What Are The Causes Of Type 1 Diabetes In Children
Glucose comes from food and is the major source of energy for your body. After eating, your body breaks down food into glucose, which is absorbed into the bloodstream. The glucose level rises, triggering the pancreas to produce insulin and release it into the bloodstream. Type 1 diabetes is a result of the pancreas not producing any insulin. This is due to an autoimmune reaction where the body destroys the cells in the pancreas that make insulin. The causes of type 1 diabetes are still being researched. Possible causes include:
- Genes
- Virus or trigger in the environment
Assessment Of Glycemic Control
Recommendations
-
A1C should be measured in all children and adolescents with type 1 diabetes at 3-month intervals to assess their overall glycemic control. E
-
An A1C target of < 7.5% should be considered in children and adolescents with type 1 diabetes but should be individualized based on the needs and situation of the patient and family. E
-
With increasing use of CGM devices, outcomes other than A1C, such as time with glucose in target range and frequency of hypoglycemia, should be considered in the overall assessment of glycemic control. E
Peripheral And Autonomic Neuropathy
The peripheral and autonomic nerves are affected in type 1 diabetes mellitus. Hyperglycemic effects on axons and microvascular changes in endoneural capillaries are amongst the proposed mechanisms.
Autonomic changes involving cardiovascular control have been described in as many as 40% of children with diabetes. Cardiovascular control changes become more likely with increasing duration and worsening control. In a study by 253 patients with type 1 diabetes , Cho et al reported that the prevalence of cardiac autonomic dysfunction increases in association with higher body mass index and central adiposity.
Gastroparesis is another complication, and it which may be caused by autonomic dysfunction. Gastric emptying is significantly delayed, leading to problems of bloating and unpredictable excursions of blood glucose levels.
Also Check: Can You Get Rid Of Diabetes Type 1
Treating Type 1 Diabetes
It’s important that diabetes is diagnosed as early as possible. If left untreated, type-1 diabetes is a life-threatening condition. It’s essential that treatment is started early.
Diabetes can’t be cured, but treatment aims to keep your blood glucose levels as normal as possible and control your symptoms, to prevent health problems developing later in life.
If you’re diagnosed with diabetes, you’ll be referred to a diabetes care team for specialist treatment and monitoring.
As your body can’t produce insulin, you’ll need regular insulin injections to keep your glucose levels normal. You’ll be taught how to do this and how to match the insulin you inject to the food you eat, taking into account your blood glucose level and how much exercise you do.
Insulin injections come in several different forms, with each working slightly differently. You’ll most likely need a combination of different insulin preparations.
Insulin is given to some patients by a continuous infusion of fast acting insulin . This is where a small device constantly pumps insulin into your bloodstream through a plastic tube that’s inserted under the skin with a needle.
There are alternatives to insulin injections and pumps, but they’re only suitable for a small number of patients. They are:
Read more about diagnosing diabetes and treating type 1 diabetes
How Is Type 1 Diabetes Treated
The goal of type 1 diabetes treatment is to control glucose levels and prevent your childs blood sugar from being too high. The ideal diabetes management regimen includes insulin therapy, glucose and ketones monitoring, regular exercise, and healthy eating.
Insulin therapy replaces insulin the body cannot make on its own. Usually, this is done with both long-acting and short-acting insulin injections. Many people with type 1 diabetes use insulin pumps instead of injections. Your diabetes team can teach you more about insulin pumps.
Glucose monitoring It is very important to monitor glucose levels throughout the day. You can do this with finger-stick blood glucose checks and/or with a continuous glucose monitor . CGM devices measure blood sugar with a subcutaneous glucose sensor and report a value every five minutes. Some devices can report values directly to a parent or patients mobile phone. The FDA has approved some CGM devices for use as a replacement for finger-stick tests.
Ketone monitoring When the body doesnt have enough insulin, the liver compensates by producing extra ketones, a chemical that converts fat into energy. High levels of ketones in the blood can become a medical emergency. Therefore, in addition to monitoring glucose levels, it is very important to monitor ketones when your childs glucose level is very high or when your child is sick.
Don’t Miss: Foods Good For Kidney Disease And Diabetes
Maybe It’s A Different Type
If you or someone you know is diagnosed with type 2 diabetes but isnt responding well to the typical treatments for type 2 diabetes, it may be worth a visit to an endocrinologist to determine what type of diabetes is happening. Generally, this requires antibody tests and possibly the measurement of a C-peptide level.
Diabetic Ketoacidosis At Diagnosis Of Type 1 Diabetes Predicts Poor Long
Diabetes Care
Lindsey M. Duca, Bing Wang, Marian Rewers, Arleta Rewers Diabetic Ketoacidosis at Diagnosis of Type 1 Diabetes Predicts Poor Long-term Glycemic Control. Diabetes Care 1 September 2017 40 : 12491255.
This study tested the hypothesis that diabetic ketoacidosis at diagnosis of type 1 diabetes in children predicts poor long-term glycemic control independently of established risk factors.
This was a prospective cohort study of 3,364 Colorado residents diagnosed with type 1 diabetes before 18 years of age, in 19982012, and monitored for up to 15 years. Of those, 1,297 had DKA at diagnosis . Severity of DKA was further classified as mild/moderate or severe . HbA1c levels were measured an average of 2.8 times/year . A linear mixed model was used to examine the effect of DKA on long-term HbA1c levels, adjusting for age, race/ethnicity, sex, family history of diabetes, health insurance, and insulin pump use.
DKA at diagnosis of type 1 diabetes in children predicts poor long-term glycemic control, independent of demographic and socioeconomic factors.
You May Like: Financial Help With Diabetic Supplies
Living With Type 1 Diabetes
You need insulin to live, so youll need to take it every day by injecting it or using an insulin pump. Youll also check your blood sugar levels throughout the day to make sure youre staying in your target range as much as possible. Your health care team will help you understand what your target range is and how to stay within it.
Can Symptoms Appear Suddenly
In people with type 1 diabetes, the onset of symptoms can be very sudden, while in type 2 diabetes, they tend to come about more gradually, and sometimes there are no signs at all.
Symptoms sometimes occur after a viral illness. In some cases, a person may reach the point of diabetic ketoacidosis before a type 1 diagnosis is made. DKA occurs when blood glucose is dangerously high and the body can’t get nutrients into the cells because of the absence of insulin. The body then breaks down muscle and fat for energy, causing an accumulation of ketones in the blood and urine. Symptoms of DKA include a fruity odor on the breath, heavy, taxed breathing and vomiting. If left untreated, DKA can result in stupor, unconsciousness, and even death.
People who have symptomsof type 1 or of DKAshould contact their health care provider immediately for an accurate diagnosis. Keep in mind that these symptoms could signal other problems, too.
Some people with type 1 have a “honeymoon” period, a brief remission of symptoms while the pancreas is still secreting some insulin. The honeymoon phase usually occurs after someone has started taking insulin. A honeymoon can last as little as a week or even up to a year. But its important to know that the absence of symptoms doesn’t mean the diabetes is gone. The pancreas will eventually be unable to secrete insulin, and, if untreated, the symptoms will return.
Recommended Reading: Is Insulin Used To Treat Type 2 Diabetes
Get The Support You Need
Diabetes Canada is here to help provide information and support so that your child can live a healthy life. A positive and realistic attitude toward diabetes can help make it easier.
Talking to other people with kids with type 1 diabetes is a great way to learn, and to feel less alone.
Your health-care team is there to help you too. Depending on the resources available in your community, your team may include a family doctor, diabetes educator , endocrinologist, pharmacist, social worker, exercise physiologist, psychologist, foot-care specialist, and eye-care specialist.
Your team can answer your questions about how to manage diabetes and work with you to adjust food plans, activity and medications.
Complications Of Diabetes In Children
Diabetic ketoacidosis Diabetic Ketoacidosis Diabetic ketoacidosis is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with… read more is common among patients with known type 1 diabetes it develops in about 1 to 10% of patients each year, usually because they have not taken their insulin. Other risk factors for DKA include prior episodes of DKA, difficult social circumstances, depression or other psychiatric disturbances, intercurrent illness, and use of an insulin pump . Clinicians can help minimize the effects of risk factors by providing education, counseling, and support.
You May Like: Printable Low Carb Food List For Diabetics
Glucose And Hba1c Target Levels
Plasma glucose targets or peripheral insulin resistance , causing hyperglycemia. Early symptoms are related to hyperglycemia and include polydipsia… read more ) are established to balance the need to normalize glucose levels with the risk of hypoglycemia. Patients beyond the honeymoon phase should try to have 50% of blood glucose levels in the normal range and < 10% below range.
Treatment goals should be individualized based on patient age, diabetes duration, access to diabetes technology , comorbid conditions, and psychosocial circumstances. The risk of hypoglycemia in children who have hypoglycemia unawareness or lack the maturity to recognize the symptoms of hypoglycemia can limit aggressive attempts to achieve treatment goals. A less stringent HbA1c target level should be considered for such patients, whereas a more stringent target level should be reserved for select patients in whom it can be achieved without significant hypoglycemia and without negative impacts on well-being.
Type 1 Diabetes Insulin Regimens

Insulin is the cornerstone of management of type 1 diabetes. Available insulin formulations are similar to those used in adults . Insulin should be given before a meal, except in young children whose consumption at any given meal is difficult to predict. Dosing requirements vary by age, activity level, pubertal status, and length of time from initial diagnosis. Within a few weeks of initial diagnosis, many patients have a temporary decrease in their insulin requirements because of residual beta-cell function . This honeymoon phase can last from a few months up to 2 years, after which insulin requirements typically range from 0.7 to 1 unit/kg/day. During puberty, patients require higher doses to counteract insulin resistance caused by increased pubertal hormone levels.
Types of insulin regimens include
-
Multiple daily injections regimen
-
Insulin pump therapy
-
Premixed insulin regimen
Most people with type 1 diabetes should be treated with MDI regimens or insulin pump therapy as part of intensive insulin regimens with the goal of improving metabolic control.
Clinicians should use the most intensive management program children and their family can adhere to in order to maximize glycemic control and thus reduce the risk of long-term vascular complications.
Don’t Miss: Nursing Care Plan For Diabetes
Chronic Poor Metabolic Control
A careful multidisciplinary assessment should be undertaken for every child with chronically poor metabolic control to identify potential causative and associated factors, such as depression , eating disorders , lower socioeconomic status, lower family support and higher family conflict , and to identify and address barriers to improved glycemic control. Use of a standardized measure of risk factors has been shown to identify those at high risk for poor control, emergency room visits and DKA . Glycemic control may be particularly challenging during adolescence due to physiologic insulin resistance, depression and other psychological issues, and reduced adherence during a time of growing independence. Multipronged interventions that target emotional, family and coping issues have shown a modest reduction in A1C with reduced rates of hospital admission .
Occurrence In The United States
The overall annual incidence of diabetes mellitus is about 24.3 cases per 100,000 person-years. Although most new diabetes cases are type 1 , increasing numbers of older children are being diagnosed with type 2 diabetes mellitus, especially among minority groups .
A study by Mayer-Davis et al indicated that between 2002 and 2012, the incidence of type 1 and type 2 diabetes mellitus saw a significant rise among youths in the United States. According to the report, after the figures were adjusted for age, sex, and race or ethnic group, the incidence of type 1 and type 2 diabetes mellitus during this period underwent a relative annual increase of 1.8% and 4.8%, respectively. The greatest increases occurred among minority youths.
You May Like: What Do You Do If You Think You Have Diabetes
Screening And Testing For Type 1 Diabetes In Asymptomatic Children
Screening for type 1 diabetes in asymptomatic children with a panel of autoantibodies is currently recommended only in the setting of research studies in first-degree family members of a proband with type 1 diabetes . The incidental discovery of hyperglycemia without classic symptoms does not necessarily indicate new-onset diabetes, especially in young children with an acute illness who may experience stress hyperglycemia. The risk of eventually developing diabetes, however, may be increased in some children with incidental or stress hyperglycemia, especially those with immunological, metabolic, or genetic markers for type 1 diabetes , and consultation with a pediatric endocrinologist is indicated.
Although POC A1C assays may be certified by the NGSP , proficiency testing is not mandated for performing the test accordingly, POC assays for diagnostic purposes are not recommended. Further details on factors that may impact hemoglobin glycation and thus the A1C test, including age, race, and hemoglobinopathies, can be found in Standards of Medical Care in Diabetes .
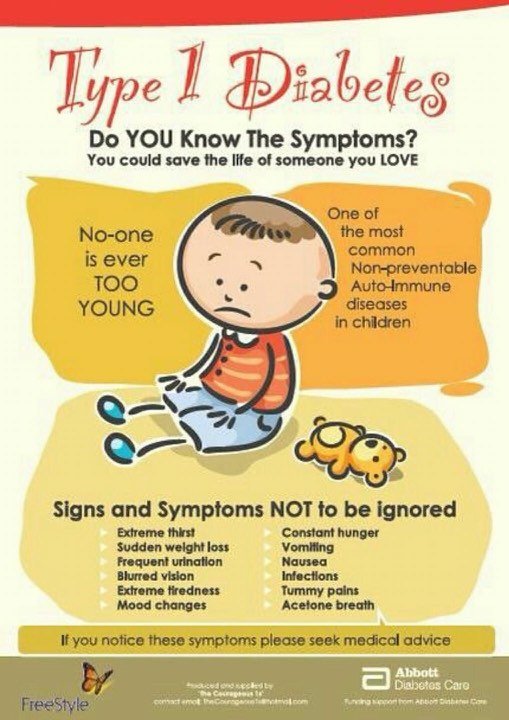
What To Watch For
Symptoms of type 1 diabetes in infants and children can start very suddenly. Keep an eye out for these signs in your baby or child:
- Sudden strange behavior
- Breath that smells fruity, sweet, or like wine
- Extreme drowsiness or lack of energy
- Ongoing, intense thirst
- Peeing more often
- Difficulty breathing
Also Check: Are Omelettes Good For Diabetics
Etiology Of Diabetes In Children And Adolescents
There appears to be a familial component to all types of diabetes in children, although the incidence and mechanism vary.
In type 1 diabetes, the pancreas produces no insulin because of autoimmune destruction of pancreatic beta-cells, possibly triggered by an environmental exposure in genetically susceptible people. Close relatives are at increased risk of diabetes , with overall incidence 4 to 8% . Children with type 1 diabetes are at higher risk of other autoimmune disorders, particularly thyroid disease and celiac disease Celiac Disease Celiac disease is an immunologically mediated disease in genetically susceptible people caused by intolerance to gluten, resulting in mucosal inflammation and villous atrophy, which causes malabsorption… read more . Inherited susceptibility to type 1 diabetes is determined by multiple genes . Susceptibility genes are more common among some populations and explain the higher prevalence of type 1 diabetes in certain ethnic groups .
-
Obesity
-
Native American, black, Hispanic, Asian American, and Pacific Islander heritage
-
Positive family history
Monogenic forms of diabetes are caused by genetic defects that are inherited in an autosomal dominant pattern, so patients typically have one or more affected family members. There is no insulin resistance or autoimmune destruction of beta-cells. Onset is usually before age 25 years.
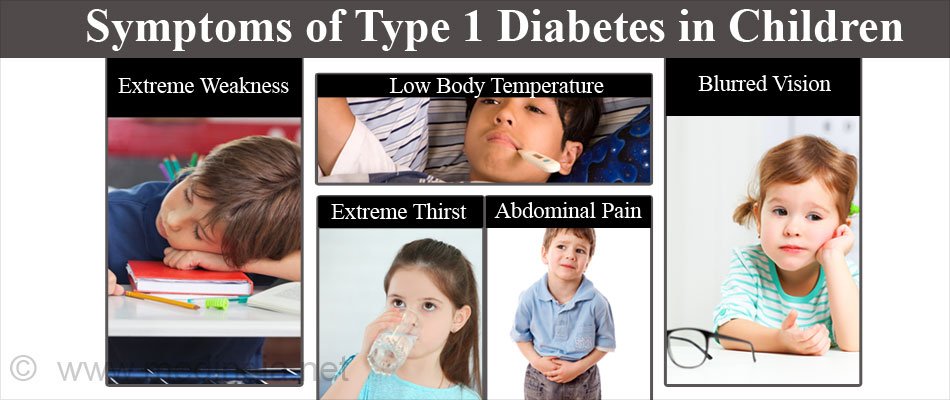
Symptoms Of Type 1 Diabetes In Children
Your childs diabetes symptoms are caused by some or all of the glucose remaining in their blood, rather than being converted into energy by the body. As the body attempts to reduce the levels of glucose in the blood, symptoms can occur.
Lets look at the type 1 diabetes symptoms your child may experience in more detail:
Recommended Reading: Number Of Grams Of Sugar Per Day For Diabetic
Diagnosing Diabetes In Children And Teenagers
Until recently, almost all children and teenagers with diabetes were diagnosed as having type 1 diabetes.
Now younger people are also being diagnosed with type 2 diabetes due to:
- strong family histories
- increasing rates of obesity
- being overweight.
Children or teenagers who have recently been diagnosed with diabetes may struggle with their emotional reactions to their condition and the reactions of others, and have concerns about going back to school.
Teenagers with diabetes may also worry about things like negotiating sex, drinking alcohol, smoking, illicit drugs, driving and work.
Children and families will need a period of adjustment after diabetes is diagnosed.
How Is Type 1 Diabetes Diagnosed
To confirm a diagnosis, your childs doctor may order some or all of the following blood and urine tests:
- hemoglobin A1C test: a blood test that indicates your childs average blood sugar level for the past two to three months
- random blood sugar test: a blood sample taken at a random time
- fasting blood sugar test:a blood sample taken after an overnight fast
- To help distinguish between type 1 and type 2 diabetes, your childs doctor may also check for autoantibodies in the bloodthat are common in type 1 diabetes.
- ketones test: a test that measures ketones, byproducts from the breakdown of fat in children without enough insulin in the urine or blood
Your child may need to have blood drawn more than once so the test results can be confirmed with a second test on a different day. Distinguishing between type 1 and type 2 diabetes in children can sometimes be difficult, and your child’s doctor may need to do additional testing or monitor your child for some time before the type of diabetes can be confirmed.
You May Like: Why Do Diabetics Legs Swell