A Program For The Cure Of Type 1 Diabetes Using A Generic Drug: Phase Ii
Researcher:Denise L. Faustman, MD, PhD., Associate ProfessorHarvard Medical School and Director Immunobiology LaboratoryMassachusetts General HospitalCharlestown, MA
Purpose:In August 2012, results of the Phase I trial showed that the pancreas of long-term diabetics was able to transiently make insulin after two doses of the Bacillus Camlette-Guerin vaccine. In 2018 a follow up report on a total of 232 participants both treated and untreated with BCG, published in the journal Vaccines, showed positive results in lowering blood sugars in subjects with type 1 diabetes to almost normal levels while also reducing the amount of insulin needed about one-third after 5 to 8 years from the initial treatment with the BCG vaccine without any reports of severe hypoglycemia. The 2015 FDA approved Phase II clinical trial, which is now fully enrolled with 150 participants with long-term type 1 diabetes, will determine the dose and frequency of doses required to reverse type 1 diabetes. It is still necessary to obtain funding to track these patients for an additional two years with the ultimate goal of bringing BCG to market as an approved treatment for type 1 diabetes. Five additional clinic trials with BCG/placebo to over 150 subjects are currently ongoing.
Albert Einstein College of MedicineBronx, NY
Identification Of Environmental Chemicals That Trigger Beta Cell Damage And Type 1 Diabetes
Researcher:Albert Einstein College of MedicineBronx, NY
Purpose:The rise in the incidence of type 1 diabetes , especially in industrialized countries, can only be explained by a prevailing influence of environmental factors interacting with common genetic variants that predispose to T1D. Preliminary epidemiological data support an association between chemical exposure and T1D and there is evidence that such exposures can impact Beta-cell function and contribute to the development of autoimmunity. Despite these correlations, there are no studies directed towards understanding the role of industrial chemical exposure in T1D development. This leaves a gap in our understanding of the T1D etiology and its increasing incidence. Dr. Stefan-Lifshitz has developed a strategy which integrates complementary approaches to efficiently evaluate the association of environmental chemicals and chemical mixtures with T1D development and to dissect the mechanisms by which they trigger T1D in susceptible individuals. These studies will set the rationale for development of prevention strategies based on the mechanisms causing the disease.
Type 2 Diabetes Treatment Options
Managing diabetes involves a combination of medical treatment and lifestyle changes.
Healthy EatingYour care team may include a dietitian who can work with you to make sure you are eating a healthy diet. This may include eating more fresh fruits and vegetables, whole grains, and other high-fiber, nutritious foods cutting out sugary drinks, processed foods, sweets, and refined carbs and replacing saturated fats with healthy fats like olive oil. Its also important to eat regular meals and snacks to keep blood sugar levels stable. You may also need to eat smaller portion sizes and fewer calories to maintain a healthy weight.
Physical ActivityExercise is an integral part of treating type 2 diabetes because physical activity can help regulate blood sugar levels. At the same time, spending long periods sitting down can make your diabetes worse, so its essential to move around. Aim for about 30 minutes of cardiovascular activity like walking, running, dancing, or cycling most days of the week, plus two or three sessions of strength training or other resistance exercises like weight lifting.
Talk with your doctor before starting an exercise program to ensure its safe for your health conditions.
Its important to lose weight at a healthy pace, so work with your healthcare team to develop a weight loss plan.
Your doctor may also prescribe medications to help manage other health conditions related to diabetes, such as hypertension and cardiovascular disease.
Read Also: Does High Blood Sugar Mean You Are Diabetic
Type 2 Diabetes: Experimental Therapy Could Remove Need For Insulin
Scientists have proposed a new therapy for type 2 diabetes. If proven effective, the therapy could help some people discontinue insulin treatment.
Scientists have proposed a new therapy for the treatment of type 2 diabetes, with a proof-of-concept study showing positive initial results. If effective, the therapy may mean that some people can stop taking insulin treatment.
The authors of the research presented their findings at UEG Week Virtual 2020, a conference organized by United European Gastroenterology, a professional nonprofit organization for specialists in digestive health.
National Institute of Diabetes and Digestive and Kidney Diseases , a person may have type 2 diabetes when their blood sugar is too high.
People gain blood sugar, or blood glucose, mainly from the food they eat. Insulin helps cells access this glucose to use as energy. However, for a person with type 2 diabetes, either their body does not make enough insulin or their cells do not respond to insulin correctly.
This then means that the glucose in their blood increases, which can lead to complications of diabetes, such as heart and kidney disease, visual impairment, and loss of sensation in the limbs. The higher the blood glucose over time, the
Centers for Disease Control and Prevention , about 1 in 10 adults in the United States have diabetes, and 9095% of these individuals have type 2 diabetes.
Type 2 Diabetes Treatment
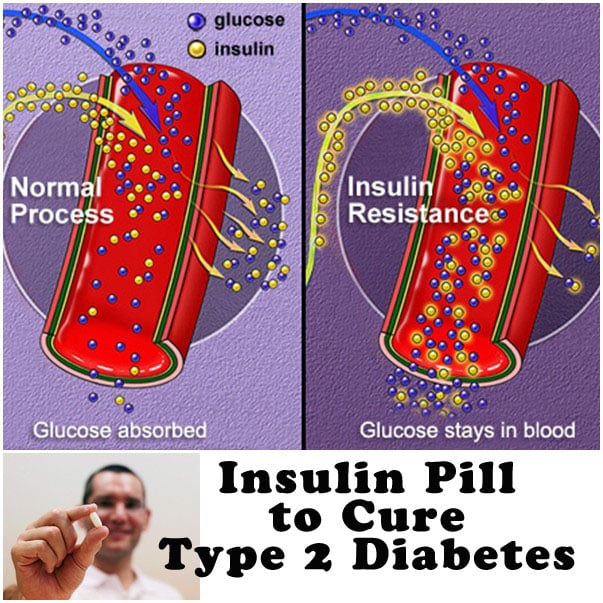
With type 2 diabetes, your body gradually loses the ability to regulate blood sugar levels. Over time, your cells become resistant to insulin. This hormone helps you absorb sugar out of your blood and use it for energy. At the same time, many people stop producing insulin or dont make enough. As a result, sugar, or glucose, starts to accumulate in your bloodstream. This can damage your blood vessels and internal organs if its not managed, leading to severe or even life-threatening complications.
While doctors dont know exactly what causes this disease, having excess weight or living a sedentary lifestyle can increase your risk.
Fortunately, there is treatment for type 2 diabetes. By working with your healthcare provider and making lifestyle changes, you can manage your diabetes and keep blood sugar levels under control, preventing serious health problems.
Read Also: Control Solution For Glucose Meter
Whats Next In Diabetes Treatment
The global diabetes drugs market is expected to reach a massive 68B by 2026, and we can expect all sorts of revolutionary technologies to come forward and claim their market share.
Researchers are already speculating about microchips that can diagnose diabetes type 1 before the symptoms appear, nanorobots traveling in the bloodstream while they measure glucose and deliver insulin, or silica particles that can slow down the digestion of food to prevent diabetes and obesity.
Whatever the future brings, it will undoubtedly make a huge difference in the lives of millions of people worldwide.
Explore Related Topics:
What Are The Problems Associated With Type 2 Diabetes
New advances in research and treatment methods are helping people with type 2 diabetes live full, active and healthy lives. However, it is important to remember that diabetes is a serious, chronic condition with potential short-term and long-term complications. Frequent self-monitoring of blood sugar levels and carefully following an individualized meal and exercise program is a good course of action.
People with undiagnosed, untreated or long-term diabetes are at risk of developing complications, including nerve and blood vessel damage. These potential complications, which can affect the eyes, kidneys, limbs, heart, brain, and stomach, may occur after many years of living with diabetes. Early detection, improved medications, and new technologies may help prevent or minimize diabetes-related complications.
Also Check: Can High Cholesterol Cause Diabetes
New Insights In The Pathogenesis Of Diabetes Mellitus
Researcher:Albert Einstein College of MedicineBronx, NY
Purpose:The main goal of this project is to understand the molecular mechanisms underlying the pathogenesis of diabetes in patients affected by COVID-19. The role of diabetes in COVID-19 is two-fold: not only do people with diabetes present an augmented risk of a severe outcome of COVID-19, but COVID-19 has been shown to also increase the risk of developing diabetes. Dr. Santullis hypothesis is that the coronavirus responsible for COVID-19 is causing endothelial dysfunction and that extracellular vesicles secreted by impaired endothelial cells can cause beta cell dysfunction. Dr. Santullis lab has preliminary data supporting this hypothesis and has identified some specific molecules contained in endothelial microvesicles that can be targeted to prevent and cure the onset of diabetes in COVID-19 patients. Moreover, the unprecedented relationship between endothelial cells and pancreatic beta cells can also be harnessed and targeted in diabetes mellitus non caused by COVID-19.
A New Way To Prevent Immune Cells From Attacking Insulin
Replacing insulin-producing beta-cells that have been lost in people with type 1 diabetes is a promising strategy to restore control of glucose levels. However, because the autoimmune disease is a continuous process, replacing beta-cells results in another immune attack if immunosorbent drugs are not used, which carry significant side-effects. This year, Dr. Song reported on the potential of an immunotherapy he developed that prevents immune cells from attacking beta-cells and reduces inflammatory processes. This immunotherapy offers several potential benefits, including eliminating the need for immunosuppression, long-lasting effects, and the ability to customize the treatment to each patient.
The ability to suppress autoimmunity has implications for both prevention of type 1 diabetes and improving success rates of islet transplantation.
Haque, M., Lei, F., Xiong, X., Das, J. K., Ren, X., Fang, D., Salek-Ardakani, S., Yang, J.-M., & Song, J. . Stem cell-derived tissue-associated regulatory T cells suppress the activity of pathogenic cells in autoimmune diabetes. JCI Insight, 4.
You May Like: Gastric Bypass Surgery And Diabetes
A Better Use Of Rare Donations
Islet cells are created in the pancreas and produce the hormones that regulate blood sugar, such as insulin.
Transplantation of islet cells into the liver can help diabetics to produce their own insulin. But with this method, about 75 per cent of transplanted islet cells, donated from cadavers, are lost in the first 24 hours. This is due to the limited supply of oxygenated blood to the liver.
You have to process three pancreases to get one that will work, so transplanting into the liver is a very inefficient procedure, said Professor Coates.
So the quest around the world has been to come up with alternative sites where the cells might be more likely to survive, and thats what led us to start working here, looking at implanting into the skin.
Sourcing islet cells from the pancreas of deceased donors means there is a finite supply. This places a limit on the number transplants that can be performed and the number of patients who can successfully benefit.
However, by creating an oxygen rich environment outside of the liver to support the survival and functioning of islet cells, the supply of donated cells can be better utilised to provide more transplants to more patients.
The innovative treatment is also less invasive than the liver implantation method, as it can be done under local anaesthetic, is easy to monitor or remove and is significantly less expensive. It also provides the transplanted cells with their own blood supply, which reduces the risk to the patient.
Type 1 Diabetes Research
Through the JDRF Beyond Type 1 Alliance, Beyond Type 1 has partnered with JDRF the worlds biggest nonprofit funder of Type 1 diabetes research to educate our community on the important role research plays in the lives of everyone affected by T1D. It was diabetes research that led to the discovery of insulin in 1921. It was research that led to the creation of the first insulin pump in 1963, and research that led to the modern analog insulins used by many living with T1D today. Without research, we wouldnt have CGMs, hybrid closed loop systems, or treatment for the complications that arise from living with diabetes. And it is research that will some day lead to the cure for Type 1 diabetes.
Don’t Miss: How To Check Accuracy Of Glucose Meter
Can Type 2 Diabetes Be Reversed
Type 2 diabetes can be a life-long, chronic disease in which the body either does not produce enough insulin or the cells in out body doesnt respond to insulin correctly. Because of these two problems, there isnt enough insulin to move the glucose from the blood into the cells. When glucose builds up in the blood instead of going into cells, the bodys cells cant function properly.
Type 2 diabetes is more likely to occur in people who are over the age of 40, overweight, or have a family history in diabetes. Certain ethnic and racial groups also have higher risk for type 2 diabetes, including black, Hispanic/Latino, American Indian, Asian American and Pacific Islander. However, over the past decade the incidence of type2 diabetes has been increasing in adolescents and the young adult population.
According to recent research, type 2 diabetes cannot be cured, but individuals can have glucose levels that return to non-diabetes range, or pre-diabetes glucose level The primary means by which people with type 2 diabetes achieve remission is by losing significant amounts of weight.
We talk of remission and not a cure because it isnt permanent. The beta cells have been damaged and the underlying genetic factors contributing to the persons susceptibility to diabetes remain intact. Over time the disease process reasserts itself and continued destruction of the beta cells ensues. An environmental insult such as weight gain can bring back the symptomatic glucose intolerance.
Preclinical Targeting Of Immune
Researcher:Diabetes, Obesity, and Metabolism Institute Icahn School of Medicine at Mount SinaiNew York, NY
Purpose:Thermogenic fat cells dissipate excess calories as heat and confers protection against obesity and diabetes. Dr. Rajbhandaris work have shown that local crosstalk between cytokine interleukin-10 -producing immune cells and fat cells is a determinant of thermogenesis and systemic energy and glucose balance. Deletion of fat IL-10 signaling protects against obesity and insulin resistance, and elicits fat thermogenesis. To further test the hypothesis that fat-specific IL10 receptor directly senses IL-10 in the fat to limit thermogenesis and insulin sensitivity, this study entails two interrelated aims to examine i) metabolic consequences of fat-specific deletion of IL10 receptor in mice by genetic and pharmacological approach, and ii) mechanisms underlying IL-10 inhibition of fat thermogenic gene program. Dr. Rajbhandari’s lab has identified IL-10 axis as a novel regulator of fat tissue. This study aims to explore preclinical targeting of immune signaling and fat tissue function in the setting of obesity and type 2 diabetes.
You May Like: Blood Sugar 136 After Eating
New Research Breakthrough In Type 1 Diabetes
An article in The New York Times on December 3rd made headlines that are especially important for people living with Type 1 diabetes. It announced that Brian Shelton from Ohio had been cured of Type 1 diabetes. Curing Type 1 requires a renewable source of beta cells that can be produced in the laboratory. Once placed into the body, they need to restore insulin production and automatically regulate blood-glucose levels.
On June 29th, Brian received an infusion of cells, grown from stem cells which were just like the insulin-producing pancreas cells his body lacked. Now his body automatically controls its insulin production and blood sugar levels. He may be the first person to be cured of Type 1 diabetes with a new treatment that leads us all to hope that help may be coming for people with Type 1 diabetes.
This study has not yet been published in a peer-reviewed journal so the results of the trial are not yet known. The findings in this one man need to be replicated in many more people and other questions arise:
- will there be unexpected adverse effects,
- people will need to take immunosuppressants and what effects of this are,
- will the cells last for a lifetime or does the treatment have to be repeated.
Nevertheless, it is an amazing result.
The next step for Melton was to start a company to finance taking this procedure to the market and later when the stage of clinical trials was reached, pharmaceutical company, Vertex acquired Semma for $950 million.
Can Walking Alleviate Diabetes
Studies have shown that walking may be effective for lowering blood glucose levels and improving diabetes management. In a research involving individuals with type 1 diabetes, participants were randomly allocated to either take a 30-minute walk after a meal or have the same meal while remaining sedentary.
Don’t Miss: How To Fix Low Blood Sugar
Weight Loss Through A Highly Restrictive Diet
Researchers found that restrictive diets like low carb diets or 800 calorie diets are amazing for diabetes remission. Studies show that it causes diabetes remission in more than half of those living with T2D, along with obesity. So those who achieve high weight loss like 15 kg may expect almost 90% of chances of remission.
Researchers are unsure why such amazing results occur on weight loss. However, they think it has something to do with the increased accumulation of fats in the liver causing insulin resistance.
Whole Genome Sequencing For Type 1 Diabetes
Using very new genome technologies and cutting edge scientific methods, my team is embarking on a new program with the aim of functionally annotating the gene changes in type 1 diabetes. To start, we have sequenced the entire genomes of 50 individuals with type 1 diabetes.
Already, even at this early stage of this newest program, we have made an exciting discovery. We have shown how single-nucleotide polymorphism changes in one particular gene called A20 not only contributes to diabetes susceptibility, but also enhances rejection in islet transplantation.
This exciting data provides tantalising new information that will help to bring us closer to a better understanding of type 1 diabetes and hopefully, to a cure.
Every day, scientists all around the world are making progress toward a cure for type 1 diabetes. While it is difficult to say how long it will be before a cure is finally realised, we can reflect on how far we have come since the discovery of insulin in the early twentieth century, and look forward to more new and exciting discoveries that will bring us closer to a cure for type 1 diabetes.
Don’t Miss: How To Use Insulin Pump Video