Increasing Insulin Prices Highlight The Prioritization Of Capitalism Over The Health Of Human Beings In The American Healthcare System
Becca Hamberg BA 24
HHS Competencies: Ethics and judgment Social and structural proficiency
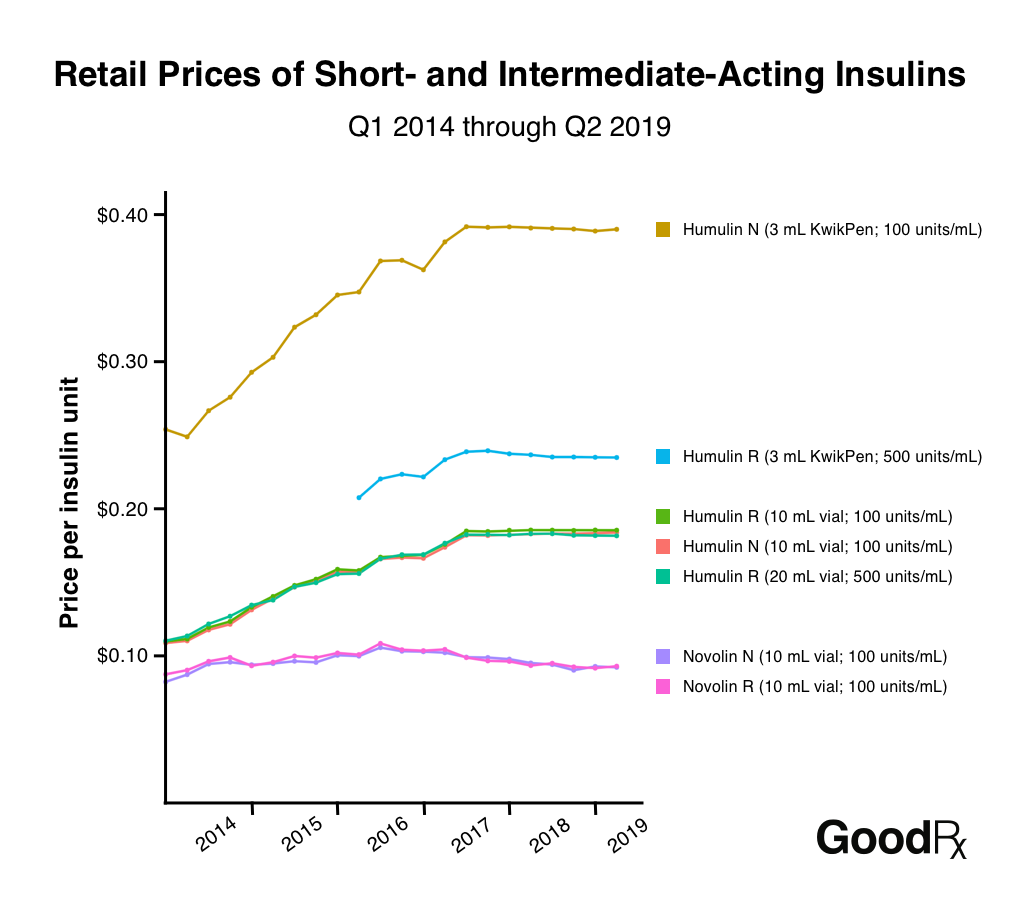
The cost, Im getting it for so cheap its like water, Trump remarked in a September presidential debate falsely claiming that he had significantly reduced the cost of insulin for diabetic Americans . Yet insulin costs between $270 and $289 per vial. Type 1 diabetics typically require two or three vials a month while type 2 diabetics can require 6 or more vials . This means spending between $540 and $1734 or more every month for survival. There are people that are unable to afford these high costs and are forced to figure out a way to stay alive. One strategy is to ration their insulin as a staggering 1 in 4 Americans do or sacrifice other expenses in their life such as buying groceries or paying bills . Rationing insulin can lead to life-threatening and even more costly complications such as kidney failure, blindness, amputation, heart attacks, and in the worst scenarios, death . People with diabetes are forced to make impossible decisions of whether to buy enough to eat or to take their medication. However, this has not always been the case. Insulin prices have increased by 555 percent, adjusted for inflation, in just 14 years .
The Only Thing Thats Changed Is The Price
In 2019, Congress heard testimony from diabetes experts and others regarding the high cost of prescription drugs.
I can help shop for the best price of insulin, connect them with a discount pharmacy, sometimes switch to a less expensive product, said Dr. Kasia J. Lipska, an endocrinologist and assistant professor at Yale School of Medicine. But these are Band-Aid solutions. What we need to do is exert pressure on drug makers to reduce those prices.
Over the past quarter century, the prices of products have increased an average of 75%. Thats a fraction compared to the huge hike for insulin. A vial of Humalog , which cost $21 in 1996, now costs as much as $400 a more than 1,800% increase.
During that time, theres been no innovation to improve Humalog, Lipska said. Its the same exact insulin hormone. The only thing thats changed is the price.
A study she worked on found that 1 in 4 rationed insulin because of the high price.
Executives for the drug makers and the pharmacy benefit managers acknowledged to Congress in 2019 that the cost of insulin had become too expensive.
Kathleen Tregoning, an executive vice president at Sanofi, testified that while the treatment of diabetes has been transformed by medical innovations, the landscape in which patients access medications has also fundamentally changed, and not for the better. We understand the anger of patients who cannot afford the insulin they need due to rising, out-of-pocket costs.
The Role Of Insulin Manufacturers
The list price of insulin has risen steeply over time, with the greatest increase over the last fifteen years. For context, one vial of insulin typically lasts an insulin-dependent person anywhere from 5 to 20 days. Most insulin-dependent people require 2-3 vials of insulin per month, while some require 6 or more. Every case of diabetes is unique.
In the late-90s, one vial of analog insulin cost about $25-40 per vial, without insurance. By 2005, this had doubled to about $80, then started sharply increasing about $125 by 2010, $260 in 2015, and depending on the type of insulin up to $275 and sometimes as much as $500 or more for long-acting analog insulins. Experts have stated that, even in a capitalist but competitive market, an insulin-dependent person should be paying $130 or less per year for their insulin needs.
These price hikes are not limited to insulin all drugs, including all glucose regulating medications and most recently, diabetes devices, are subject to the rebates problem. But insulin is certainly where we see one of the clearest examples of how the US healthcare system is broken. Not only do PBMs and insurance companies benefit, but the Senate Finance Committees January 2020 report states that despite the insulin manufacturers saying that they are not making as much off insulin as people say, evidence shows that they are.
The report calls out several clear instances of the pricing increase practices:
Recommended Reading: Risks Of Type 1 Diabetes
Drugmakers Do This Because They Can
So insulins drug pricing problem is much bigger than anything one state or drug company alone can fix. But more changes in the market may be on the horizon.
The three major insulin makers Eli Lilly, Novo Nordisk, and Sanofi testified before the House Energy and Commerces oversight subcommittee last April, focusing more attention on the issue. Lawmakers, including Sens. Chuck Grassley and Ron Wyden , have also been investigating the problem and sending letters to drug companies asking them to account for their outrageous price hikes.
But while the pressure around insulin may be mounting, were also seeing the terrible impact of rising insulin prices on patients: people being forced to taper off insulin so they can pay their medical bills, and winding up with kidney failure, blindness, or even death.
Some are forced to head to Canada, where drug prices are more heavily regulated and, according to the new NEJM editorial, where a carton of insulin costs $20 instead of the $300 patients often pay in the US. Of course, there isnt enough insulin in all of Canada to make large-scale importation feasible, the editorial authors wrote.
But not all insulins are patent-protected. For example, none of Eli Lillys insulins are, according to the drugmaker. In those cases, Luo said, potential manufacturers may be deterred by secondary patents on non-active ingredients in insulins or on associated devices .
Debate On The Real Impact Of The Proposal
The executive order signed by former President Trump was meant to require federally qualified health centers who purchase insulins and epinephrine in the 340B program to pass the savings from discounted drug prices directly on to medically underserved patients.
The statement made by the US Health and Human Services about the rule said that the proposal would increase access to life-saving insulin and epinephrine for the patients who face especially high costs among the 28 million patients who visit every year.
The rule was finalized in December of last year. However, upon publishing it, the HHS itself acknowledged that the rules economic impact will most likely be minimal since the majority of patients who get their insulin from community health centers already purchase the medication on a discounted price.
The health centers involved also said the same thing. They stated that they already pass on those savings and they even called the rule an administrative burden that paints them as predators and enemies that price-gouge patients.
Read Also: Best Hydration Drink For Diabetics
Senators Press Insurers For Reams Of Pricing And Rebate Info On Insulin
The FDAs policy decrees that any insulin application thats still pending before the agency on March 20, 2020, will be rejected. Any applicant would then have to start over and reapply under a new biosimilar pathway.
Given the lengthy timeline for drug development along with an uncertain and often timely FDA approval process the hard stop in 2020 has made it dicey for drug makers to submit a potential generic insulin application for several years now.
Even companies who have insulin products in development and are ready to file their applications with the FDA are now waiting to apply until after 2020, given they want to avoid going through the time and money of applying in 2019, only to be rejected on the March 20, 2020, date, AAM explained to the FDA in March 2016.
he policy is already having a devastating effect on current development programs for many important protein products, including insulins, AAM wrote in its most recent letter to the FDA on the subject, adding that the policy conflicts with the relevant statutes, is arbitrary and capricious, words often used by companies to signal they will sue over a policy.
When it was first proposed, generic drug makers blasted the 2020 cliff, saying it would impair patient access to affordable alternatives to insulin and other drugs.
Policy Recommendations To Bring Down Insulin Prices
Reed and DeGette in the report recommended 11 policy proposals to address the rising cost of insulin:
- Allow generic drugmakers to manufacturer older, off-patent versions of insulin
- Cap out-of-pocket costs for prescription drugs designed to treat chronic conditions
- Encourage the development of generic insulin products by addressing extensions on patents
- Link a patient’s out-of-pocket costs to negotiated prices instead of list prices
- Promote the development and use of value-based contracts between insulin makers and PBMs
- Promote the use of standardized fees and other payment arrangements instead of rebates between insulin makers and wholesalers
- Restrict the number of changes an insurer can make to a formulary each year
- Require insulin makers, PBMs, and health insurers disclose the value of rebates to other entities in the insulin supply chain
- Require manufacturers disclose how they determine the list price of insulin products
- Standardize the process for patients to challenge formulary restrictions and
- Standardize a process for drug formularies to disclose patient cost-sharing information .
Don’t Miss: Pre Diabetic Diet To Lose Weight
Rep Degette Newly Atop An Oversight Subcommittee Promises To Grill Drug Industry Ceos And Investigate Insulin Makers
While even the American Medical Association acknowledged in a recent policy statement that guidance and educational materials can help younger physicians become more comfortable with prescribing more affordable insulin alternatives, some doctors maintain that they shouldnt be blamed for the current insulin affordability crisis.
When we first starting using Humalog and Lantus, the difference between the two in terms of cost were minimal, but there were modest differences in hypoglycemia, Dr. Irl Hirsch, a professor of medicine at the University of Washington, told STAT. Since cost wasnt a big concern, how can one blame the physicians?
Branded drug makers deserve a share of the blame for the concentrated market, too.
Their strategy for keeping generic competition at bay? Filing patents lots of them. Each of the major manufacturers has hundreds of unexpired patents related to their products, the devices that deliver the drugs, and the methods for manufacturing them.
Sanofi, which manufactures Lantus, has been singled out in particular for allegedly repeatedly making small changes to its product to file for new patents. It has filed 74 patents on some version of that drug alone, according to I-MAK.
What Is A Fqhc / Community Health Center
Federally Qualified Health Centers, or FQHCs, are care clinics that qualify for specific reimbursement systems under Medicare and Medicaid and receive federal Health Center Program grant money intended to finance care for uninsured populations. Their patients are disproportionately poor, uninsured, and minorities. They receive subsidies in the form of federal grants and enhanced Medicaid reimbursement. They are located in underserved rural communities and central cities, where other providers are unable economically or unwilling to locate.
The National Association of Community Health Centers confirmed that its member health centers already provide deeply discounted drug prices to the low-income families they serve. In a press release, NACHC explained that the regulation, , was based on a fundamental misunderstanding that would have imposed extensive administrative burdens and targeted EpiPens and insulin dispensed by health centers and purchased under the federal 340B drug discount program. The 340B rule would have blocked Community Health Centers from receiving future grant funding unless they provided a complete pass-through of 340B discounts on insulin and epi-pens to low-income patients. Community Health Centers strongly opposed the order, arguing that it would add significant bureaucratic obligations to operations while making a minimal impact on the costs of drugs it already provides to patients.
Read Also: Does Sleeve Gastrectomy Cure Diabetes
How Much Does A Pharmacy Make Per Prescription
In 2016, average per-prescription revenues in the NCPA sample decreased to $55.99, compared with $56.37 per prescription in 2015. Combined with the decrease in gross margin, gross profit dollars per prescription dropped by 1.0%, from $11.99 per prescription in 2015 to $11.87 per prescription in 2016.
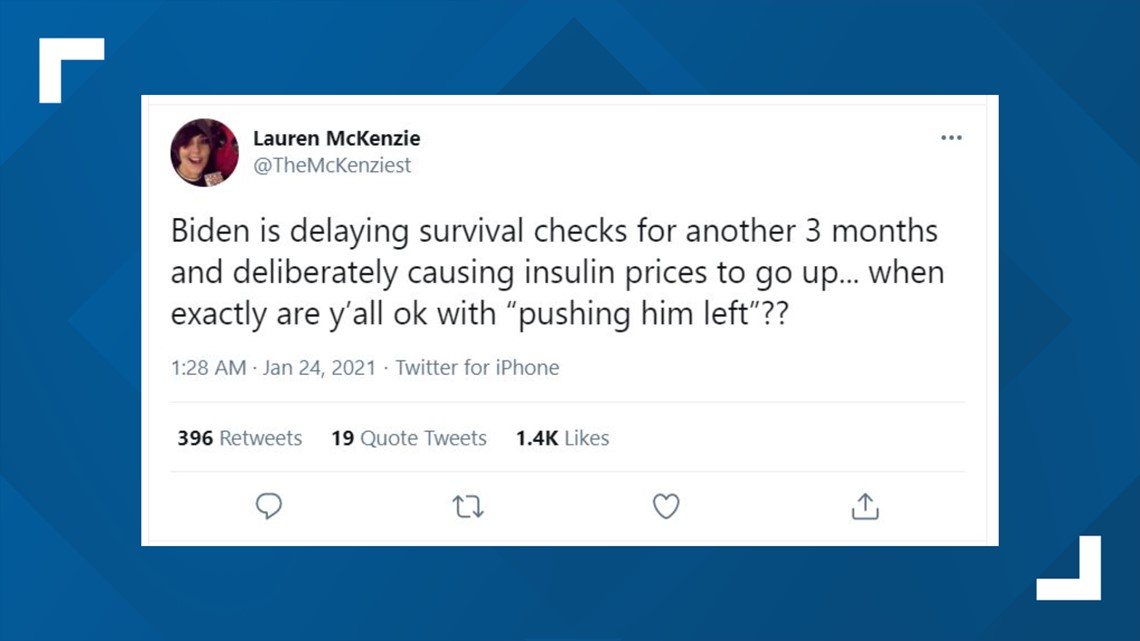
Our Ruling: Missing Context
We rate this claim about the Biden administration’s action to be MISSING CONTEXT, based on our research. Some patients who use insulin and EpiPens the fraction who are served by federally qualified health centers may benefit from Trump’s order, but others could suffer if it results in decreased access for the centers to the 340B drug discount program. Also, the freeze through March 22 does not represent final action on the program, so it’s premature to call it a “reversal.”
Also Check: Does Medicare Cover Diabetic Testing Supplies
Pharma: Biden Freezes Trumps Lower Cost Insulin And Epinephrine Rule
Posted on 01/22/2021
Big pharma is smiling big right now. The big three insulin producers are Eli Lilly and Company, Novo Nordisk A/S, and Sanofi S.A., in which they dominate more than 90% of the world insulin market by value. After swearing-in, U.S. President Joe Bidens HHS froze the Trump administrations December 2020 drug policy that mandates community health centers to pass on all their insulin and epinephrine discount savings to patients.
The rule was finalized in late December 2020. The drug rule was put in place to benefit patients who have a hard time paying for expensive insulin and allergy medication. Former President Trump campaigned on lowering the price of important pharmaceutical drugs like insulin, which is used to treat diabetes, and epinephrine. Diabetes afflicts over a quarter of Medicare beneficiaries and drives billions in Medicare spending every year. More than 20 million Americans have diabetes, in which the body fails to properly use sugar from food due to insufficient insulin, a hormone produced in the pancreas.
How The Companies Justify Their Price Increases
With Type 1 diabetes, which affects about 5 percent of people with diabetes in the US, the immune system attacks the insulin-producing cells in the pancreas, leaving the body with little or none of the hormone. In Type 2 diabetes, the pancreas still makes insulin, but the body has grown resistant to its effects. In both cases, patients rely on insulin medication to keep energy from food flowing into their bodies.
The US is a global outlier on money spent on the drug, representing only 15 percent of the global insulin market and generating almost half of the pharmaceutical industrys insulin revenue. According to a recent study in JAMA Internal Medicine, in the 1990s Medicaid paid between $2.36 and $4.43 per unit of insulin by 2014, those prices more than tripled, depending on the formulation.
The doctors and researchers who study insulin say it is yet another example along with EpiPens and of companies raising the cost of their products because of the lax regulatory environment around drug pricing. They are doing it because they can, Jing Luo, a researcher at Brigham and Womens Hospital, told Vox in 2017, and its scary because it happens in all kinds of different drugs and drug classes.
In countries with single-payer health systems, governments exert much more influence over the entire health care process.
The US doesnt do that. Instead, America has long taken a free market approach to pharmaceuticals.
Recommended Reading: Insulin Syringe Needle Sizes Chart
How Rebates Most Of The Cost Of Your Insulin Work
The math is infuriating, but heres the heavily-simplified basics of how rebates work if you made a product for $5 and wanted to sell it, you may set the price at $10, to create a $5 profit. With that $5 profit, you can invest back in your company to create better products, pay yourself whatever you want to do with your $5.
But lets say you want your product to be in more places and available to more people. You might hire a middle person to place your product in new stores across the country, and theyll charge a fee, which is reasonable.
When you begin, their fee is $1. So that you can keep your $5 profit, you raise your price to $11. Still reasonable. But over time, your middle person makes themselves indispensable and knows it. Youre making way more money because of how many products youre able to sell, so youre not about to drop your middle person.
And oh oops you also signed a contract with your middle person to ensure youll always get your product placed in these nation-wide stores, so youre locked in. And part of that contract was an understanding that you wont lower your price, since that would impact your middle-persons profit.
So now, your product costs $50. Its the same product youve never improved it. Your customers are receiving no more value than when the product cost just $10. Over time, you wanted to make more money from it, so your profit is now $10.
Its still $5 to make your product.
The Astronomical Price Of Insulin Hurts American Families
essay
A woman from Minnesota holds up her U.S. bottle of NovoLog insulin and a Canadian box of NovoRapid, which she bought at a pharmacy in Ontario, Canada, June 29, 2019
Drug companies charge more for insulin in the United States than in nearly three dozen other countries RAND researchers examinedand it’s not even close. The average list price for a unit of insulin in Canada was $12. Step across the border into America, and it’s $98.70.
Those differences help explain why insulin has become a symbol of the high cost of American health care. Its prices have shot up in recent years, for reasons that are opaque at best, with those who can least afford it often paying the most. Reining in those prices has become the rare political cause embraced by Democrats and Republicans alike.
This isn’t just some academic question: ‘How do our prices compare with those in other countries?’ said Andrew Mulcahy, a senior policy researcher at RAND who specializes in health care economics and led the study. It’s becoming a very practical question, because there are ideas out there to do something about it, and they can benefit from this kind of analysis.
The U.S. Department of Health and Human Services asked RAND to investigate how American insulin prices compare with those in other parts of the world. Researchers obtained list prices for all types of insulin from 33 countries in Europe, Asia, Australia, and the Americas. Plotted on a graph, the U.S. prices stand alone.
Recommended Reading: What Is A Good Morning Blood Sugar For A Diabetic