What Is Nonproliferative Diabetic Retinopathy
High blood sugar levels cause damage to the fine vessels that supply blood to the retina, the light-sensitive tissue inside your eyes. As this damage accumulates, your doctor can begin to see the earliest signs of diabetic changes in your retina distortion of the vessels and tiny retinal hemorrhages. When the damage has not progressed to the point where new, abnormal blood vessels are growing to try to replace damaged ones, then we call the diabetic damage nonproliferative diabetic retinopathy.
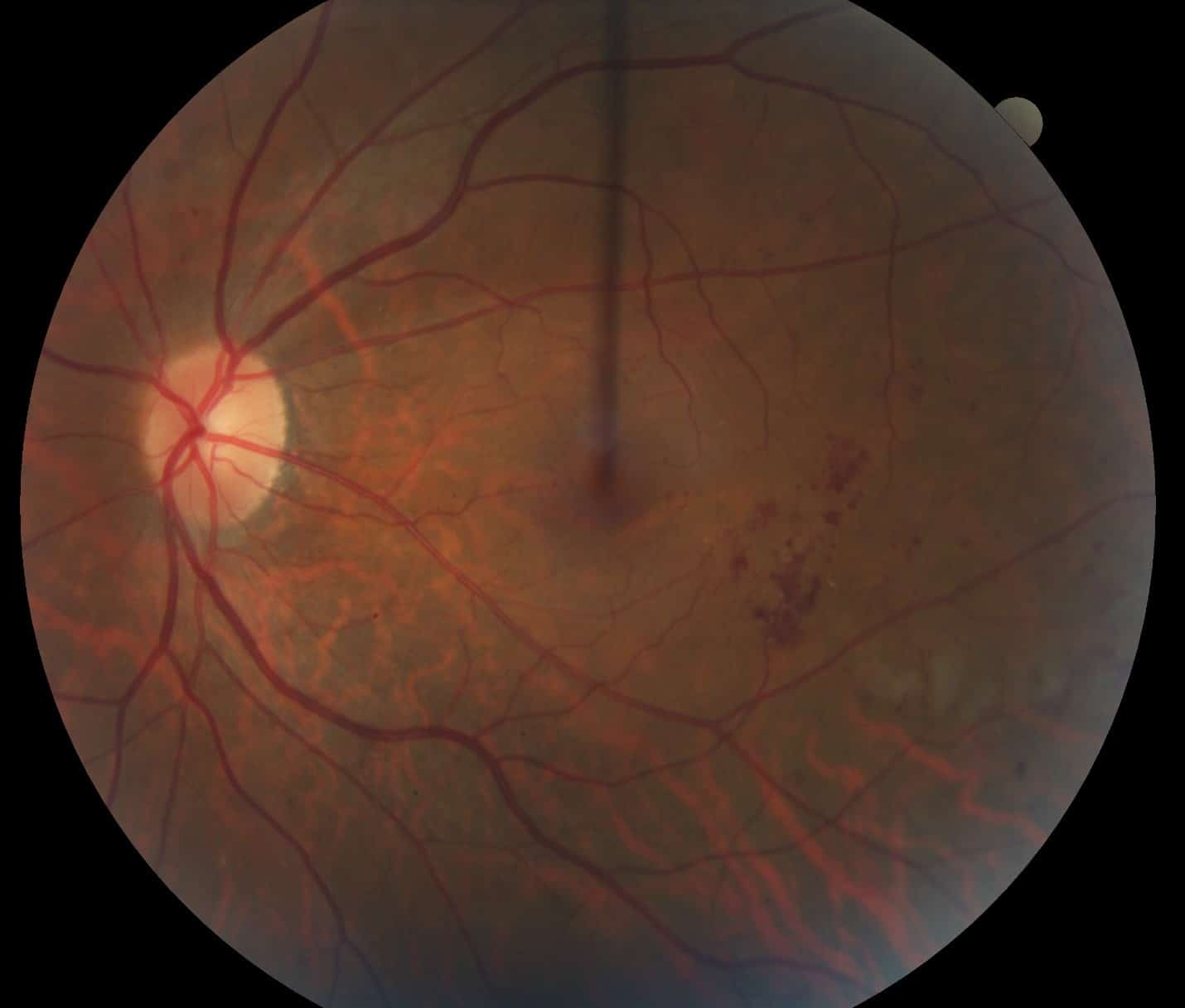
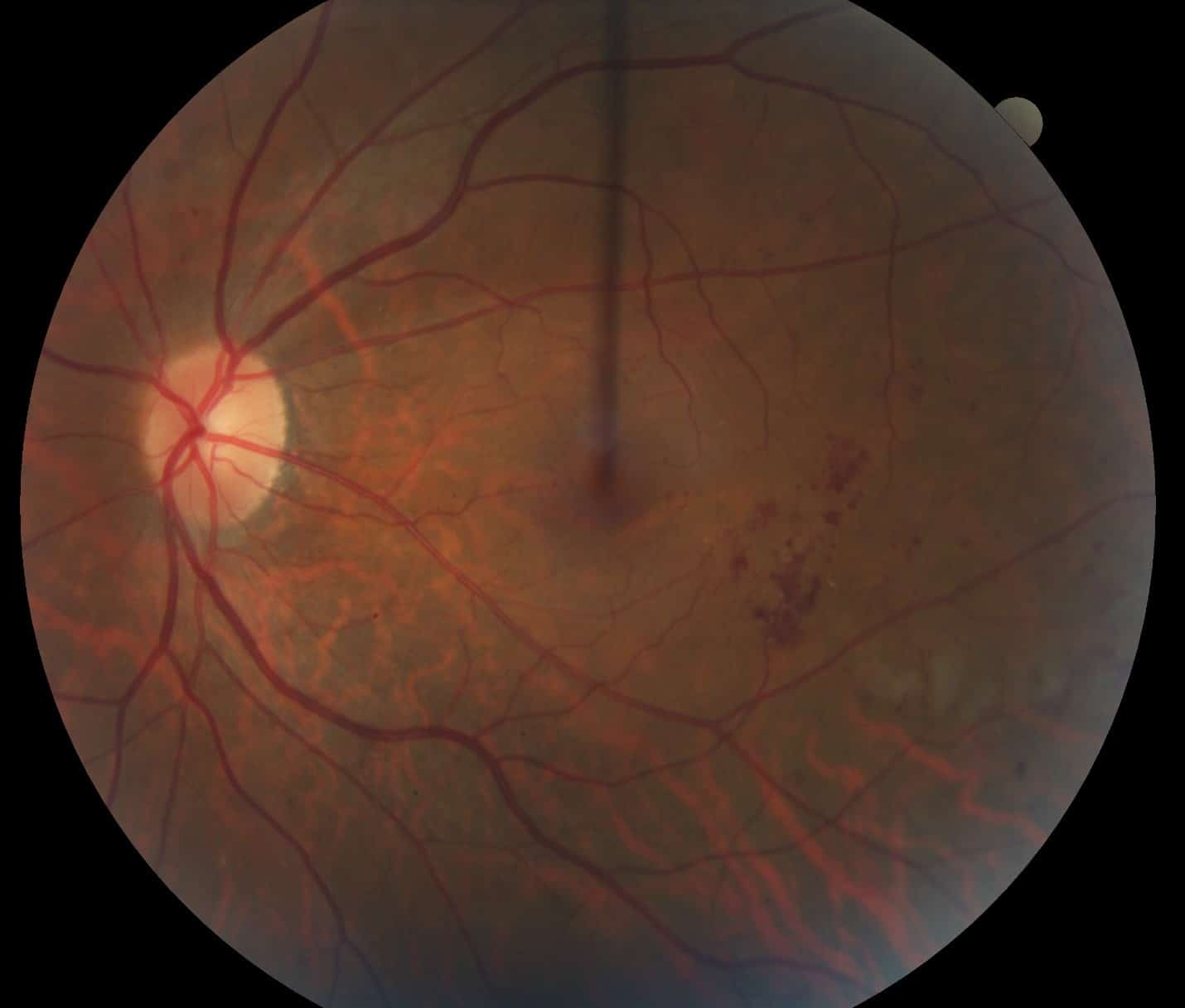
This color photograph illustrates areas of red dots and blots that indicate hemorrhage from diabetic damage to the retina. Also, there are white areas of fatty deposition in an area of swollen retina, a condition called diabetic macular edema
Diabetic Retinopathy Level And Management
Level of Retinopathy
Zone of retinal thickening 1DD in size within 1DD of the macular center
Fundus photo FA macular OCT Non center- involved macular edema: Two months to four monthsCenter-involved macular edema: retina referral within one week to two weeks =RecommendedNPDR=nonproliferative diabetic retinopathy PDR=proliferative diabetic retinopathy MA=microaneurysms Hemes=hemorrhages CWS=cotton wool spots VB=venous beading IRMA=intra-retinal microvascular abnormalities NVD=neovascularization of the disc NVE=neovascularization elsewhere VH=vitreous hemorrhage PRH=preretinal hem- orrhage CSME=clinically significant macular edema CI=centrally involving DD=disc diameter
Lastly, remember that diabetic macular edema can occur at any level of retinopathy, from mild NPDR to proliferative disease.
Traditionally, diabetic macular edema was classified as CSME if any of the following criteria were met:
1. Thickening of the retina at or within 500µm of the center of the macula 2. Hard exudates at or within 500µm of the center of the macula with thickening of the adjacent retina 3. A zone or zones of retinal thickening greater than 1 disc area in size, any portion of which is within 1DD of the center of the macula.32
| Taken with an an Eidon True Color Confocal Scanner, this image shows a patient following extensive panretinal photocoagulation for proliferative diabetic retinopathy. Click image to enlarge. |
How Is Nonproliferative Diabetic Retinopathy Treated
Not all forms of nonproliferative diabetic retinopathy require treatment to the eyes, but all patients require continued care and blood sugar control through their primary care provider. If the diabetic damage includes a significant degree of swelling in the central portion of the retina, a condition called diabetic macular edema, medical therapy with injections of drugs in the eye or laser therapy may be recommended for the eyes involved. Injections of medications have become the most common modern treatment for diabetic macular edema and have the greatest chance for arresting the progression of the diabetic damage and in some cases restoring some lost vision. Laser photocoagulation is also a common treatment for nonproliferative diabetic retinopathy with macular edema. In this kind of procedure, painless brief spots of bright light are used to treat the retina to reduce further loss of vision from diabetic macular edema. Laser surgery may need to be repeated several times. If the diabetic retinopathy progresses beyond the nonproliferative stage to the proliferative stage, a different type of laser therapy may be recommended.
In 2020, we joined together with other elite retina-only practices and formed Retina Consultants of America, now the premier national retina provider in the USA.
Read Also: Genetic Testing For Diabetes Type 1
Treatment Depends On Severity And Ranges From Observation To Intravitreal Injection Or Laser Photocoagulation
For years, the treatment paradigm for patients with diabetic retinopathy was fairly well-established. Recently, however, the advent of anti-vascular endothelial growth factor injections and data from studies are changing some treatment patterns. Heres a review of how retina specialists currently approach these patients, after taking into account all of the recent developments.
Treatment Philosophy
Treatment for nonproliferative diabetic retinopathy depends on severity. Assuming theres no diabetic macular edema, most cases of mild NPDR can be observed. More advanced cases-moderately severe to severe NPDRcan be considered for treatment, which typically includes intravitreal injection or laser photocoagulation.
|
Severe NPDR in a patient with significant peripheral nonperfusion on fluorescein angiography. |
Whether to use injection or laser, as well as the length of treatment, is up for debate. Obviously, if you ask 10 retina specialists, Im sure youll get different answers, says Tom Stone, MD, who practices in Lexington, Kentucky. For me, it depends on the underlying condition of the patient. If someone has kidney disease, hypertension, or if he or she smokes or is obese, these conditions will further compound the care of NPDR. I would consider anti-VEGF therapy in these patients. In other patients who have mild cases, I will just watch them and try to coordinate with their primary care physician to optimize their systemic status.
Moderately Severe and Severe Cases
What To Look For
Patients with NPDR generally present with hemorrhages of varying sizes, microaneurysms , hard exudates, soft exudates intraretinal microvascular abnormalities , and venous looping or beading.2,5,6 MAs are saccular outpouchings of retinal capillaries that have been weakened by a loss of intramural pericytes.4 The weakened capillary walls can leak or rupture, causing hemorrhages.2 IRMAs are either new vessel growth within the retina or preexisting vessels with proliferative endothelial cells that are moving through areas of nonperfusion. Presence of IRMA indicates ischemia and is a precursor to neovascularization.2 Venous looping and beading are caused by severe retinal hypoxia and indicate an increased risk for progression to neovascularization.2 When patients with diabetes are in your chair, its important to gather as much information about their condition as possible .
You May Like: Type 1 Diabetes Insulin Pen
Type 2 Diabetes Mellitus With Mild Nonproliferative Diabetic Retinopathy With Macular Edema
- 20162017 – Converted to Parent Code201820192020202120222023Non-Billable/Non-Specific Code
- E11.321 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
- Short description: Type 2 diab w mild nonprlf diabetic rtnop w macular edema
- The 2023 edition of ICD-10-CM E11.321 became effective on October 1, 2022.
- This is the American ICD-10-CM version of E11.321 – other international versions of ICD-10 E11.321 may differ.
- Applicable To annotations, or
Staging And Assessing Efficacy Of Potential Therapies
Limitations of current staging methods.
Surrogate outcomes.
As new treatments become available, alternative outcomes must also be devised that can accurately predict the progression of DR from its initial stages. For example, the detection and quantitation of microaneurysm formation and/or other retinal capillary abnormalities using FA may be a sufficiently sensitive means to evaluate the effect of pharmacological therapy on early changes in the blood-retinal barrier . The situation is greatly complicated by the nonlinear progression of DR. Clinical signs may spontaneously resolve and thus may mask true progression of the disease . There is no straightforward method to address this issue at present and more research is needed in this area. The use of multiple surrogate end points, such as a two-step ETDRS progression, measurement of retinal thickness, and assessment of fluorescein leakage, has been proposed as one means to overcome this obstacle . Such outcomes will need to be validated in clinical trials to determine whether they can accurately predict progression of DR in a clinically useful manner.
You May Like: Glucose 6 Phosphate Dehydrogenase Deficiency
Join Forces To Deliver Proper Care
As the number of US patients with diabetes grows, it is important for optometrists to collaborate with PCPs, endocrinologists, and retina specialists on managing these patients disease. This teamwork, combined with effective communication among caregivers and with patients, will enhance the care that they receive.
- 1. Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984 102:520-526.
- 2. American Optometric Association. Evidence-based Clinical Practice Guideline: Eye Care of the Patient With Diabetes Mellitus. www.aoa.org/optometrists/tools-and-resources/evidence-based-optometry/evidence-based-clinical-practice-guidlines/cpg-3–eye-care-of-the-patient-with-diabetes-mellitus. Accessed May 2, 2019.
- 3. Stratton IM, Kohner EM, Aldington SJ, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001 44:156-163.
Dos And Donts In Managing Diabetic Retinopathy:
- DO watch your diet to control blood sugar levels.
- DO remember that untreated diabetic retinopathy can cause severe vision loss and blindness.
- DO remember that macular edema may need focal laser treatment more than once.
- DO call your health care provider if you have symptoms of uncontrolled diabetes .
- DO call your health care provider if you notice vision changes.
- DONT smoke or drink alcohol.
- DONT wait until you have symptoms. Get yearly eye examinations.
- DONT forget that proliferative retinopathy and macular edema can develop without symptoms.
You May Like: What Dairy Products Are Good For Diabetics
Nonproliferative Diabetic Retinopathy Without Diabetic Macular Edema
Unlabelled OCT
Want to be able to interpret OCTs like an expert?We can show you how!
For past issues, checkout the newsletter archive.
Privacy notice
Privacy Overview
Necessary cookies are absolutely essential for the website to function properly. This category only includes cookies that ensures basic functionalities and security features of the website. These cookies do not store any personal information.
Any cookies that may not be particularly necessary for the website to function and is used specifically to collect user personal data via analytics, ads, other embedded contents are termed as non-necessary cookies. It is mandatory to procure user consent prior to running these cookies on your website.
Analytical cookies are used to understand how visitors interact with the website. These cookies help provide information on metrics the number of visitors, bounce rate, traffic source, etc.
Performance cookies are used to understand and analyze the key performance indexes of the website which helps in delivering a better user experience for the visitors.
We use essential cookies to make our Website work. These cookies are strictly necessary to enable core functionality such as security, network management, your cookie preferences and accessibility. Without them you wouldnt be able to use basic services. You may disable these by changing your browser settings, but this may affect how the website functions.
Role Of Oxidative Stress And Use Of Antioxidant Compounds
Production of reactive oxygen species has been implicated in the development of diabetic complications . Diabetes may cause ROS production through glucose auto-oxidation, increased flux through the polyol pathway, and increases in protein glycation . ROS may activate aldose reductase and PKC and increase AGE production and DAG formation .
The pervading role of ROS in the biochemical processes leading to microvascular damage has prompted an investigation of antioxidants as preventive therapy for diabetic complications . Inhibition of superoxide production can effectively block sorbitol accumulation, AGE formation, and PKC activation . These findings suggest that ROS production is associated with at least three mechanisms of diabetes-induced vascular damage. Antioxidants are effective inhibitors of pericyte loss secondary to diabetes in experimental models . Tocopherol also inhibits hyperglycemia-induced DAG production and PKC . Tocopherol prevents retinal hemodynamic abnormalities in diabetic rats . In patients with type 1 diabetes and little or no baseline retinopathy, retinal blood flow was significantly increased after 4 months of tocopherol therapy . Recent results of the Heart Outcomes Prevention Evaluation study and other trials showed a lack of effect of tocopherol in the prevention of cardiovascular risks, despite suggestive evidence to the contrary .
Don’t Miss: A1c 6.1 Average Blood Sugar
What Is Diabetic Retinopathy
Diabetic retinopathy is an eye disease caused by diabetes mellitus. It affects the retina, the part of the eye that lets us see. Diabetes hurts the retinas tiny blood vessels and can cause swelling and leaking of fluid into the eye. Extra retinal blood vessels can grow, which damages eyesight. Diabetic retinopathy is the leading cause of blindness in people 20 to 70 years old. All people with diabetestype 1 or 2are at risk. Almost half of Americans with diabetes have some stage of diabetic retinopathy. There are four stages of diabetic retinopathy. The first is early mild nonproliferative retinopathy, with small balloon-like swollen areas in tiny retinal blood vessels. Then moderate nonproliferative retinopathy occurs, with blocked blood vessels. Severe nonproliferative retinopathy follows . In the advanced stage , new abnormal, fragile blood vessels grow along the retina and watery soft gel inside the eye.
Other Potential Therapies For Retinopathy Prevention
Somatostatin activity is linked with the progression of DR , and hypophysectomy has been proposed as an intervention for severe treatment-resistant DR. Consequently, somatostatin has been evaluated for the treatment of DR . Early results in patients with PDR were encouraging, although some evidence for resistance to the drug was noted . In a recent trial of patients with severe nonproliferative DR or early PDR, therapy with octreotide decreased the need for retinal photocoagulation compared with conventional treatment . However, the incidence of progression to severe PDR was not significantly different between the treatment arms . Additional controlled trials will determine whether somatostatin analog therapy is a viable therapeutic option for patients with more advanced stages of DR.
Read Also: How Much Is Tresiba Insulin
A Guide To Following And Educating Patients Who Face This Sight
Today, optometrists play a crucial role in managing diabetes, a leadingand growinginstigator of vision loss. With management of this disease now firmly in optometrys wheelhouse, the depth of research into its ocular impact has provided the ability to delineate its progression using various categories. In the case of diabetic retinopathy, these are divided, chiefly, into two: proliferative diabetic retinopathy and nonproliferative diabetic retinopathy. These categories are each further split by severity. It may seem like minutiae, but even minor distinctions can be valuable as they inform our treatment protocol and, ultimately, prevent significant visual impairment for our patients.
This article explains the care diabetes patients require and details the biological processes that indicate where to classify a patient with diabetic retinopathy, as well as what treatment should follow.
How Is Diabetic Retinopathy Treated
For early disease, no treatment may be needed.
Two treatments can help people with advanced disease: laser surgery and vitrectomy . In the first procedure, which is painless, a laser beam is used to destroy abnormal blood vessels. Focal laser surgery is used for macular edema a small laser burns slow leakage from vessels. A similar scatter laser treatment helps shrink abnormal blood vessels in proliferative retinopathy. In vitrectomy, blood that leaked from vessels is removed.
Control of blood sugar levels and other risk factors is important to prevent worsening disease.
Recommended Reading: What Brand Of Glucose Meter Is Covered By Medicare 2022
Role Of Ages And Use Of Age Inhibitors
Carbohydrates interact with protein side chains in a nonenzymatic fashion to form Amadori products, and these may subsequently form AGEs, especially in the presence of high glucose . Excessive formation of AGEs has been proposed as another biochemical link between diabetes and the development of microvascular complications. AGEs may affect such functions as enzyme activity, binding of regulatory molecules, and susceptibility of proteins to proteolysis . The chronic interaction of these products with at least one specific cell surface receptor for AGEs may perpetuate a proinflammatory signaling process and a pro-atherosclerotic state in vascular tissues . In vitro, the AGEAGE-specific receptor interaction has been associated with oxidative stress and the activation of nuclear factor-B, which leads to hyperexpression of proinflammatory cytokines, lymphocyte adhesion molecules , vasoactive mediators, and pro-coagulant factors . These processes may result in disruptions of retinal hemodynamics and/or damage to vascular endothelial cells. Accordingly, strategies to reduce AGE formation in the absence of achieving euglycemia have been investigated as potential preventive therapies for diabetic microvascular complications .
How Is The Diagnosis Of Nonproliferative Diabetic Retinopathy Made
The first step is a careful eye exam where both pupils are dilated. To supplement the direct examination of your eye with lights and lenses, the circulation of the retina can be carefully assessed with a special test called a fluorescein angiogram. This is a photographic study of the back of the eye performed after an orange-colored dye is injected in a vein in the hand or arm. The dye circulates through the body into the eye to highlight abnormal vessels, or where treatment may be needed. In addition, the degree and extent of damage to the center of the retina, called the macula, can be evaluated by a painless retina imaging system called an optical coherence tomography scan .
This is an example of an angiographic image of nonproliferative diabetic retinopathy. Note the dark spots indicating areas of hemorrhage and the white dots that indicate areas where diabetes has damaged blood vessels.
Don’t Miss: Insulin Glargine 300 Units Ml
Does Diabetes Cause Macular Edema
Yes, diabetes is one potential cause of macular edema. Persistently high blood sugar levels affect can affect blood vessels in the eye, causing them to leak. That, in turn, results in swelling of the macula and DME.
DME affects more than 28 million people around the world, according to the International Diabetes Federation. About 20 percent of people with type 1 diabetes and up to 25 percent of people with type 2 diabetes develop DME after 10 years, according to research from 2016.
In the United States, approximately 7.7 million people have diabetic retinopathy. Of those, 750,000 also have DME, per the .
DME can occur at any stage of diabetic retinopathy, but the risk increases as the condition progresses.
DME is more common in men than women. You may also be at higher risk of DME if you have the following conditions:
- high blood sugar
My Vision Seems Fine Can I Still Have Diabetic Retinopathy
Yes. Often there are no visual symptoms in the early stages of nonproliferative diabetic retinopathy. The vision usually deteriorates as progressive damage occurs to the vessels in the central part of the retina, called the macula. Diabetic injury to the blood vessels in the macula can cause swelling or ischemia nerve damage from lack of blood flow. It is important not to wait for symptoms to occur before having your eyes examined for diabetic damage. Treatments to preserve your vision from diabetic damage are much more successful if the disease is consistently monitored and treated in its earlier stages
Don’t Miss: 3 Hour Glucose Tolerance Test Pregnancy Normal Range