Medicaid And Diabetic Supplies
Medicaid typically covers diabetic supplies and medications. You should always check your states specific coverage and eligibility requirements before ordering your diabetes testing supplies. Most states have disease state management programs to help in areas like diabetes supplies, glucose meters, test strips and more.
Whether you have type 1 diabetes, type 2 diabetes, or have gestational diabetes, as long as youre eligible to receive Medicaid, your diabetes supplies and medications may be covered. In some states you may be required to pay a co-pay to receive your diabetes testing supplies. Again, this will vary by state .You should also check with your Medicaid fiscal intermediary to see the specifics regarding the exact Medicaid coverage for your state and region .
Read Also: How Many Levels Of Medicaid Are There
Best Glucose Meters: The Different Types
Currently, there are three main types of glucose meter:
- Basic blood glucose meters
- Continuous glucose monitors
- CGM-Insulin Pump Combos
The most simple glucometers are handheld devices with a digital screen that displays a reading, and these are the devices were mostly focusing on with our guide to the best glucose meters. These readings are gathered from disposable blood sugar test strips treated with specific chemicals that react to glucose. A new test strip is inserted into the glucometer for each new reading.
Standard glucometers are usually battery operated and capable of storing readings, and many can be connected to a computer so that you can download and store your readings to look back on as needed.
Some basic blood glucose meters are designed with a spring-loaded needle that pricks the side of your fingertip to draw a small drop of blood for testing. Others use an external lancing device.
Once blood is drawn, you touch it to the test strip, which will absorb your blood sample and display a reading on the glucometers screen. While response times vary between blood sugar monitors, were usually talking seconds.
Some glucose meters are approved for Alternate Site Testing . That means they give results within 20% of correct values when used on alternative sites such as the palm, forearm or thigh. However, Diabetes Self Management advises that, you should still check alternate site readings on yourself before trusting them too much.
What Can I Do If I Cant Afford My Insulin
The cost of insulin can be a big concern for people with diabetes. Thankfully, there are resources available for people struggling to afford this medication.
If you need a short-term solution or its an emergency, contact your doctor first. Many health care providers have insulin samples that they can provide to beneficiaries. Free clinics are another source of samples in an emergency.
The diabetes community also bands together to help people with an urgent need by donating extra medication. Searching for diabetes pay-it-forward programs can put you in contact with people who may be able to help.
There are a range of options that may be able to reduce your insulin costs over the long-term.
You May Like: Tooth Removal For Diabetic Patient
Is Dexcom Covered By Medicare
Does Medicare cover Dexcom G6?
Yes. The Dexcom G6 Continuous Glucose Monitoring System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or type 2 diabetes and intensively manage their insulin. Dexcom now ships Dexcom G6 to Medicare patients with traditional fee-for-service coverage. For a full description of coverage criteria, .
Medicare Coverage Criteria
Medicare patients with type 1 and type 2 diabetes on intensive insulin therapy may be able to obtain reimbursement if the following Medicare coverage criteria are met:
- The patient has diabetes
- The patient is insulin-treated with three or more daily administrations of insulin or a continuous subcutaneous insulin infusion pump
- The patients insulin treatment regimen requires frequent adjustments based on BGM or CGM testing results
- Within six months prior to ordering the CGM, the patient had an in-person visit with the treating practitioner to evaluate their diabetes control and determine that the above criteria have been met and
- Every six months following the initial prescription of the CGM, the patient has an in-person visit with the treating practitioner to assess adherence to their CGM regimen and diabetes treatment plan.
*To view a list of compatible smart devices, visit dexcom.com/compatibility
I am an existing Medicare customer. How do I get my ongoing Dexcom G6 supplies?
CMS Policy
Does Medicare Cover Dexcom G6

Glucose monitoring technology, including continuous glucose monitoring systems, plays a vital role in protecting the health of individuals who suffer from issues related to blood sugar and insulin production. In the past, individuals who needed to check their blood glucose levels would typically need to obtain a blood sample, often through a prick on the finger, and the sample would then need to be manually inserted into a testing device for analysis. Unfortunately, this method can be time-consuming, and it relies on the user remembering to take measurements at various times throughout the day. This could also mean missing regular testing during the night due to sleep.
Today, however, advanced glucose monitoring using technology like the Dexcom G6 can provide real-time data 24 hours a day for people who need continuous monitoring. Modern monitoring provides important information regarding overall health as it relates to glucose levels, allowing for faster treatment in the event of an emergency. This is vital for patients who are diabetic or for patients who may be at risk for developing health conditions related to fluctuating or uneven blood glucose.
Related articles:
Read Also: What Age Can You Get Type 2 Diabetes
How Do I Get Medicare To Cover A Cgm
For Medicare to cover the cost of FreeStyle Libre, you must:
- Continue to pay your Part B premium
- Have already paid your Part B deductible
- Receive a prescription for the device from a physician who accepts Medicare
- Buy the CGM from a supplier who accepts Medicare
- Cover whatever portion of the costs that Medicare doesnt
You Are About To Leave For A 3rd Party Website
The Continue link below will take you out of the Abbott Laboratories family of websites. Links which will take you out of Abbott Laboratories worldwide websites are not under the control of Abbott Laboratories, and Abbott Laboratories is not responsible for the contents of any such site or any further links from such site. Abbott Laboratories is providing these links to you only as a convenience, and the inclusion of any link does not imply endorsement of the linked site by Abbott Laboratories.
Do you wish to continue and leave this site?
You May Like: How To Deal With Gestational Diabetes
Medicare Coverage Of Cgm
Medicare has provided coverage for CGM systems since 2017, provided they are classified as therapeutic devices, meaning users can use them to make treatment decisions. These include things like changes to exercise regimen, diet or insulin dosage. While thats still the case, The Centers for Medicare & Medicaid Services have recently relaxed Medicares other coverage criteria somewhat. Previously Medicare coverage of CGM devices was limited to patients who met the following requirements:
-
Have a diagnosis of either type 1 or type 2 diabetes
-
Use a traditional blood glucose meter and test blood sugar levels four or more times a day
-
Are treated with insulin injections or insulin pump
- Require frequent adjustments to their insulin regimen
-
Have an in-person visit with a doctor to evaluate glycemic control and whether they meet the above criteria, as well as follow up appointments every 6 months after prescription
So whats changed? No longer are insulin injections the only acceptable form of insulin administration for those who are covered. Now, diabetics who are treated with inhaled insulin will be eligible for coverage. Additionally, the requirement for self-testing up to four or more times a day with a fingerstick test has been removed, so diabetics who test less frequently may also be eligible.
Medicare Eligibility For A Therapeutic Cgm
A therapeutic CGM is a medical device approved by the U.S. Food and Drug Administration as a replacement for home blood sugar monitors. It provides you and your doctor with the medically necessary information to make diabetes treatment decisions, such as changes in diet and your insulin dosage.
To qualify for a therapeutic CGM, you must be undergoing treatment for diabetes and meet certain other criteria.
To be eligible for a therapeutic CGM under Medicare, you must meet the following requirements.
- You are using insulin to treat Type 1 or Type 2 diabetes.
- You need to check your blood sugar four or more times per day.
- You must use an insulin pump or receive three or more insulin injections per day.
- You must make routine, in-person visits to your doctor.
- Your doctor has determined that you meet all Medicare eligibility requirements.
The decision between a therapeutic CGM or a traditional monitor is one you should make after talking to your doctor. A therapeutic CGM may be a better option if you use insulin and frequently change your dosage.
Don’t Miss: How To Check If I Have Diabetes
What Are The Qualifications For Medicare Coverage For Cgms
Under the guidelines established by Medicare, the following statements must apply to you to qualify for coverage for a CGM:
- You have an established diagnosis of diabetes.
- You are currently using a blood glucose monitor.
- Your doctor recommends that you check your blood sugar four or more times every day.
- You use insulin to control diabetes, and your regimen needs to be adjusted regularly.
- You have been seeing the doctor who will prescribe the CGM for at least 6 months.
- Your doctor has taught you how to properly use the device.
For coverage to continue, you will need to see the prescribing doctor for checkups every 6 months. In addition, you must use the receiver to display your glucose readings. You may use the smartphone app in addition to the receiver to review data or send readings to your medical provider however, you cant only use your smartphone. This rule exists because a smartphone is not classified as durable medical equipment.
Also Check: Is Root Canal Covered By Medicare
What Should Providers Do When Contacted By Cms Regarding Their Cgm Device Billing History
With CMS, the HHS OIG, and the DOJ all prioritizing enforcement with regard to Medicare billing for CGM devices, entities that bill Medicare for CGMs need to be prepared for the possibility of an audit or investigation. If contacted by auditors or federal agents, providers, pharmacies, and others should be prepared to:
Identify Relevant Documentation and Initiate an Internal Compliance Audit
Immediately upon learning of an audit or investigation, it is imperative to identify and preserve all relevant documentation. This includes Medicare compliance policies and procedures, patient records, and billing records pertaining to DME and non-DME continuous glucose monitoring devices. An internal compliance audit needs to be conducted at this time as well, as it will be necessary to determine whether auditors or investigators are going to uncover Medicare billing violations.
Establish Clear Lines of Communication and a Chain of Command
All internal personnel should be instructed not to communicate with auditors or agents directly. There should be a clear chain of command, and all communications with federal authorities should be routed through the practices or companys defense counsel.
Read Also: Can You Change Medicare Plans After Open Enrollment
Don’t Miss: Insulin Syringes 31 Gauge 8mm
What About Medicare Coverage For Those Not On Intensive Insulin Therapy
At this time, Medicare coverage is only available to those that meet the criteria above. We feel very strongly that others at risk of hypoglycemia, especially those on sulfonylureas , should also have access to CGM. We will be working on advocacy on this front if youd like to help.
If you have other questions on Abbotts FreeStyle Libre, Dexcoms G5, and Medicare coverage,
Also Check: When Must The Medicare Supplement Buyers Guide Be Presented
Medicaid And Diabetes Health
As an insurer, Medicaid is dedicated to helping people achieve their health goals. Medicaid has many programs that are geared directly toward specific diseases. The programs are specifically designed to help you with your overall treatment plan and health management. A diabetes health program usually contains information and resources regarding medications, diet, and exercise. Please check with your state run Medicaid program to find out whats available to you as a person living with diabetes.
MedicaidSupplies.com understands that diabetes is a very complex and serious disease. We strive to provide people with valuable information and resources to help make living with diabetes that much easier.
Recommended Reading:
You May Like: Are Diabetic Test Strips Universal
How Do I Get My Diabetic Supplies Through Medicare
You may receive diabetes testing supplies in two ways. You can get them through a local pharmacy or supplier , or you can order your supplies to arrive by mail. To find a Medicare supplier, you can visit Medicare.gov/supplier or call 1-800-MEDICARE .
Medicare has a National Mail-Order Program for diabetes testing supplies. Under this program, you can choose a national supplier who works with Medicare to provide diabetes supplies. These suppliers cannot charge you more than the cost of your unmet deductible plus 20% of the supplies costs through Medicare.
Mail-order suppliers who accept Medicare must meet the following standards:
- They must provide the brand your doctor prescribes.
- They cannot try to influence your choice of test strips brand.
- They must make the same products available to those with Medicare as those without it.
Before choosing any supplier to receive your supplies, including test strips, you must ask them if they are enrolled in Medicare and accept assignment. If the supplier is not enrolled, Medicare will not pay its portion, and you will be responsible for paying for the test strips. By accepting assignment, Medicare will pay the supplier directly so you dont have to pay for the test strips and wait for reimbursement.
You need a new prescription for your diabetes testing supplies at least every 12 months to make sure Medicare will still pay its portion.
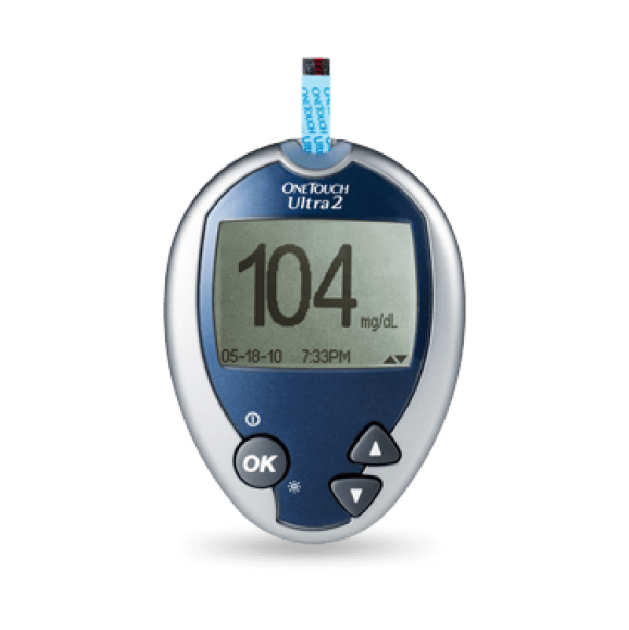
$0 Copays On Preferred Brand Diabetic Test Strips And Glucose Meters For Medicare Advantage Members
In 2018, Independence will continue the requirement for Medicare Advantage members to use diabetic test strips and a glucose meter from the preferred manufacturer brands, Accu-Chek® and OneTouch®, in order to have their test strips and glucose meters covered at $0 copayment. All other manufacturersâ brand of test strips and glucose meters will not be covered by Keystone 65 HMO plans. For Personal Choice 65SM PPO plans, an out-of-network coinsurance will apply to all other manufacturersâ brand of test strips and glucose meters. If their current glucose meter does not work with either of the preferred brands of test strips, Medicare Advantage members can obtain a new glucose meter at no cost. Test strips can be purchased from either a network pharmacy or durable medical equipment supplier. The $0 copayment on Accu-Chek and OneTouch test strips will apply at both preferred and standard pharmacies. Providers may appeal if they feel a member is unable to use Accu-Chek or OneTouch test strips and glucose meters. Note: Independence Medicare Advantage plans will continue to offer a $0 copayment on all brands of lancets and solutions.Continue reading > >
Recommended Reading: Best Fruit Drinks For Diabetics
Medtronics New Access Program Provides Discounted Cgm To Those Without Coverage
Jeemin Kwon
The CGM Discount Access program provides discounted rates on the Guardian Sensor 3 continuous glucose monitoring system for people without insurance coverage for Medtronic CGMs.
Medtronic recently launched its CGM Discount Access program which provides the Guardian Sensor 3 continuous glucose monitor at a discounted price to people who meet the eligibility criteria. Specifically, the program provides a Guardian Link 3 transmitter with a 12-month warranty for $180 and a monthly supply of five Guardian Sensor 3 sensors for $60 per month.
To be eligible for the program, people must:
-
Use multiple daily injections of insulin or be on insulin pump therapy
-
Have a valid CGM prescription from a healthcare professional
-
Not have insurance coverage for a Medtronic CGM
People on Medicare are also eligible for the CGM Discount Access program, as Medicare does not currently cover Medtronics CGM system. It should be noted however, that the Centers for Medicare and Medicaid Services recently proposed new rules that would allow for reimbursement of Medtronics Guardian CGM. If approved, the changes would go into effect on April 1, 2021.
These programs have become increasingly important, especially since people with diabetes face more severe financial hardship during the pandemic. Read more about how COVID-19 has affected the diabetes community here.
Recommended Reading: Does Medicare Pay For Mens Diapers
What Are Continuous Glucose Monitors
Continuous glucose monitors are devices that let you check your blood sugar without having to collect a blood sample each time. To use one, you insert a patch into the skin on the back of your arm. Sensors in the device track your blood sugar levels continuously. When you want to see your number, you hold a receiver up to the patch. Some CGMs have an app that turns your smartphone into a receiver. The app also stores your readings and can send them to your doctor if you wish.
CGMs offer many benefits, including:
- Reduced need for finger sticks
- Greater accuracy, as the devices are not typically affected by over-the-counter medications
- Easier tracking with mobile app
- Fewer low blood glucose emergencies because many devices warn you of out-of-range readings with alarms
Don’t Miss: Just Found Out I Have Diabetes
Resources For People With Diabetes
Diabetes.org: The American Diabetes Association is the online authority on diabetes. If you or a loved one have diabetes, becoming a member is a great idea. The association is devoted to education, prevention, community and meal planning.
Diabetes Forecast: A partner of The Healthy Living Magazine, this resource includes consumer guides on diabetes products and medicines, as well as recipes and tips for taking care of the psychological impacts of living with diabetes.
diaTribe: Excellent resource for finding the latest academic studies on diabetes and clinical trials currently underway, including how you might be able to take part in the trials.
DiabeticGourmet: A website and magazine of diabetic-friendly recipes, diet tips and resources. You can register for free and keep track of your favorite recipes, connect with others on a forum, and receive tips for better management.
Diabetes Food Hub: A partner of the American Diabetes Association, this website is devoted to providing diabetic-friendly recipes and meal planning.
Beyond Type 1: A community of over 2 million people in over 150 countries. This website features programs, stories and news on Type 1 diabetes.
John Hopkins Patient Guide to Diabetes: One of the most comprehensive online resources for diabetes articles, news, terminology, treatments and tools.
Diabetes Exercise News & Organization: A resource for exercise-related articles to help with home-monitoring, recognizing symptoms and managing complications.