Neuropathy End Points For Research And Clinical Trials
There are currently no approved disease-modifying therapies for DSPN, CAN, or other forms of diabetic neuropathy, and multiple clinical trials for these conditions have failed. Important contributing factors include a lack of agreement and uniformity in the use of the most sensitive DSPN measures that capture the natural history of the disease and detect repair in the specific nerve fiber populations, as well as the inclusion of appropriate patient populations. Thus, a valid and careful diagnosis for DSPN in clinical research is critical for correctly identifying the appropriate patient population targeted for either a specific intervention or for prognostic implications.
The use of validated clinical instruments such as the Michigan Neuropathy Screening Instrument , the modified Toronto Clinical Neuropathy Scale , the Utah Early Neuropathy Scale , or the Neuropathy Disability Score are recommended. These may be combined with electrophysiology measures of small-fiber damage and repair, such as intraepidermal nerve fiber density or corneal confocal microscopy and objective measures of patient function in the design of DSPN trials.
This position statement was reviewed and approved by the American Diabetes Association Professional Practice Committee in September 2016 and ratified by the American Diabetes Association Board of Directors in October 2016.
Research Ethics And Informed Consent
ADDITION-Denmark was approved by the Committee on Health Research Ethics in the Central Denmark Region and by the Danish Data Protection Agency . The Danish National Committee on Health Research Ethics and the Danish Data Protection Agency approved the DD2 study. All participants in ADDITION-Denmark and DD2 gave written informed consent.
Epidemiology And Impact Of Diabetic Neuropathies
Diabetic neuropathies are the most common complications of T1DM and T2DM. Distal symmetric polyneuropathy represents the most commonly diagnosed and highly morbid of the diabetic neuropathies. While prevalence estimates vary depending on how the diagnosis is made, DSPN occurs in at least half if not more of all diabetic patients over time.595 Prevalence as determined by clinical examination was approximately 45% after 25 years of diabetes in the classic study by Pirat following a cohort of 4400 diabetic patients between 1947 and 1973.596 However, when more contemporary quantitative sensory testing or nerve conduction studies are used as part of the diagnostic criteria, the prevalence of DSPN increases from 60%597 to greater than 75%.598 Multiple studies now confirm that DPSN also occurs inpatients with prediabetes and the metabolic syndrome599601 and while higher in those metabolic syndrome patients with hyperglycemia, ranging from prediabetic to T2DM levels, DSPN can also occur independent of glycemic status.601 With the alarming rise of prediabetes, T2DM, and the metabolic syndrome, estimates range from 15 million to 30 million individuals in the United States are living with DSPN.602
Gerald Charnogursky, … Norma Lopez, in, 2014
Don’t Miss: Keto Pills Safe For Diabetics
Diabetic Neuropathy: A Position Statement By The American Diabetes Association
R.P.-B. and A.J.M.B. served as co-chairs of the writing committee.
Diabetes Care
Rodica Pop-Busui, Andrew J.M. Boulton, Eva L. Feldman, Vera Bril, Roy Freeman, Rayaz A. Malik, Jay M. Sosenko, Dan Ziegler Diabetic Neuropathy: A Position Statement by the American Diabetes Association. Diabetes Care 1 January 2017 40 : 136154.
Medical Management / Interventions
Medical management starts with 0ptimized glycemic control and lifestyle interventions. Lifestyle intervention includes physical exercise and weight loss.
Tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors and anticonvulsants are commonly prescribed treatments for neuropathic pain. At present, there are no universally accepted disease modifying medicines, but this is currently being researched and developed.
Moreover, multidisciplinary team management is required for the prevention and management of diabetic foot complications.
Also Check: What Does Black Seed Oil Do For Diabetics
Precision Medicine For Painful
Unfortunately, the current pharmacotherapeutic agents available for neuropathic pain, including painful-DPN, remain inadequate with the best agents offering only modest improvements in pain which is often offset with significant side effects . Traditional neuropathic pain treatments have been prescribed according to disease etiology. However, the clinical features, and perhaps underlying disease mechanisms, of neuropathic pain may vary greatly from individual to individual . Recent studies have explored whether stratification according to patient characteristics can identify patients more likely to respond to a particular treatment. The ultimate end goal is personalized medicine which is currently only possible in rare cases of neuropathic pain secondary to gene mutations. Over recent years, the stratification methods employed for neuropathic pain treatments include: detailed clinical assessment, sensory profiling, psychology/co-morbidities, physiological changes and molecular profiling .
What Is Diabetic Neuropathy
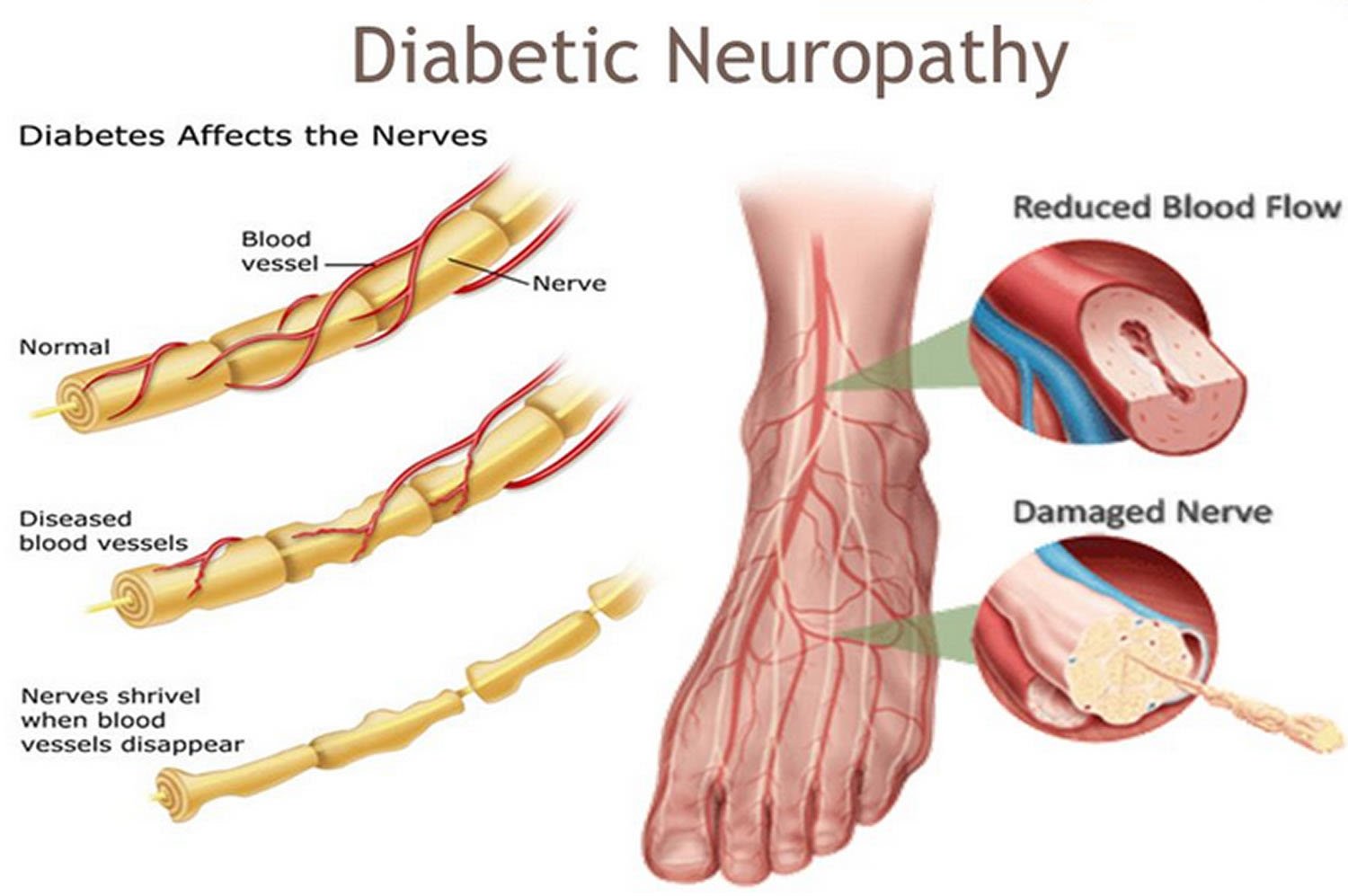
Neuropathy is a complication of diabetes that can lead to problems throughout the body. Diabetes can affect nerves that control movement, sensation and other functions.
If you have diabetes, you can develop nerve problems at any time. Sometimes, neuropathy can be the first sign of diabetes. Significant nerve problems can develop within the first 10 years after a diabetes diagnosis. The risk of developing neuropathy increases the longer you have diabetes. About half of people with diabetes have some form of neuropathy.
Read Also: What Is Good For Diabetic Dry Skin
Clinical Features Of Diabetic Neuropathy
DPN may present with a wide range of clinical symptoms and signs. Some people may be entirely asymptomatic, where a foot ulcer can be the first presentation. However, other patients may experience one or a number of different symptoms such as paresthesia , numbness and neuropathic pain which can range from mildly troublesome to intractable, causing great suffering . These symptoms may be sporadic or constant, and their natural history varies among patients. Sensory symptoms may be present for only a short period of time before they disappear entirely, or they may become chronic. Sensory symptoms and clinical examination signs begin in the toes/distal foot symmetrically. On physical examination, light touch and pin-prick of the distal foot is commonly impaired first, followed by more advanced sensory and motor abnormalities. As the disease progresses, it spreads proximally up the leg before impacting the finger tips and upper limbs. The physical examination for patients with painful-DPN is generally indistinct from those without neuropathic pain. However, some patients may have a pure small fiber neuropathy which results in a loss of small fiber modalities with normal large fiber function . Additionally, a small sub-set of patients have the so called irritable nociceptor phenotype with positive sensory signs such as allodynia and hyperalgesia .
What Is Diabetic Polyneuropathy
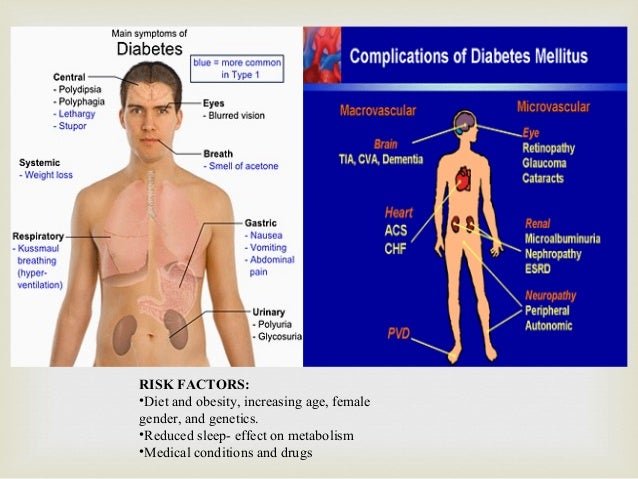
Diabetic polyneuropathy is a complication of diabetes mellitus characterized by progressive death of nerve fibers, which leads to loss of nerves, increased sensitivity, and the development of foot ulcers. Diabetes mellitus is one of the leading non-communicable diseases of mankind. According to the World Health Organization, more than 422 million people suffer from diabetes mellitus worldwide, and 7-10% at the age of 65 and older. Risk factors for development are obesity, low physical activity, hyperlipidemia , arterial hypertension, impaired glucose tolerance, heredity for diabetes mellitus, gestational diabetes in history.
Elevated blood sugar levels cause damage to the peripheral nervous system, which manifests itself in the development of diabetic neuropathy. The initial damage is mainly the long nerve fibers that provide innervation of the distal parts of the lower extremities since they are especially sensitive. This explains the clinical picture of the predominant lesion of the feet.
Also Check: How To Check If I Have Diabetes
Diagnosis Of Diabetes Mellitus
Diagnosis of diabetes mellitus is made on a combination of typical symptomsweight loss, thirst, weakness and fatiguewith a persistently raised blood glucose . Glycosuria and raised HbA1 values alone are not used to make the diagnosis of diabetes mellitus.
Biochemical diagnosis of diabetes mellitus
Treatment Of Diabetic Neuropathy
In diabetic patients the risk of DPN and autonomic neuropathy can be reduced with improved blood glucose control, and the improvement of lipid and blood pressure indexes and the avoidance of cigarette smoking and excess alcohol consumption are already recommended for the prevention of other complications of diabetes .
Also Check: Diabetic Belly Fat Type 1
How Is Diabetic Neuropathy Treated
Theres no cure for diabetic neuropathy, but you can slow its progression. Keeping your blood sugar levels within a healthy range is the best way to decrease the likelihood of developing diabetic neuropathy or slow its progression. It can also relieve some symptoms.
Quitting smoking and exercising regularly are also parts of a comprehensive treatment plan. Always talk to your doctor or healthcare team before beginning a new fitness routine. You may also ask your doctor about complementary treatments or supplements for neuropathy.
Diagnosis Of Autonomic Neuropathy
Questionnaires have been developed to investigate orthostatic symptoms and their severity in dysautonomic conditions, although they have not been specifically validated for CAN and validated translations in different languages are lacking .
Diabetic patients with features of cardiac autonomic dysfunction such as unexplained tachycardia, orthostatic hypotension and poor exercise tolerance, or with other symptoms of autonomic dysfunction, should be evaluated for the presence of CAN. Screening for CAN should be performed at the diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes, particularly in patients at greater risk of CAN due to a history of poor glycaemic control, cardiovascular risk factors, DPN, and macro- and microangiopathic diabetic complications . Diagnosis of CAN is based on the use of cardiovascular autonomic reflex tests for heart rate response to deep breathing, standing and Valsalva manoeuvre, as well as for blood pressure response to standing .
A number of instruments are available to quantify gastrointestinal symptoms, including the Diabetes Bowel Symptom Questionnaire. Objective gastric emptying measurement is advocated for the diagnosis of gastroparesis. Unfortunately, there is no specific test in the detection of diabetic gastroparesis – it is only an exclusion diagnosis after detailed gastrointestinal examinations .
You May Like: Type 2 Diabetes And Heart Failure
Controlling Blood Glucose Levels
Getting blood glucose levels under control cant reverse nerve damage but can prevent further damage from occurring. Your doctor will give you specific blood sugar goals. Managing these levels includes eating a healthy diet high in protein and low in carbs. When you eat carbs, try to choose food with a higher fiber content, avoiding chips and soda.
Regular exercise can help keep blood sugar levels manageable by increasing insulin sensitivity, meaning youll need to take less insulin each day. Getting enough sleep is also important, as we often crave high-carb foods when overly tired.
Symptoms And Clinical Features
The most common symptoms of DSPN are length dependent, usually affecting the feet first and progressing proximally. Symptoms are predominantly sensory and can be classified as positive or negative . Painful DSPN is often described as burning or electric and tends to occur more often at night. Motor symptoms are less common but can occur later in the disease course. Distal deep-tendon reflexes are typically reduced or absent.
The most serious complications of DSPN include foot ulcers, Charcot foot abnormalities, injuries, and ultimately, lower-extremity amputation, especially when concomitant peripheral vascular disease causes foot ischemia. Degradation of sensory function leading to imbalance and unsteadiness in gait with loss of proprioception results in increased likelihood of a fall . Decreased sensation of the distal extremities makes small injuries and ulcers common, and more than 2 % of patients with diabetes develop new foot ulcers each year . The lifetime risk that a patient with diabetes will acquire a foot lesion, including an ulcer or gangrene, is estimated to be approximately 15 % to 25 % . The chronic nature of DSPN can lead to anxiety, depression, catastrophizing behavior, an inability to accept chronic pain, and sleep disturbances .
You May Like: How To Lower Insulin Resistance
Diagnosis Of Sensorimotor Neuropathy
In DPN, sensory deficits usually overshadow motor nerve dysfunction and appear first in the distal portions of the extremities and progress proximally in a stocking-glove’ distribution with increasing duration or severity of diabetes . In the typical form, the large nerve fibres are damaged later than the small ones . The signs and symptoms of DPN vary depending on fibre type involved, with large fibre disease impairing proprioception and light touch. Small-fibre disease impairs pain and temperature perception, leading to paraesthesia, dysaesthesia and/or neuropathic pain . Distal weakness occurs only in the most severe cases. Diminished or absent deep-tendon reflexes, particularly the Achilles tendon reflex, often indicate mild and otherwise asymptomatic DPN. More advanced asymptomatic neuropathy may first present with late complications such as ulceration or neuroarthropathy of the foot .
Electrophysiological tests are usually not recommended in the diagnosis of chronic sensorimotor diabetic neuropathy, as they can be normal when only small-diameter fibres are damaged, but it is a reliable procedure in the case of mononeuropathies or radiculopathies to exclude any other aetiology . Such procedures are really useful when the clinical presentation is atypical and the diabetic origin uncertain .
Diagnostics Of The Diabetic Polyneuropathy
In the diagnosis of diabetic polyneuropathy, its early detection is important. In the future, this will improve the quality of life of patients and prevent early disability. Diagnosis in DPN consists of taking anamnesis, high-quality clinical examination, and the use of modern instrumental examination methods.
Despite the wide possibility and availability of neurophysiological examination methods, special attention is paid to clinical examination. Do not forget that the absence of symptoms does not mean the absence of neuropathy often DPN may be asymptomatic in the early stages. An important role at the preclinical or early clinical stages is played by specific, screening tests that exist to detect early manifestations of diabetic polyneuropathy:
- Study of vibration sensitivity using a graduated tuning fork at 128 Hz, which is applied to the bony part of the distal phalanx of the big toe and the inner ankle.
- Tactile sensitivity studies using monofilament. To perform the test, place the instruments perpendicular to the surface to be examined . When touching the skin, the working monofilament should normally bend, which indicates a reaction. Lack of response indicates decreased sensitivity.
- Using scales to determine polyneuropathy. There are special scales for assessing the strength of the muscles of the feet, the Achilles reflex and pain assessment NISS-LL and for determining the degree of pain, numbness and paresthesia TSS .
You May Like: Can Urgent Care Treat Diabetes
Physiotherapy Management And Exercise
Research has shown that strength training can moderately improve muscle function, reduce neuropathic pain and help control blood sugar levels for people with diabetic neuropathy. Therefore, exercise can help to improve quality of life for this patient group. Diabetic clients must take precautions, including monitoring their blood sugar levels during exercise and snacking beforehand to prevent major fluctuations.
Specific exercise programs should include
- Flexibility .
- Muscle strengthening .
- Aerobic activity.
Endocrine Nutritional And Metabolic Diseasesnote
- transitory endocrine and metabolic disorders specific to newborn
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Includes
- diabetes mellitus due to underlying condition
- drug or chemical induced diabetes mellitus
- secondary diabetes mellitus NEC
- type 1 diabetes mellitus
- Diabetes type 2 with diabetic polyneuropathy
- Diabetes type 2 with peripheral neuropathy
- Diabetic peripheral neuropathy associated with type 2 diabetes mellitus
- Diabetic polyneuropathy
- Polyneuropathy diabetic
- Polyneuropathy , diabetic
- Polyneuropathy associated with type 2 diabetes mellitus
- Polyneuropathy associated with type ii diabetes mellitus
- Polyneuropathy due to type 2 diabetes mellitus
- 008 Simultaneous pancreas and kidney transplant
- 019 Simultaneous pancreas and kidney transplant with hemodialysis
- 073 Cranial and peripheral nerve disorders with mcc
- 074 Cranial and peripheral nerve disorders without mcc
- : New code
- 2017
Also Check: Why Use An Insulin Pump
Focal And Multifocal Neuropathies
This group of neuropathies should not be considered in isolation as they often co-exist with DSDP. Their aetiologies are likely to differ, however, with the focal and multifocal neuropathies having a prominent vascular component or a compressive aetiology as opposed to the predominant metabolic component in DSDP.
> > > Best Diabetes Solution Available
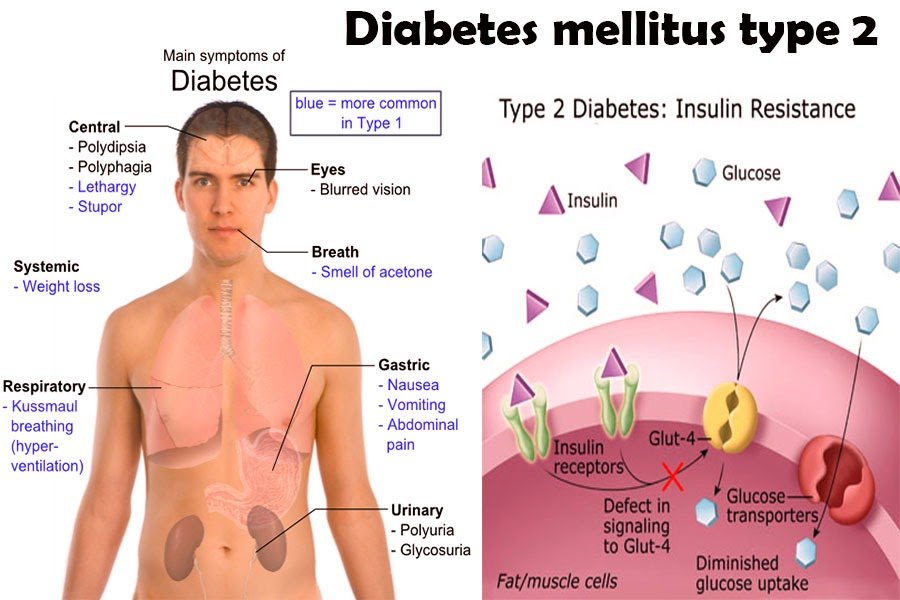
Type 2 diabetes causes the body to become resistant to the hormone insulin. This hormone unlocks cells. There are two types of diabetes: type 1 and type 2. While both types of the disease can cause problems, you can minimize the impact by following healthy eating and being physically active. The sooner you know more about diabetes, the better prepared you will be to deal with it. Once you know more about the disease, youll be better prepared for treatment.
Type 2 diabetes is a chronic condition that causes the body to produce too much insulin. It is also known as type 2 diabetes. If you have type 1, you can control your blood glucose levels by eating a balanced diet. If you have type 2 diabetes, you can even prevent it by adopting healthy lifestyle habits and modifying your diet. Its important to seek information that can help you be your own health advocate. There are many different types of diabetes, so its important to learn as much as you can about the condition.
You May Like: Life Without Diabetes Roy Taylor
Forms Of Diabetic Neuropathy
Several fairly distinct clinical syndromes of diabetic neuropathy have been delineated. The most common, as noted, is a distal, symmetrical, primarily sensory polyneuropathy affecting feet and legs in a chronic, slowly progressive manner. The others are as follows: acute ophthalmoplegia that affects the third, and less often the sixth, cranial nerve on one side acute mononeuropathy of limbs or trunk including a painful thoracolumbar radiculopathy an acute or subacute painful, asymmetrical, predominantly motor multiple neuropathy affecting the upper lumbar roots and the proximal leg muscles a more symmetrical, proximal motor weakness and wasting, usually without pain and with variable sensory loss, pursuing a subacute or chronic course, and an autonomic neuropathy involving bowel, bladder, sweating and circulatory reflexes. These forms of neuropathy often coexist or overlap, particularly the autonomic and distal symmetrical types and the subacute proximal neuropathies .
Table 2
Signs, diagnosis and treatment of diabetic autonomic neuropathies ]
Table 3
The main features of different patterns of disabling neuropathies in patients with diabetes ]