What Is Dme In Diabetic Retinopathy
DR carries a possibility for complications such as diabetic Macular Edema . In its simplest form, arfunctioning occurs due to long-term hyperglycemia in disrupting the blood-retinal barrier, resulting in an excessive layer of retinal thickened to the fovea itself. It affects over 28 million people with diabetes with a potential effect of chronic fatigue disorder.
Causes And Symptoms Of Diabetic Macular Oedema
Diabetic macular oedema refers to a build-up of fluid in a part of the eye called the macula. The macula is an area in the centre of the retina that has a very high concentration of light receptor cells. The macula is responsible for ensuring our central vision is clear, sharp, and correctly detailed. For example, the macula would be at work if we were to thread a needle or read small print. When there is swelling and thickening in the macula, this causes our vision to distort. This occurs due to damaged blood vessels in the surrounding retina.
Symptoms of DMO include wavy or blurry vision in the centre of the visual field, and colours may appear faded or washed out. The severity of DMO symptoms can range from a slight blurring of vision to noticeable vision loss. If only one eye is affected, changes in vision may go unnoticed until the condition is quite advanced2.
Worsening vision due to diabetic retinopathy and/or diabetic macular oedema can have a considerable impact on daily life, leading to difficulties reading or at work, participating in leisure activities, and completing household and personal care tasks.
What To Look For
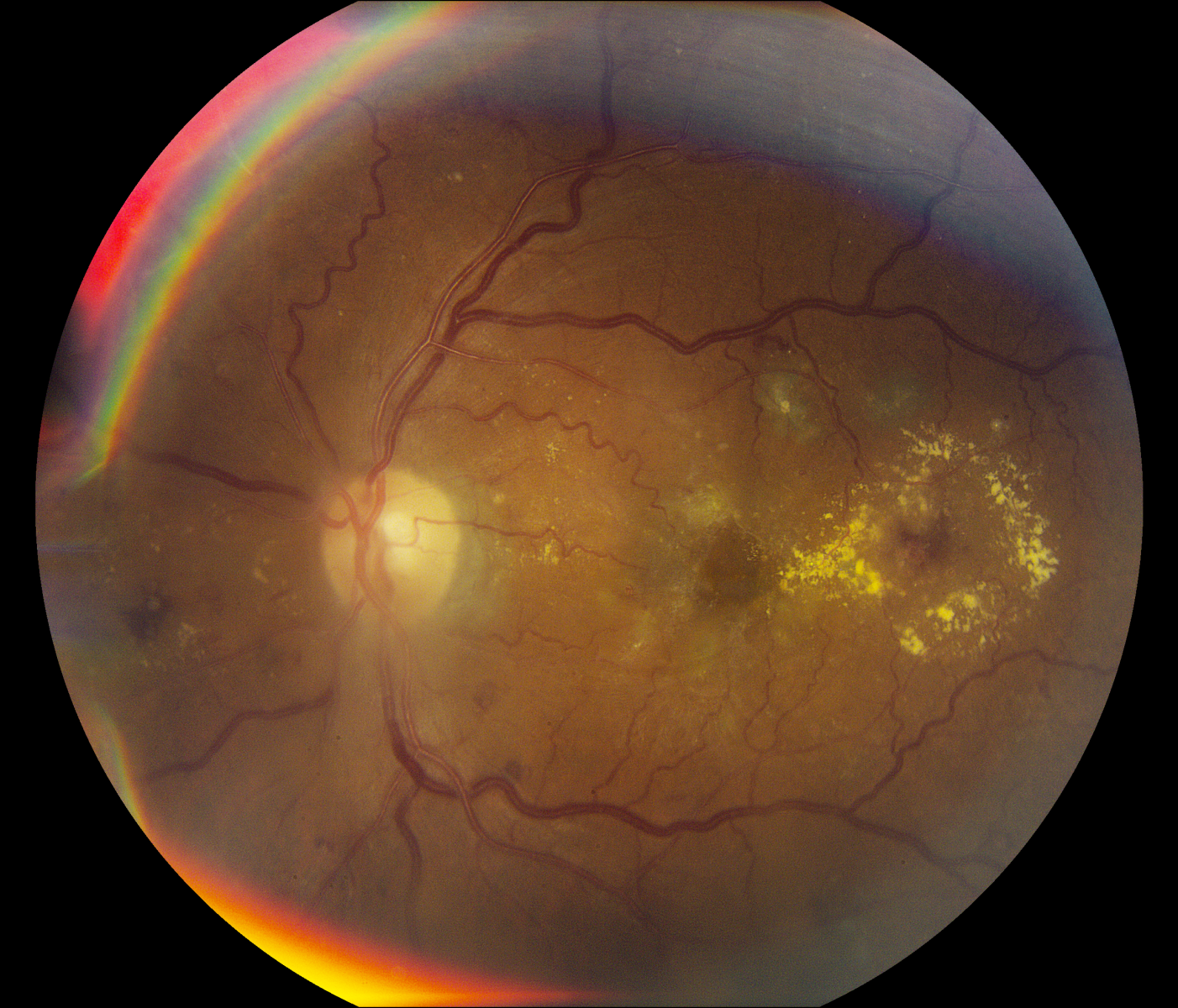
Patients with NPDR generally present with hemorrhages of varying sizes, microaneurysms , hard exudates, soft exudates intraretinal microvascular abnormalities , and venous looping or beading.2,5,6 MAs are saccular outpouchings of retinal capillaries that have been weakened by a loss of intramural pericytes.4 The weakened capillary walls can leak or rupture, causing hemorrhages.2 IRMAs are either new vessel growth within the retina or preexisting vessels with proliferative endothelial cells that are moving through areas of nonperfusion. Presence of IRMA indicates ischemia and is a precursor to neovascularization.2 Venous looping and beading are caused by severe retinal hypoxia and indicate an increased risk for progression to neovascularization.2 When patients with diabetes are in your chair, its important to gather as much information about their condition as possible .
Don’t Miss: Can You Join The Airforce With Diabetes
Study Subjects And Materials
The present study included patients with type 2 diabetes diagnosed with DR by CFI and FA, who referred to the First Hospital of China Medical University between January 2015 and December 2020. The medical records, including age, sex, CFI , FA , and OCT scan results, were reviewed and measured. The scanning quality index of the OCT was above 60. We identified the same 50° angle of the view between the CFI and FA .
Figure 1. The medical record of a 63-year-old patient with diabetic retinopathy . color fundus images , fundus angiography , and optical coherence tomography .
Using the International Clinical Diabetic Retinopathy Disease Severity Scale , we evaluated the severity of DR in CFI and FA, which was also based on previous studies . A DME was defined by hard exudates in the presence of microaneurysms and blot hemorrhages within one-disc diameter of the foveal center . Seven central horizontal lines of the OCT that were 6-mm length in their maculas were selected, and central foveal thickness was automatically measured by a built-in software. The type of DME in the OCT images was assessed according to a previous study , where XB and RH accomplished the grading work together, including CFT, FA, and OCT. The patients who had poor quality images, other retinal diseases, or a history of ocular interventions were excluded.
Stage : Moderate Npdr
These patients have hemorrhages or MAs in one to three retinal quadrants and/or cotton wool spots, hard exudates, or venous beading .2, 5-7
Figure 2. This patient with type 2 diabetes has moderate NPDR and macular edema. Note the MA and hard exudates within the macula and the moderate, scattered dot hemorrhages throughout both the inferior and superior arcades.
Patients with moderate NPDR should be seen every 6 to 8 months.2,7 There is a 12% to 27% risk that they will develop proliferative diabetic retinopathy within 1 year.2 The use of fundus photography is suggested for these patients, and you may obtain macular OCT images at your discretion if you suspect DME. These patients do not need to be referred to a retina specialist unless you have confirmed DME or you believe OCT imaging is warranted but do not have access to this technology.
Again, it is important to educate these patients on the findings and what they suggest about the disease process. Depending on their recent blood sugar control and last diabetes examination with their PCP or endocrinologist, it may be necessary to refer patients back to those providers sooner than scheduled so that they can consider changes in treatment.
You May Like: How To Treat Hypoglycemia In Type 2 Diabetes
What Is Diabetic Retinopathy
Diabetic retinopathy affects people with diabetes, and occurs when high levels of sugar in the bloodstream cause progressive damage to the retina.
Diabetes causes damage to the blood vessels in the body, including the retina. As a result, the blood vessels leak blood and other fluid into the eye, causing the retinal tissue to swell and cloudy or blurred vision. Moreover, as these blood vessels are destroyed, new abnormal blood vessels are produced. These new blood vessels are fragile and even more susceptible to leaking and bleeding fluid into the eye.
Diabetic macular edema occurs when damaged blood vessels from the retina leak fluid into the macula, the center of the retina.
Diabetic macular edema can occur at any stage of diabetic retinopathy, though it generally develops as the disease progresses to more advanced stages.
Diabetic macular edema causes the macula to swell and thicken, resulting in distorted vision.
Can Macular Edema Be Cured Naturally
It is impossible to cure macbook edema completely, but it is possible to treat it effectively based on early detection. A treatment regimen for Macular Edema early on in its development should preserve vision better for its associated symptoms. It may take months to recover from swelling of the central lip caused by scarring of the blood vessels.
Don’t Miss: Type 1 Diabetes And Anxiety
Is Diabetic Macular Oedema The Same As Diabetic Retinopathy
No, but the two conditions are intimately linked: diabetic retinopathy is a common cause of diabetic macular oedema, and DMO is the most common cause for vision loss in people who have DR. Macular oedema typically develops as retinopathy worsens, but it can occur at any stage of DR. However, not everyone with diabetic retinopathy will necessarily develop diabetic macular oedema. Experts estimate that around 10% of people with DR also have DMO2.
Modern Scanning Laser Photocoagulation
As laser technology has evolved and improved over the last several decades, emphasis has been placed on developing modifications to conventional retinal laser therapy in order to minimize retinal damage and adverse side effects, while maintaining the excellent therapeutic effect of the conventional approach. To this end, most of the innovations have focused on changing the laser pulse duration, wavelength, and spot size to achieve these goals.
Fundus photograph comparing conventional laser and patterned scanning laser , demonstrating more uniformly spaced, small, and less intense spots provided by the pattern scanning laser. Reprinted with permission from Paulus, Y. M., Palanker, D., & Blumenkranz, M. S. . Short-pulse laser treatment: redefining retinal therapy. Retinal Physician, 7, 5456
Read Also: Why Do Diabetics Legs Swell
Diagnosis And Ancillary Testing/differential Diagnosis
DR is diagnosed clinically on the basis of visible hemorrhages, microaneurysms, cotton wool spots, lipid exudates, and neovascularization. Fundus photography and fluorescein angiography have greater sensitivity than ophthalmoscopy because of superior optics, the enhanced contrast of fluorescein angiography, confirmation of vascular leakage, and the ability of the observer to review magnified images without the interference of patients moving or blinking.
Progression And Regression Of Dr
A large number of cohort studies have investigated progression and regression of DR . Disease severity was most often classified by the Early Treatment Diabetic Retinopathy Study classification for DR severity . The cohort with the longest follow-up time was the WESDR cohort, which reported 25-year progression of DR in patients with type 1 diabetes . In this study, DR severity was assigned a level by concatenating the severity grade in both eyes, with the worse eye given greater weight. This created a 15-step scale, and progression was defined as increase in severity of 2 steps or more. Some other studies assigned DR severity based on the severity grade in the worse eye alone. The findings on DR progression and regression from the various cohort studies are summarized in Table . Four to six-year cumulative incidence of 2-step progression among the studies ranged from 24.1 to 38.9 %, which increased to 64.1 and 83.1 % in studies with 16-year or 25-year follow-up.
Also Check: How Can An Ophthalmologist Help A Diabetic
Get Support From The Lucentis Patient Support Program
If you have diabetic retinopathy or diabetic macular edema, join the LUCENTIS Patient Support Program to receive more information and support, including:
The Genentech Ophthalmology Support Line that makes it easy for you to quickly access the information and support you need. Our representatives are available MondayFriday, 9 to 8 Eastern Time.
Brochures mailed to your home
Emails with tips and resources to help you stay on track
Information on patient assistance options from Genentech Ophthalmology Access Solutions
What Causes Diabetic Macular Edema

It is believed that in order to induce the edema, there should be leakage of moist, abnormal fluids from damaged blood vessels in the eye in the left side of the retina to the macula. Medical experts recommend preventing scarring if its associated with diabetic retinopathy, the disease that occurs when people take their medication regularly.
Read Also: How Do Diabetics Check Their Blood Sugar
Upcoming Innovative Clinical Laser And Delivery Platforms
In addition to the efficacious novel laser approaches outlined above , several other important clinical innovations are likely to become main-stream in busy retina practices over the next few years, including endpoint management and image-guided navigated laser delivery. Table compares the parameters and indications for several of these novel laser techniques.
I Get Diabetic Macular Oedema
Diabetic retinopathy and diabetic macular oedema are both eye conditions that can affect people with diabetes.
Diabetic retinopathy is a condition where the blood vessels that supply the retina the part of your eye responsible for forming images are damaged. Diabetic macular oedema may then develop as a result of this damage, causing fluid to accumulate in the macula. The macula is the part of the retina responsible for making sure our vision is clear and sharp. If left untreated, either condition can potentially lead to severe vision loss and blindness.
It can be quite overwhelming to be diagnosed with a diabetic eye disease. The good news is that tests can detect these conditions before they affect your eyesight, and there are treatments available that can prevent further damage from occurring. This article will help you understand the link between diabetic retinopathy and diabetic macular oedema, and what to do if you suspect you have either condition.
Also Check: Best Cookbook For Type 1 Diabetes
Stage : Proliferative Diabetic Retinopathy
These patients had NPDR that has progressed to PDR, and they exhibit either neovascularization of the disc/elsewhere or vitreous/preretinal hemorrhage.2,5-7
These patients require immediate referral to a retina specialist for further testing and treatment. Peripheral neovascularization is usually treated with laser panretinal photocoagulation .7 They also often receive anti-VEGF intravitreal injections that may be performed in conjunction with PRP.7
Figure 4. This patient with type 2 diabetes was treated with laser PRP in the periphery for PDR in both eyes.
Until their disease stabilizes, these patients need to be monitored monthly by a retina specialist.7 Thereafter, they may be seen every 6 to 12 months.7
Communicate all findings to the patients PCP and/or endocrinologist. A phone call is warranted if the patient has new-onset PDR.
Other Eye Complications Of Diabetes
While DR and DME are the most important and well-studied diabetes-related eye complication, many patients with diabetes are at risk of vision loss from other diabetes-related eye conditions that range from mild vision impairment to blindness. Diabetes is associated with early and rapid development of cataracts, and is hence a major cause of visual impairment among patients with diabetes. The Singapore Malay Eye Study found patients with diabetes to be more likely to have cortical and posterior subcapsular cataracts . In the WESDR study and SN-DREAMS study, presence of cataracts were significant factors contributing to visual impairment and blindness in patients with diabetes . Many patients with diabetes require cataract surgery at a relatively younger age. In the WESDR, 10-year cumulative incidence of cataract surgery was 8 % in patients with type 1 diabetes and 25 % in patients with type 2 diabetes . While usually a surgical procedure with good outcomes, cataract surgery is complicated in patients with diabetes as they may develop DME after surgery .
Also Check: Advanced Diabetes Supply Freestyle Libre
How Does Retinal Laser Therapy Treat Diabetic Eye Disease
The principle of retinal laser therapy resulting in therapeutic effects in the target retinal tissue is based upon the absorption of light by ocular pigments, predominantly in the retinal pigment epithelium and choroid melanin and hemoglobin. Conventional photocoagulation results in permanent chorioretinal scars, although some of the newer laser modalities utilizing reduced intensity and pulse duration may not have such permanent tissue effects, based upon studies in animal models . The differences between these laser treatment types will be reviewed later in this article.
The exact mechanism by which retinal laser therapy results in effective treatment and improvement of retinal vascular disease is not fully understood. With regards to PRP for PDR, one possible mechanism is that damage to the retinal cells by laser photocoagulation in areas of poor retinal perfusion decreases the overall retinal oxygen demand and the level of retinal hypoxia, with subsequent downregulation of angiogenic factors and VEGF production by the retinal tissue and subsequent increased oxygen perfusion to the remaining viable retina . Photoreceptors are the most metabolically active and numerous cell type within the retina, and PRP treatment involves the purposeful destruction of a fraction of photoreceptors in the peripheral retina to reduce overall oxygen demand. The resulting decrease in VEGF production by the retina also results in decreased retinal vascular permeability and retinal edema .
Causes & Risk Factors
Diabetic retinopathy results from the damage diabetes causes to the small blood vessels located in the retina. These damaged blood vessels can cause vision loss:
- Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
- In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
Diabetic retinopathy is classified into two types.
Don’t Miss: How Can I Check If I Have Diabetes
Causes And Symptoms Of Diabetic Retinopathy
Diabetic retinopathy is caused by changes in the tiny blood vessels that supply the retina. These changes occur due to chronically high blood glucose levels. Therefore, people with longstanding diabetes and poorly-controlled blood sugar levels are more likely to develop DR. The condition usually affects both eyes and can occur with both type 1 and type 2 diabetes1.
In the early stages, DR may not cause any symptoms. As the condition progresses, however, symptoms may start to occur. These may include blurred vision, floaters , impaired colour discrimination, dark areas in the visual field, fluctuating vision, and vision loss 1.
Join Forces To Deliver Proper Care

As the number of US patients with diabetes grows, it is important for optometrists to collaborate with PCPs, endocrinologists, and retina specialists on managing these patients disease. This teamwork, combined with effective communication among caregivers and with patients, will enhance the care that they receive.
- 1. Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984 102:520-526.
- 2. American Optometric Association. Evidence-based Clinical Practice Guideline: Eye Care of the Patient With Diabetes Mellitus. www.aoa.org/optometrists/tools-and-resources/evidence-based-optometry/evidence-based-clinical-practice-guidlines/cpg-3–eye-care-of-the-patient-with-diabetes-mellitus. Accessed May 2, 2019.
- 3. Stratton IM, Kohner EM, Aldington SJ, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001 44:156-163.
Read Also: Does Viagra Work For Diabetics
Risk Factors For Dr And Dme
DR and DME share many common risk factors. Incidence-derived risk factors for DR and DME reported in the various cohort studies are summarized in Table . The major and established risk factors have been reviewed extensively before . The most pertinent observations will be highlighted again in this review, with updates from the latest literature. Novel risk factors were also reviewed.
Diagnosis And Treatment Of Diabetic Eye Complications
If you have diabetes and are wondering whether it has affected your eye health, a visit to the optometrist can help you identify any issues and make a plan for managing them. Some of the tests that may be performed include:
- Visual acuity testing with an eye chart
- Tonometry to measure the pressure inside the eye
- Dilated eye exam to examine the optic nerve and retina
- Digital retinal photography
- to capture 3D images of the eye
These tests will show any changes in the retinal blood vessels that indicate damage due to diabetes. If intermediate or advanced stages of DR or DMO are discovered, more frequent dilated eye examinations may be recommended and treatment may be started.
Therapies for DMO include drugs that prevent the growth of abnormal blood vessels. Corticosteroids can help in the short-term, but they can increase the risk of other complications such as glaucoma and cataracts. Laser surgery can also help to slow down the leakage of fluid from the damaged retinal blood vessels. These treatments can be used alone or in combination.
Want to learn more about diabetic retinopathy or diabetic macular oedema? Browse through our educational resource or book an appointment with one of our Specsavers optometrists.
Don’t Miss: How To Test For Diabetes Without Taking Blood