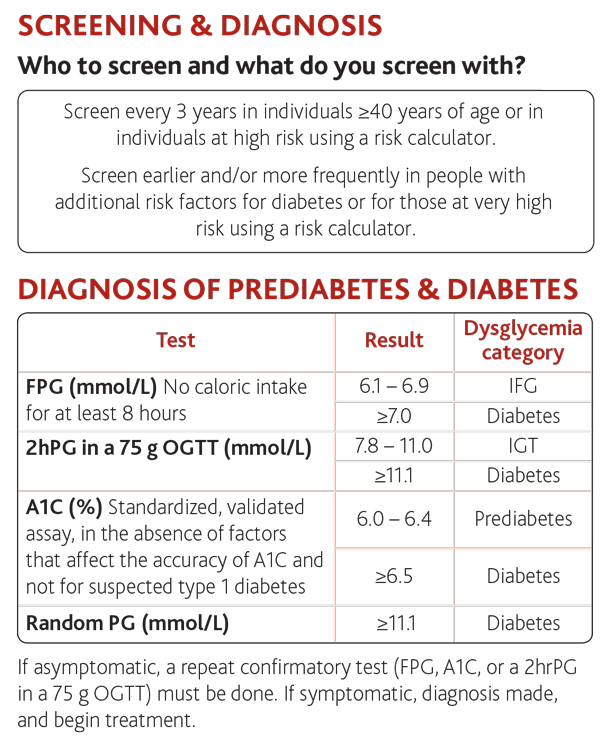
Diagnostic Criteria And Testing
The 1997 ADA consensus guidelines lowered the blood glucose thresholds for the diagnosis of diabetes.5 This increased the number of patients diagnosed at an earlier stage, although no studies have demonstrated a reduction in long-term complications. Data suggest that as many as 5.7 million persons in the United States have undiagnosed diabetes.6Table 1 compares specific diagnostic tests for diabetes.1114
| Test |
|---|
|
Diabetes can also be diagnosed with a random blood glucose level of 200 mg per dL or greater if classic symptoms of diabetes are present. Lower random blood glucose values have a fairly high specificity of 92 to 98 percent therefore, patients with these values should undergo more definitive testing. A low sensitivity of 39 to 55 percent limits the use of random blood glucose testing.15
The oral glucose tolerance test is considered a first-line diagnostic test. Limitations include poor reproducibility and patient compliance because an eight-hour fast is needed before the 75-g glucose load, which is followed two hours later by a blood draw.17 The criterion for diabetes is a serum blood glucose level of greater than 199 mg per dL .
You May Like: Fasting Blood Glucose Normal Range
How Does Diabetes Lead To Amputation
Unmanaged diabetes can lead to poor blood flow . Without oxygen and nutrients , you are more prone to the development of cuts and sores that can lead to infections that cant fully heal. Areas of your body that are farthest away from your heart are more likely to experience the effects of poor blood flow. So areas of your body like your toes, feet, legs and fingers are more likely to be amputated if an infection develops and healing is poor.
Type 2 Diabetes Ada Diagnosis Criteria
Diagnostic criteria by the American Diabetes Association include the following:
-
A fasting plasma glucose level of 126 mg/dL or higher, or
-
A 2-hour plasma glucose level of 200 mg/dL or higher during a 75-g oral glucose tolerance test , or
-
A random plasma glucose of 200 mg/dL or higher in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, or
-
A hemoglobin A1c level of 6.5% or higher
Read Also: How Much Sugar Can A Diabetic Have In One Day
Selection Criteria Study Selection And Data Extraction
Studies were eligible if they had population based design, universally assessed the prevalence of GDM and provided accurate screening strategies and thresholds of blood sugar in those screening test. We excluded non-original studies including reviews, commentaries, editorials, letters, meeting abstracts, case reports or any papers that did not provide accurate and clear data.
The screening of titles, abstracts and full-text articles was conducted independently by authors , for determining final eligibility criteria. Disagreements were resolved through discussions with senior investigator . The general characteristics of the studies including the first author name, journal, publication year, country of study, years of sampling, study design, sample size, population characteristics including age and BMI, PCOS definition, GDM screening strategy, GDM criteria and laboratory values of blood sugar tests, study quality assessment and prevalence of GDM were extracted from the studies included and assessed. To prevent extraction and data entry errors, a control check between the final data used in the meta-analysis and the original publications was performed by all authors.
World Health Organisation Recommendations
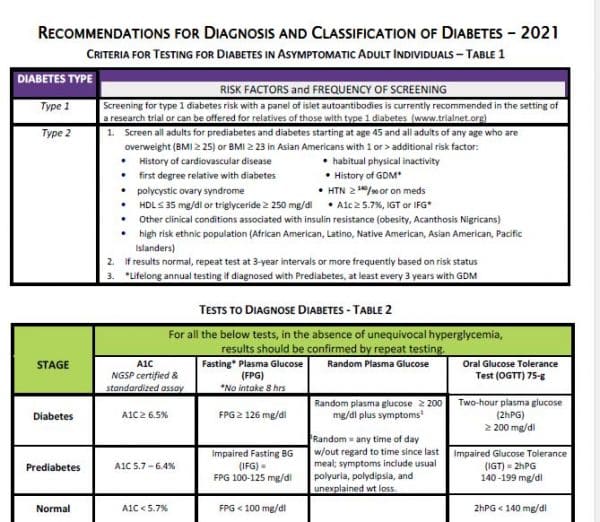
Diabetes UK supports the diagnostic criteria published by the WHO in 2006: “definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia“. Diabetes UK also welcomes the 2011 decision by the WHO to accept the use of HbA1c testing in diagnosing diabetes: “use of glycated haemoglobin in the diagnosis of diabetes mellitus“.
Information on the diagnostic criteria for diabetes is below. For further information and an explanation of terms and classifications please refer to the full WHO guidelines.
Recommended Reading: Blood Sugar Monitor Without Finger Pricks Price