How Can Therapeutic Approaches Be Revised
Even when individuals with conditions or circumstances allowing exemption from specific glycemic targets are removed from discussion, a sizable group of people who have no apparent reason not to attain HbA1c in the 5364 mmol/mol range remains. Insulin therapy is often said to be unlimited in its capacity to lower glucose levels, but in practice, even very high prescribed doses sometimes yield results that fall short of expectations . The underlying causes of failure of usual treatments are undoubtedly numerous, and to understand them calls for further effort to identify the personal characteristics of each person that may prove relevant . In many cases, progressive obesity, as a marker for high calorie intake and insulin resistance, identifies a metabolic challenge that resists success even when ample insulin is delivered to tissues. Other medical conditions may be important. Examples include unrecognized Cushing syndrome or a genetic or acquired disorder of extreme insulin resistance.
For some people, psychological factors may interfere with adherence to the regimen or lead to very poor decisions on the timing and dosage of insulin. Obtaining accurate information about actual use of insulin and other medications, independent of what has been prescribed, can be very challenging. For others, environmental pressures, including financial constraints, family or work-related conflict, or social isolation, may prove to be central factors.
Advise The Use Of Home Glucose Monitoring
People who actively manage their blood glucose can gain better control of their T2D compared with those who do not . The use of self-monitored blood glucose or continuous glucose monitoring can provide valuable information for many patients. The patient and the HCP should discuss patient preference regarding the frequency of testing and recommendations made thereafter. People with T2D need to be aware that the frequency of blood glucose monitoring varies according to treatment. For example, the usual recommendation for blood glucose monitoring when receiving basal insulin is before breakfast or bedtime, but this is increased for regimens that require multiple injections of insulin. The HCP should explain to the patient how these readings are used to interpret overall glycemic control and to assess for fasting and/or postprandial hyper- or hypoglycemia, and to guide dose adjustments and food choices. Use of SMBG/CGM provides an opportunity to enhance the HCPpatient relationship through information that can be used to support and educate the patient, and inform overall shared decision-making.
Table 1 Standardized CGM metrics for clinical care
The Importance Of Assessing Health Literacy
In preparing the delivery of diabetes education to enable shared decision-making, it is important to understand that health literacy varies from person to person . The American Diabetes Association Standards of Care state that clinicians and diabetes care/education specialists should provide easy-to-understand information and reduce unnecessary complexity when developing care plans in collaboration with people with diabetes . It is important to note, however, that matching the complexity of language used to a persons health literacy is associated with better understanding than the use of oversimplified language . People benefit greatly from acknowledgment of their emotional needs as well as clear explanation of the goals of therapy and how treatments work, using language tailored to their level of health literacy. Consideration of language barriers and cultural health beliefs, such as beliefs in traditional folk remedies and health misconceptions, is vital .
Don’t Miss: Fasting For Type 1 Diabetes
How Is Insulin Used
Most people use insulin as an injection, or shot. It is given into the fatty tissue just under the skin. Learning how to give yourself insulin may take some time. Youll also need to pay more attention to your blood sugar levels than you may be used to. But with practice, monitoring your levels and using insulin correctly can become a routine part of your day.
Assessment Of Older Adults With T2d
Psychological insulin resistance may be a particularly important consideration for insulin initiation in older adults . HCPs may also be more reluctant to initiate insulin therapy in older adults due to the perceived difficulty of managing hypoglycemia in this population. Assessment of comorbid depression using the Geriatric Depression Scale may be appropriate to identify patients who may benefit from a more holistic approach to therapy . When treating older adults with T2D, to reduce the risk of hypoglycemia, it may be appropriate to de-intensify their treatment, for example through using a basal insulin/glucagon-like peptide-1 receptor agonist fixed-ratio combination to remove the need for multiple insulin injections, or by using basal insulin in combination with other non-insulin regimens instead of prandial insulin. Additionally, individualized A1C targets may need to be reevaluated and relaxed. Some people with T2D may benefit from accessing recommended resources for patients, such as diabetes.org , or from a referral to a diabetes educator or local support groups.
Don’t Miss: How Much Does Farxiga Lower Blood Sugar
If Not Controlled At The Right Time Diabetes Can Lead To Kidney Failure Partial Or Complete Blindness Nerve Problems Loss Of Limbs And Increase The Risk Of A Heart Attack
Insulin, which is produced by the pancreas in the body, helps control the bodys blood sugar level. Regular insulin intake along with a proper diet and exercise plan is recommended for type 2 diabetes patients to help maintain their blood sugar level. If not controlled at the right time, diabetes can lead to kidney failure, partial or complete blindness, nerve problems, loss of limbs and even increase the risk of a heart attack. However, there are several myths around injecting insulin due to lack of awareness.
A study, published in the American Medical Associations biomedical journal JAMA Network Open, also found that the relative risk of death due to diabetes itself was much stronger among individuals who were underweight. The findings suggest that there is an urgent need to develop diabetes management programs that are tailored to Asian populations and the subsequent strong implementation of these programs in Asia.
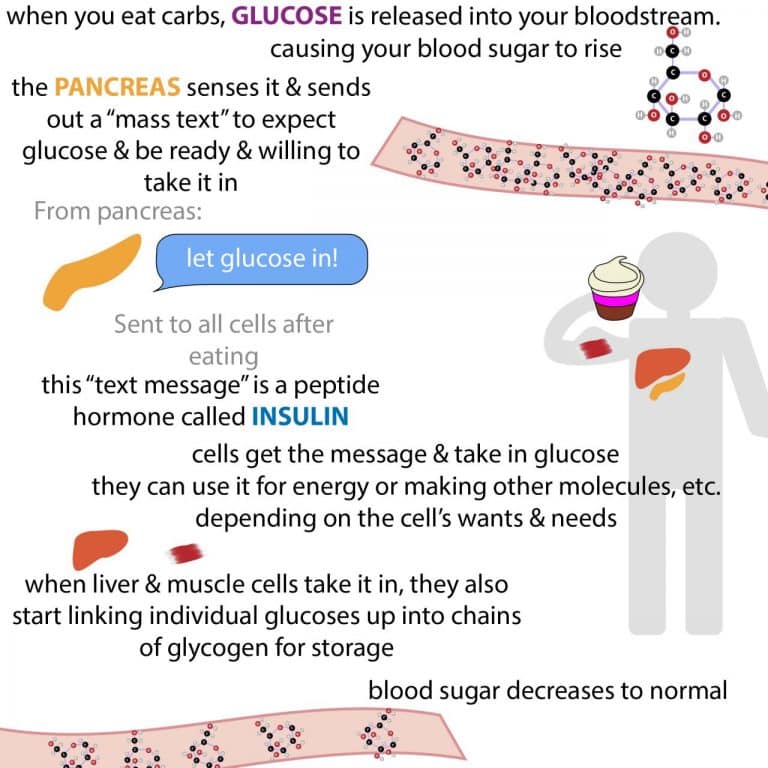
Why do Type 2 diabetics need insulin?
The pancreas, that produces digestive enzymes, is also responsible for producing insulin, a hormone that helps regulate blood sugar levels. Insulin helps the body use the carbohydrates in food for energy. If a patient develops Type 2 diabetes, their pancreas stop producing sufficient insulin that is required for the body to control blood sugar level, said Dr Roopak Wadhwa, consultant, department of diabetes endocrinology and metabolism at Fortis Hospital.
Tips while taking insulin injections
When Should Insulin Be Started
Q. Will my patient with type 2 diabetes require insulin?
A. It varies from patient to patient. However, type 2 diabetes is a progressive disease marked by gradual loss of beta cell function and most patients will eventually require insulin therapy.1 This should be viewed as part of the pathophysiology of the disease and not as a failure on the part of the patient or healthcare provider.
Insulin should be discussed early with patients who are beginning to show progression of their diabetes to ease the transition when the time to start insulin therapy arrives. This time should be considered part of a larger conversation between provider and patient, and not seen as a turning point down a path to the many severe complications of diabetes.
Q.Is there a specific hemoglobin A1c at which insulin must be started?
A. No. Insulin, like all treatments for diabetes, should be started and adjusted to achieve a reasonable goal HbA1c for the patient. The American Diabetes Association previously recommended that a patients HbA1c not be allowed to exceed 8%, creating an action point for escalation of therapy.
Insulin therapy will often need to be started if the initial fasting plasma glucose is greater than 250 or the HbA1c is greater than 10%.4_________________________________________________________________________________________________________________________________________________________________________________________________________________
References:
Also Check: Once Weekly Shot For Type 2 Diabetes
The Future Of Insulin
More insulin advances are percolating. There will be new insulins that act even faster. Improvements will be made in the open-loop pumps currently on the market, and efforts continue to develop the so-called artificial pancreas, or closed-loop system that promises, with several different models, to control blood sugar without the person having to do all the thinking.
Work also progresses on alternate ways to take insulin. The second generation of inhaled insulin is on the way with the FDAs approval of Afrezza in 2014. Investigation is ongoing for delivering insulin buccally via the tongue, throat, and cheeks or through a skin patch.
While the progress on new insulin products and delivery systems is encouraging, dont delay starting insulin if your health care provider and your diabetes health status indicate you need it now. The insulin available today is safe and relatively easy to take, and injections are nearly painless. Plus, starting to take insulin sooner rather than later may improve your health quickly and make your life better for many years to come.
> > > Discover The 1 Green Veggie That Worsens Diabetes Type 2 Symptoms
Diabetes can be managed through oral medications. In addition to insulin, metformin, which is a sugar-reducing agent, is also a common treatment for diabetes. It is considered a first-line therapy for diabetes treatment and is often added to insulin. It is important to know the risks of taking diabetes medications. Some drugs can be addictive, so you must consult your doctor before taking any medication. Your physician can prescribe you an appropriate treatment plan based on your medical history.
Your doctor will prescribe medication and check your blood glucose levels on a regular basis. Your A1c level will be checked every six months and your cholesterol levels will be tested regularly. Your doctor will also look for any signs of retinopathy, which is damage to the nerves in the eye caused by diabetes. You will also be examined for any foot problems. It is important to see a foot specialist regularly. Your feet should be thoroughly inspected for damage to the nerves.
While the first two types of insulin are the most common treatments, diabetes can be treated in a variety of ways. Your doctor may prescribe medications to control high blood pressure, which can protect the kidneys. Other types of medication include aspirin and other types of anti-platelet drugs. If your doctor is concerned about your blood sugar level, you may need to try a different medication. Some medications can cause side effects. Your treatment will depend on what type of insulin you need.
You May Like: Does Metformin Lower Blood Sugar
American Diabetes Association Guidelines
The American Diabetes Association recommends initiation of basal insulin at 10 units/day or 0.10.2 units/kg/day, adjusted by 1015% or 24 units once or twice weekly to reach a target fasting plasma glucose in patients whose A1C remains uncontrolled after > 3 months of triple combination therapy, whose A1C is > 10%, whose blood glucose is > 300 mg/dL, or who are symptomatic of hyperglycemia . details treatment intensification recommendations for patients whose A1C remains uncontrolled after basal insulin initiation and titration. Three regimen options should be considered:
-
Regimen 1: Administer one rapid-acting insulin injection before the meal with the greatest carbohydrate content if the glycemic target is not met, progress to two or more rapid-acting insulin injections before meals .
-
Regimen 2: Add a GLP-1 receptor agonist. If target A1C remains unmet or the regimen is not tolerated, patients may discontinue the GLP-1 receptor agonist and switch to regimen 1 or 3.
-
Regimen 3: Replace basal insulin with premixed insulin at a 75/25, 70/30, or 50/50 mix twice or thrice daily . Basal insulin and GLP-1 receptor agonists should be discontinued before initiating premixed insulin.
Connect With The Patients Emotional Needs
The management of diabetes is routinely focused on the clinical aspects of the disease involving lifestyle management and therapy however, as previously discussed, diabetes is also associated with emotional and distress-related experiences that directly affect the behavior and quality of life of the people who live with it .
For patients who have low health literacy, or where language is an issue, they may benefit by having someone close to them join them during consultation to help facilitate information exchange.
Also Check: How Can You Cure Diabetes
First Some Basic Things To Know About Insulin:
- Approximately 40-50% of the total daily insulin dose is to replace insulin overnight, when you are fasting and between meals. This is called background or basal insulin replacement. The basal or background insulin dose usually is constant from day to day.
- The other 50-60% of the total daily insulin dose is for carbohydrate coverage and high blood sugar correction. This is called the bolus insulin replacement.
Bolus Carbohydrate coverage
The bolus dose for food coverage is prescribed as an insulin to carbohydrate ratio.The insulin to carbohydrate ratio represents how many grams of carbohydrate are covered or disposed of by 1 unit of insulin.
Generally, one unit of rapid-acting insulin will dispose of 12-15 grams of carbohydrate. This range can vary from 4-30 grams or more of carbohydrate depending on an individuals sensitivity to insulin. Insulin sensitivity can vary according to the time of day, from person to person, and is affected by physical activity and stress.
Bolus High blood sugar correction
The bolus dose for high blood sugar correction is defined as how much one unit of rapid-acting insulin will drop the blood sugar.
Generally, to correct a high blood sugar, one unit of insulin is needed to drop the blood glucose by 50 mg/dl. This drop in blood sugar can range from 15-100 mg/dl or more, depending on individual insulin sensitivities, and other circumstances.
Meet With Your Healthcare Team
Working closely with your healthcare team is the first step to starting on insulin. Theyll discuss the importance of taking your insulin exactly as prescribed, address your concerns, and answer all of your questions. You should always be open with your doctor about all aspects of your diabetes care and overall health.
Recommended Reading: True Metrix Self Monitoring Blood Glucose Meter
Insulin Management Of Type 2 Diabetes Mellitus
ALLISON PETZNICK, DO, Northern Ohio Medical Specialists, Sandusky, Ohio
Am Fam Physician. 2011 Jul 15 84:183-190.
Insulin therapy is recommended for patients with type 2 diabetes mellitus and an initial A1C level greater than 9 percent, or if diabetes is uncontrolled despite optimal oral glycemic therapy. Insulin therapy may be initiated as augmentation, starting at 0.3 unit per kg, or as replacement, starting at 0.6 to 1.0 unit per kg. When using replacement therapy, 50 percent of the total daily insulin dose is given as basal, and 50 percent as bolus, divided up before breakfast, lunch, and dinner. Augmentation therapy can include basal or bolus insulin. Replacement therapy includes basal-bolus insulin and correction or premixed insulin. Glucose control, adverse effects, cost, adherence, and quality of life need to be considered when choosing therapy. Metformin should be continued if possible because it is proven to reduce all-cause mortality and cardiovascular events in overweight patients with diabetes. In a study comparing premixed, bolus, and basal insulin, hypoglycemia was more common with premixed and bolus insulin, and weight gain was more common with bolus insulin. Titration of insulin over time is critical to improving glycemic control and preventing diabetes-related complications.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Analogue insulin is as effective as human insulin but is associated with less postprandial hyperglycemia and delayed hypoglycemia.
How To Start Exercising With Diabetes
Use this step-by-step plan to create an exercise routine thats suited to your current fitness level and that will help keep you motivated as you progress:
Talk with your doctor. Before you begin an exercise program, get the go-ahead from your doctor. This is especially important if youre taking medication for diabetes, high blood pressure, or any other health issue, as well as if you have joint or muscle problems. If you have diabetes complications or joint or muscle problems, your doctor will explain which exercises are safe for you, and how to avoid any exacerbation of the specific medical problem, Shahar says.
You should also have a dilated eye exam and make sure to let your eye doctor know about your physical activity plans. Some restrictions may occur if you have major changes in your retina or leakage, Shahar adds.
Find out how exercise could change your medication needs. When you exercise your muscles contract and demand energy. Energy for muscles comes from glucose.
The more exercise you do, the more glucose you burn. At rest, insulin helps deliver glucose to your blood cells during exercise, however, glucose can enter these cells independently.
The muscles need to replenish themselves, and glucose uptake by the active muscles increases, Shahar explains. This process lasts 24 to 48 hours after exercise, which makes it a great way to manage blood glucose.
Recommended Reading: What To Do If You Think You Are Diabetic
At What Blood Sugar Level Should Insulin Be Given
If a person’s HbA1c level upon diagnosis is more than 10% or if a person’s fasting blood glucose level is continuously above 250 mg/dl, insulin is typically suggested as the initial therapy for diabetes. If someone’s HbA1c level is 7% to 9% and their fasting blood glucose levels are below 200 mg/dl, they may be able to avoid using insulin initially.
The American Diabetes Association recommends that insulin be used to treat people with Type 1 diabetes and those with Type 2 diabetes who do not achieve adequate control with lifestyle changes and oral medications. The association also states that insulin is usually necessary for people with Type 2 diabetes if they have not achieved good control with diet and exercise alone. Finally, the ADA says that insulin is an option for people with Type 2 diabetes who are at risk for complications but aren’t good candidates for alternative therapies.
People who have Type 1 diabetes need insulin because their bodies do not produce enough effective hormones called glucagon or insulin. People who have Type 2 diabetes often require insulin because they fail to properly use insulin or lose the ability to respond effectively to it over time. Some people with Type 2 diabetes may be able to control their condition with pills or other drugs rather than insulin. However, these individuals are still advised to test their blood sugar regularly because failure to do so could lead to serious health problems.